Motion (ROM in degrees) | Muscles | Nerves | Roots |
Shoulder flexion (180) | Anterior deltoid Coracobrachialis | Axillary Musculocutaneous | C5, C6 C6, C7 |
Shoulder extension (45) | Latissimus dorsi Teres major Posterior deltoid | Thoracodorsal Inferior subscapular Axillary | C6, C7, C8 C5, C6, C7 C5, C6 |
Shoulder abduction (180) | Middle deltoid Supraspinatus | Axillary Suprascapular | C5, C6 C5, C6 |
Shoulder adduction (40) | Pectoralis major Latissimus dorsi | Med + lat pectoral Thoracodorsal | C5-T1 C6, C7, C8 |
Shoulder external rotation (90a) | Infraspinatus Teres minor | Suprascapular Axillary | C5, C6 C5, C6 |
Shoulder internal rotation (80a) | Subscapularis Pectoralis major Latissimus dorsi Teres major | Sup + inf subscapular Med + lat pectoral Thoracodorsal Inferior subscapular | C5, C6 C5-T1 C6, C7, C8 C5, C6, C7 |
Shoulder shrug | Trapezius Levator scapulae | Spinal accessory (CN XI) C3, C4 ± dorsal scapular (C5) | |
Elbow flexion (150) | Biceps brachii Brachialis Brachioradialis | Musculocutaneous Musculocutaneous Radial | C5, C6 C5, C6 C5, C6 |
Elbow extension | Triceps brachii | Radial | C6, C7, C8 |
Forearm supination (80) | Supinator Biceps brachii | Posterior interosseous Musculocutaneous | C5, C6, C7 C5, C6 |
Forearm pronation (80) | Pronator teres Pronator quadratus | Median Anterior interosseous | C6, C7 C8, T1 |
Wrist flexion (80) | Flexor carpi radialis Flexor carpi ulnaris | Median Ulnar | C6, C7, C8 C7, C8, T1 |
Wrist extension (70) | Ext carpi rad longus Ext carpi rad brevis Ext carpi ulnaris | Radial Radial Posterior interosseous | C6, C7 C6, C7 C7, C8 |
MCP flexion (90) | Lumbricals Dors + palm interossei | Median, ulnar Ulnar | C8, T1 C8, T1 |
PIP flexion (100) | Flexor digitorum sup Flexor digitorum prof | Median Median, ulnar | C7-T1 C7, C8, T1 |
DIP flexion (90) | Flexor digitorum prof | Median, ulnar | C7, C8, T1 |
MCP, finger extension | Extensor digitorum Extensor indicis Extensor digiti min | Posterior interosseous Posterior interosseous Posterior interosseous | C7, C8 C7, C8 C7, C8 |
Finger abduction (20) | Dorsal interossei Abductor digiti min | Ulnar Ulnar | C8, T1 C8, T1 |
Finger adduction | Palmar interossei | Ulnar | C8, T1 |
Thumb flexion | Flexor pollicis brevis Flexor pollicis longus | Median, ulnar Anterior interosseus | C8, T1 C7, C8, T1 |
Thumb extension | EPB Extensor pollicis longus | Posterior interosseous Posterior interosseous | C7, C8 C7, C8 |
Thumb abduction | Abd pollicis longus Abd pollicis brevis | Posterior interosseous Median | C7, C8 C8, T1 |
Thumb adduction | Adductor pollicis | Ulnar | C8, T1 |
Hip flexion (120) | Iliopsoas | Femoral | L2, L3, L4 |
Hip extension (30) | Gluteus maximus | Inferior gluteal | L5, S1, S2 |
Hip abduction (40) | Gluteus medius Gluteus minimus | Superior gluteal Superior gluteal | L4, L5, S1 L4, L5, S1 |
Hip adduction (20) | Adductor longus Adductor magnus | Obturator Obturator, sciatic | L2, L3, L4 L2, L3, L4, L5, S1 |
Hip external rotation (45) | Obturator int + ext Quadratus femoris Piriformis Sup + inf gemelli Glut max (postfibers) | n. obt int, obturator n. quadratus femoris n. piriformis n. obt int, n. quad fem Inferior gluteal | L3-S2 L2, L3, L4 S1, S2 L4-S2 L5, S1, S2 |
Hip internal rotation (45) | Gluteus minimus Gluteus medius Tensor fasciae latae | Superior gluteal Superior gluteal Superior gluteal | L4, L5, S1 L4, L5, S1 L4, L5, S1 |
Knee flexion (135) | Semitendinosus Semimembranosus Biceps femoris | Tibial div. of sciatic Tibial div. of sciatic Tib + per div. sciatic | L5, S1, S2 L4, L5-S2 L5, S1, S2 |
Knee extension | Quadriceps femoris | Femoral | L2, L3, L4 |
Ankle dorsiflexion (20) | Tibialis anterior | Deep peroneal | L4, L5, S1 |
Ankle plantarflexion (45) | Gastrocnemius Soleus | Tibial Tibial | L5, S1, S2 L5, S1, S2 |
Ankle inversion (35) | Tibialis posterior | Tibial | L4, L5, S1 |
Ankle eversion (25) | Peroneus longus Peroneus brevis | Superficial peroneal Superficial peroneal | L4, L5, S1 L4, L5, S1 |
Toe extension | Extensor hallucis longus Extensor digitorum brevis | Deep peroneal Deep peroneal | L4, L5, S1 L5, S1 |
a Shoulder IR/ER varies with elevation of the arm. | |||
CN, cranial nerve; IR, internal rotation; PIP, proximal interphalangeal. | |||
For ROM , 0° is anatomic position. Please note that there is no absolute consensus regarding which muscles are the primary movers of joints or for the root innervations of muscles. | |||
anatomic deformity. A type II injury (see Fig. 7-1) involves an AC tear and CC ligament sprain, but the CC interspace is intact. Treatment for type I or II injuries includes an arm sling, ice, analgesics, and progressive ROM exercises. An unstable type II injury may require arm sling use for 2 to 4 weeks. Sports activities can be resumed when full painless ROM is achieved and deltoid strength is near-baseline. Type III to VI lesions involve rupture of the AC and CC ligaments with varying displacements of the clavicle. These require orthopedic consultation for potential ORIF, although many separations may be followed conservatively with several weeks of sling-and-swathe immobilization, followed by long-term therapy.
 Figure 7-1 Type II injury. Adapted from Rockwood CA, ed. Rockwood & Green’s Fractures in Adults. 3rd ed. Philadelphia, PA: JB Lippincott; 1988. |
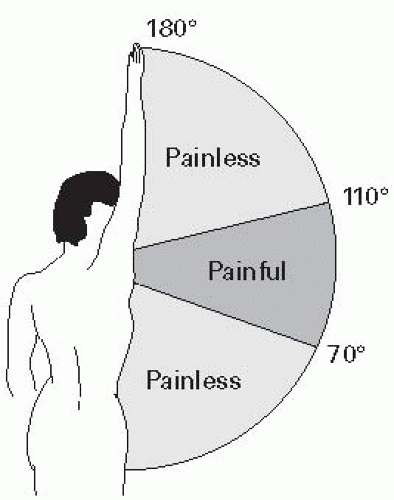
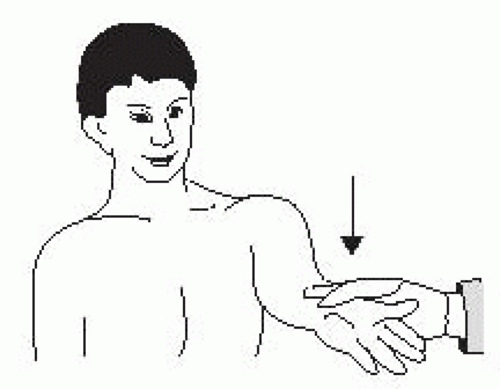
scapular plane. In the drop arm test, the arm is passively elevated to 90° in abduction and the patient is asked to hold the arm in position and then slowly lower the arm to the side. The inability to slowly lower the arm or having severe pain when attempting to do so may be indicative of a severe or complete tear of the rotator cuff pathology.
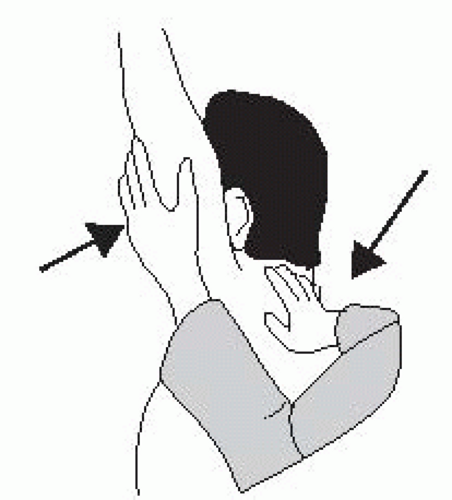
Stimson technique. This method is performed with the patient supine and longitudinal traction is applied as the shoulder is slowly abducted.4 Neurovascular status should be checked before and after attempted relocation.
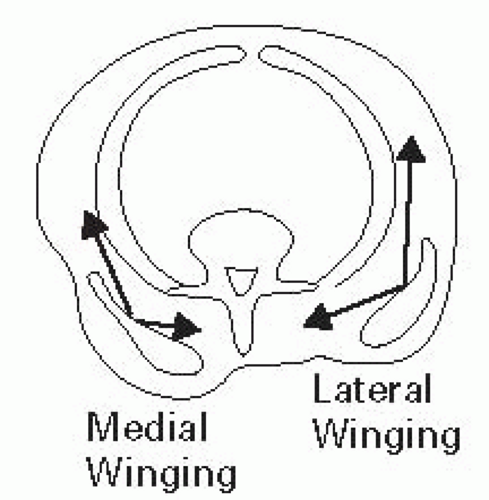
program, which may include the use of modalities such as heat and postactivity icing. Local corticosteroid injection may be used in refractory cases and US guidance may help increase your accuracy of performing injections into the tendon sheath.6 Scapular Winging – Medial scapular winging (Fig. 7-6) is caused by weakness of the serratus anterior (long thoracic nerve). It is elicited by having the patient push against a wall and using resisted forward flexion or resisted scapular protraction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree