disorder prove, over time, to have been the early presentation of a neurovascular syndrome or, for that matter, a systemic rheumatic disease.
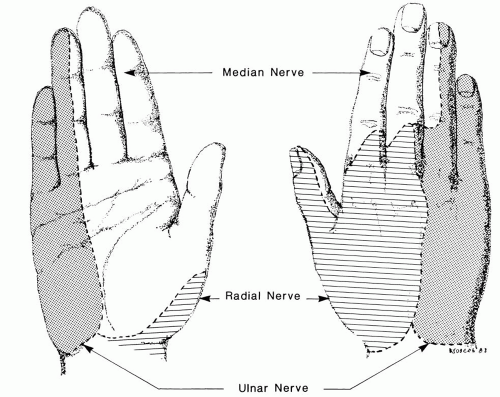
Dysesthesias are characteristically localized to the sensory distribution of the nerve.
Discomfort and paresthesias are more prominent at rest than with usage.
There is greater susceptibility of sensory fibers than motor fibers to the insult.
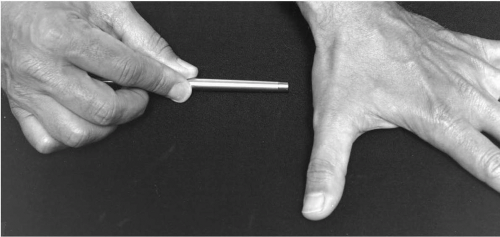
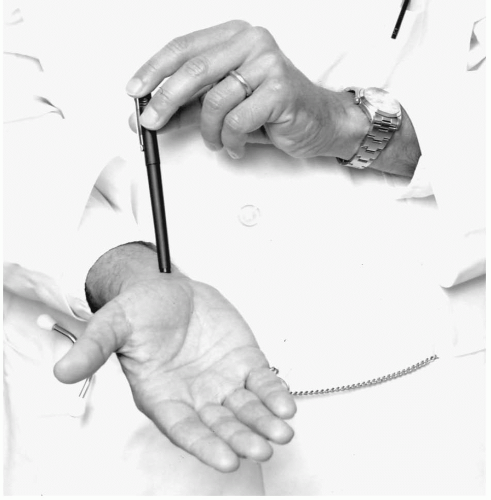
Tinel’s sign is frequently present. This means that percussion of the nerve at the site of entrapment elicits dysesthesias in the sensory distribution of the nerve.
Electrodiagnostic studies provide the gold standard for all entrapment neuropathies.
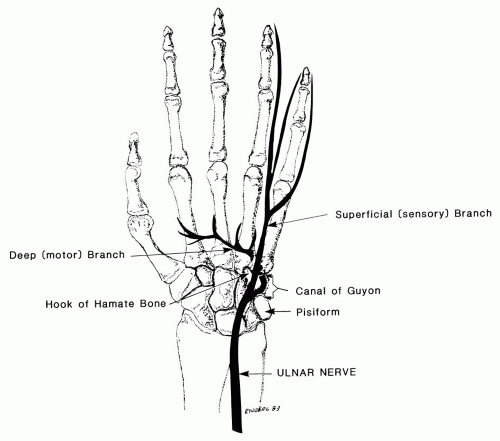
can follow, again in the ulnar distribution. Finally, weakness of ulnar innervated muscles is a prodrome to atrophy. The latter can lead to the classic claw deformity in the hand. However, the clinical presentation of ulnar nerve entrapment is notoriously variable. Insidiously progressive atrophy can occur with little discomfort and even little sensory loss, the so-called tardy ulnar palsy. More typically there is neuritic discomfort.
are commonly used. Nearly all patients experience complete long-term remission without recourse to surgery.7
indicate CTS, yet Tinel’s sign localizes proximally, and later there is compromise in the power of the long finger flexors. The diagnosis is occasionally confirmed electrodiagnostically but with considerable difficulty. CTS is excluded electrodiagnostically. The diagnosis is aided if pronation against resistance leads to symptoms. This is a rare cause of median neuropathy; the last patient I saw with this disorder was a bass player who experienced the symptoms when he played by picking the strings rather than bowing. Treatment is to restrain forceful pronation so that the pronator muscle involutes.
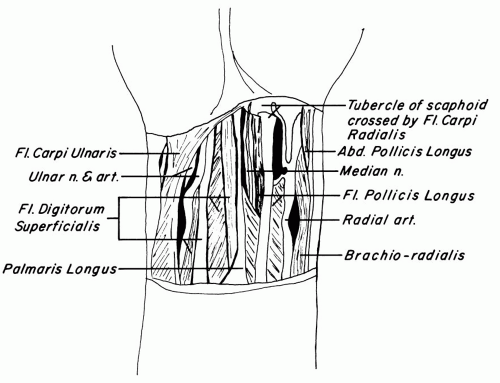
with known predilection to impair median conductivity at the wrist. CTS is well described as a complication of late pregnancy, hypothyroidism, rheumatoid arthritis, amyloidosis, acromegaly, and diabetes. The nerve can be impinged on with fractures of the wrist or intra-articular inflammatory processes such as tuberculosis. The peripheral neuropathic processes associated with diabetes, amyloidosis, and renal failure have some predilection for the median nerve in the tunnel, rendering these patients at greater risk for CTS but less likely to respond to traditional medical or surgical approaches to this entrapment neuropathy. It is not a manifestation of pyridoxine deficiency; prescribing pyridoxine has an unfavorable risk/benefit ratio.10
prototype for an entrapment neuropathy. The initial presentation is of dysesthesias, even lancinating pain, in the radial side of the hand. If the thumb is involved, the discomfort can extend its length; angina seldom passes the interphalangeal joint. Occasionally the discomfort radiates proximally toward the elbow but seldom further. The dysesthetic sensation often awakens the patient, causing the patient to leave the bed and shake his or her hand. There may be a perception of swelling, even of clumsiness early on without objective correlates. However, with progression, weakness in pinch and even atrophy of the abductor pollicis brevis (Fig. 9.4) are apparent. Further denervation leads to more thenar atrophy and overt thumb weakness. Only approximately half the patients manifest Tinel’s or Phalen’s signs (Fig. 9.5). Furthermore, in this classic series, the Mayo clinicians documented impaired conductivity by electrodiagnostic testing approximately half the time. The clinicians were satisfied with their diagnosis without electrodiagnostic testing the rest of the time and even were satisfied with their diagnosis in the 27% of patients whose electrodiagnostic test results were normal.
TABLE 9.1. CLINICAL FEATURES OF THE PATIENTS WITH DIAGNOSES OF CARPAL TUNNEL SYNDROME AT THE MAYO CLINIC BETWEEN 1961 AND 19808 | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 9.2. BRIGHAM AND WOMEN’S HOSPITAL AND HARVARD MEDICAL SCHOOL ANALYSIS OF THE USE OF CLASSIC SIGNS AND SYMPTOMS OF CARPAL TUNNEL SYNDROME IN 110 PATIENTS WITH ARM PAIN WHO WERE REFERRED FOR ELECTRODIAGNOSTIC TESTING17 | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Even with these advances in the performance and interpretation of electrodiagnostic testing, no one should take away the message that no challenges remain to diagnosing CTS or defining its incidence or prevalence.
TABLE 9.3. PERSONAL ATTRIBUTES THAT MUST BE TAKEN INTO ACCOUNT TO DEFINE NORMAL MEDIAN NERVE CONDUCTIVITY | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
a patient, another one or two people must stay alive at home and suffer in silence. This is not likely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree