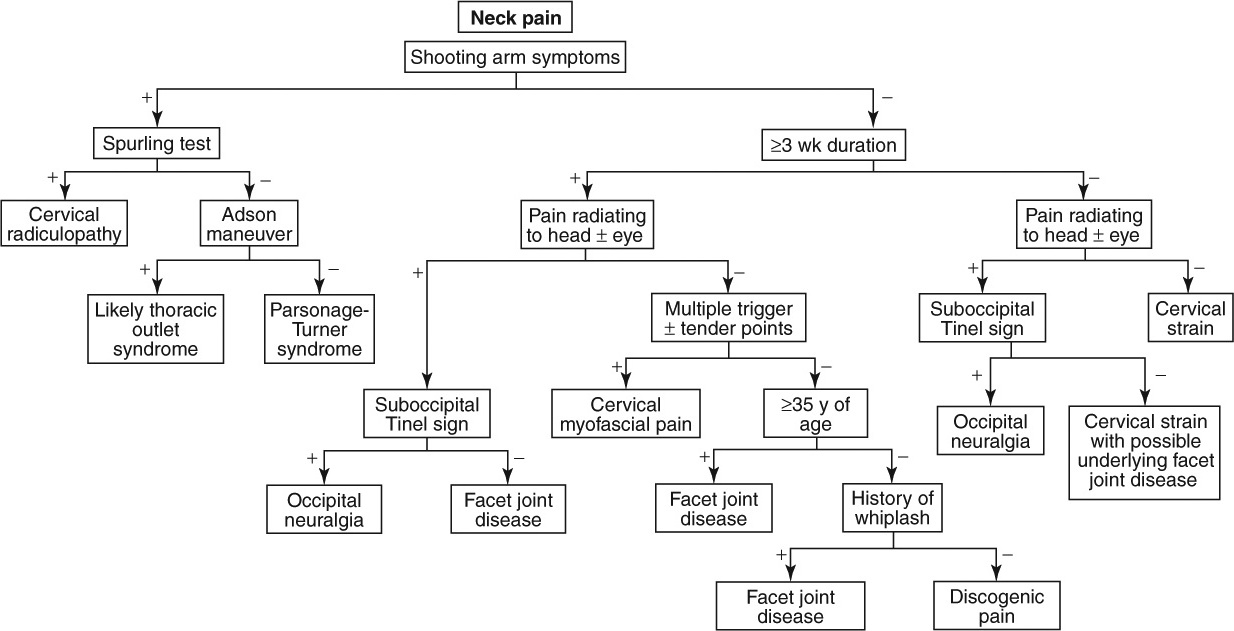
Neck Pain and Shooting Arm Pain
|
Red Flag Signs and Symptoms
Any of these signs and symptoms should prompt urgent evaluation and appropriate intervention:
Fevers
Chills
Recent unintended weight loss
Progressive neurologic symptoms
Change in bowel or bladder function
Significant trauma precipitating symptoms
CERVICAL RADICULITIS/RADICULOPATHY
Background
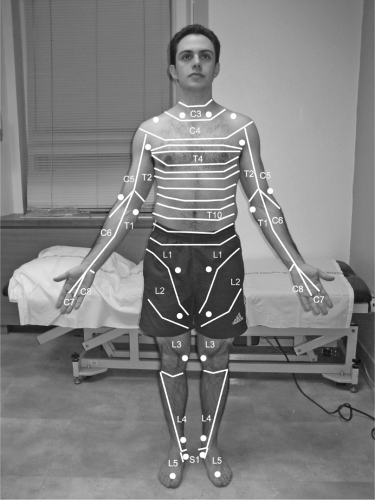
Cervical radiculopathy, as the term is commonly used, is characterized by inflammation and/or compression of the nerve root and/or dorsal root ganglion. The symptoms of cervical radiculopathy typically consist of shooting pain and/or numbness that radiates from the neck into the arm and often into the hand. As opposed to other referral pain patterns, which may be diffuse and vague in distribution, radicular symptoms characteristically follow the sclerotome of the involved nerve root. As such, patients can often trace with two or three fingers the distribution of the symptoms as they radiate down the arm (Fig. 1.1). The character of the pain is typically described as “electric,” “burning,” and/or “sharp.” This contrasts with other referral pain patterns, which may be more “dull” and “achy.” Cervical radiculopathy also may involve weakness of the muscles supplied by the involved nerve root (Table 1.1).
TABLE 1.1 CERVICAL RADICULAR PATTERNS | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In the rare instance that symptoms of a cervical radiculitis/radiculopathy become severe and progressive, or if patients have a sudden change in their bowel or bladder habits (including losing continence), emergent care is necessary and the patient should seek immediate medical attention.
Clinical Presentation
The typical patient presents with several days of neck pain and intermittent shooting, electric pain that radiates in a bandlike fashion down the arm and into the hand. The pain may be positional. Turning the head in the direction of the pain often exacerbates the symptoms. Because of the severity of symptoms, the patient may report having trouble sleeping. The inciting event is typically difficult to identify. However, sometimes, symptoms begin after a traumatic event or exercise, such as after doing a headstand in certain higher-level yoga positions.
Physical Examination
The most common finding on physical examination is a positive Spurling test. In this test, the patient’s head is
passively rotated to the side of the pain and extended. Gentle pressure is then placed at the top of the head, directed toward the feet (Fig. 1.2). This maneuver narrows the foramen, putting pressure on the affected nerve root. It is positive when it reproduces the radicular symptoms into the patient’s arm. If pain is localized to the neck, the test is not positive. Moving the head to the opposite direction (contralateral rotation and extension) often alleviates symptoms because it takes the pressure off the nerve root.
passively rotated to the side of the pain and extended. Gentle pressure is then placed at the top of the head, directed toward the feet (Fig. 1.2). This maneuver narrows the foramen, putting pressure on the affected nerve root. It is positive when it reproduces the radicular symptoms into the patient’s arm. If pain is localized to the neck, the test is not positive. Moving the head to the opposite direction (contralateral rotation and extension) often alleviates symptoms because it takes the pressure off the nerve root.
Sensory deficits may be detected in the distribution of the affected nerve root(s) (Fig. 1.1). Weakness is often subtle but may be detected. Reflexes may also be diminished (Table 1.1).
The Hoffman reflex should be checked (Fig. 1.3). In this test, the middle dorsal finger is “flicked” and if the first or second digit reflexively flexes, the sign is positive and indicates an upper motor neuron problem. The presence of this sign should raise suspicion for a more serious underlying problem such as spinal cord impingement.
Diagnostic Studies
Radiographs should be obtained. These will likely reveal foraminal stenosis, decreased disc height, and spondylosis but will be otherwise normal.
Magnetic resonance imaging (MRI) should be obtained unless symptoms are very mild. MRI may reveal foraminal stenosis from facet hypertrophy (typically in older patients) or a foraminal disc (typically in younger patients).
Electromyelography/nerve conduction studies (EMG/ NCS) are not generally needed unless the diagnosis is in doubt or surgery is being contemplated.
Treatment
Treatment generally begins with physical therapy. Physical therapy addresses postural mechanics and gentle range of motion and strengthening exercises. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to help quiet the inflammation. Ice (or a bag of frozen peas) can be a very good anti-inflammatory agent for this pathology.
If sleep is affected, a muscle relaxant taken at night may be helpful. Some physicians also suggest offering a nerve-stabilizing medication such as gabapentin (e.g., Neurontin) or pregabalin (e.g., Lyrica), which may help the symptoms.
If symptoms are particularly severe, or the patient wants to be aggressive, an oral steroid taper may be appropriate. One should be cautious, however, when considering an oral steroid taper to ensure it is not used until discitis and other inflammatory as well as malignant causes of symptoms have been ruled out. Oral steroid tapers should not be used for these conditions and may worsen the disease. It may be advisable to get a cervical MRI prior to giving oral steroids.
If the patient does not improve after 3 to 4 weeks of the conservative care just described, a fluoroscopically guided epidural steroid injection may be considered. Epidural steroid injections in the cervical spine are generally well tolerated; devastating adverse events have been reported, however, and so these injections should be respected and only done when more conservative measures have failed. They also may be used sooner if the patient’s symptoms are particularly severe and the patient understands the risks. Risks, although rare, include paralysis and death. These injections, like all injections, should only be performed by experienced expert physicians. If the cervical epidural steroid injection is helpful but symptoms persist, a second and possible third injection may be attempted. If the first injection does not help at all, a repeat injection (unless at a different level or
from a different approach—transforaminal versus interlaminar) is unlikely to be useful.
from a different approach—transforaminal versus interlaminar) is unlikely to be useful.
If symptoms persist despite aggressive conservative care, including epidural steroid injections, and an identifiable pathology is identified on the MRI, surgery should be considered. Progressive symptoms or change in bowel or bladder habits represent a potential surgical emergency and should be evaluated emergently.
CERVICAL STRAIN
Background
The muscles and tendons in the neck can be strained because of chronic, repetitive overuse with poor posture and tension or from an acute injury. The medical definitions in this regard are gray. For the purposes of this book, the diagnosis of “cervical strain” is reserved for an acute condition from a relatively minor trauma (e.g., sleeping “wrong” on the neck one night; twisting too quickly to the side) and the diagnosis of “cervical myofascial pain” is reserved for chronic overuse injuries. The distinction is important because the mechanism of injury is different as is the natural history and treatment. Similarly, neck pain following a major trauma such as a motor vehicle accident (whiplash) is a different category of injury as well.
Clinical Presentation
The typical patient presents complaining of having “slept on the pillow wrong” or looked quickly upward and felt a sharp pain in the neck. For most patients, the pain is not particularly severe, but cervical range of motion is restricted because of the pain. Most patients wait a few days or more before coming to the doctor. When they do come, it is because the pain has not improved. The pain is localized and does not radiate




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree