Abstract
Introduction
Muscle weakness is a common consequence of stroke and can result in a decrease in physical activity. Changes in gait performance can be observed, especially a reduction in gait speed, and increased gait asymmetry, and energy cost is also reported.
Objective
The aim was to determine whether strengthening of the lower limbs can improve strength, balance and walking abilities in patients with chronic stroke.
Method
Five databases (Pubmed, Cinhal, Cochrane, Web of Science, Embase) were searched to identify eligible studies. Randomized controlled trials were included and the risk of bias was evaluated for each study. Pooled standardized mean differences were calculated using a random effects model. The PRISMA statement was followed to increase clarity of reporting.
Results
Ten studies, including 355 patients, reporting on the subject of progressive resistance training, specific task training, functional electrical stimulation and aerobic cycling at high-intensity were analysed. These interventions showed a statistically significant effect on strength and the Timed Up-and-Go test, and a non-significant effect on walking and the Berg Balance Scale.
Conclusion
Progressive resistance training seemed to be the most effective treatment to improve strength. When it is appropriately targeted, it significantly improves strength.
1
Introduction
1.1
Background
In industrialised countries, stroke is the most frequent cause of disability among adults. The death rate following stroke is set to decrease as a result of better care provision as soon as the problem occurs. It can therefore be expected that the number of people surviving with a disability following a stroke is liable to increase . In addition, the incidence of stroke has increased dramatically among younger subjects, with over 20% of people affected being under the age of 65 .
After a stroke, hemiparesis is a serious motor impairment, affecting 65% of stroke victims .
Muscular weakness is a conspicuous symptom and appears as one of the main factors slowing the recovery of normal physical abilities among patients . It appears in several forms, the most significant being paresis of the body on the contra-lateral side to the cerebral lesion , although correlation has also been observed between strength deficits on the ipsilesional side and walking speed . Paresis is defined as an alteration in the ability to generate a normal level of muscle strength . This results in abnormal posture and stretching reflexes, and a loss of voluntary movement .
Muscle weakness can lead to immobilisation or to markedly reduced physical activity . In the study by Hsu et al. , the authors show how the walking performances of stroke patients, in comparison with healthy subjects, is characterised by reduced walking speed and residual left-right spatial and temporal asymmetry. According to these authors, the strength of the hip flexor muscles and the knee extensor muscles of the hemiplegic limb are the most important factors determining comfortable or fast walking speed. However, the spasticity of the ankle plantar flexors also appears as an important factor in this asymmetry. Plantar flexor muscles also affect walking speed . Other characteristics are observed in stroke patients on the ten-metre walking test, such as a decrease in step length and in swing phase speed of the hemiplegic limb, longer single support time on the healthy side and prolonged double support phase (time of transfer from hemiplegic to healthy side). It has also been shown that the pathological gait of a hemiplegic subject may have double energy cost compared to that of a healthy subject .
1.2
Intervention
It should be noted that since the 1990s there have been studies showing that neither activities requiring effort nor strength training increase spasticity among stroke patients , this having previously been a subject of controversy. Given this absence of negative effects, and the positive consequences reported, these treatments are now included in post-stroke rehabilitation programmes .
In case of marked muscle weakness, strengthening exercises are required to alleviate the effects of atrophy , but it seems that the gain in strength results mainly from an adaptation of the nerve tissues .
Muscle strengthening uses the principle of maximum strength (1 RM) defined by DeLorme in 1948 . For healthy subjects, this consists in one to three series of eight to twelve repetitions at 60–80% of the 1 RM, twice or three times a week . For post-stroke subjects, some authors prescribe exercising entailing more numerous repetitions, between 10 and 15, but with a reduced workload (percentage of 1 RM). Different authors have assessed gains in strength for workloads mainly between 50% and 80%, but it seems that a workload of only 40% also has positive effects .
Given the different methods of muscle strengthening available, we provide below a description of certain types of exercise used among patients in rehabilitation after a stroke.
1.2.1
Progressive resistance training (PRT)
Muscle strengthening by progressive resistance exercises is based on a workload of 70–80% maximum strength (1 RM) or more . This means that 1 RM should be measured regularly so as to adapt the workload to the constant improvements in the patient by way of isokinetic devices , manual dynamometers or manual testing . There is no consensus to date on the duration or the frequency of treatments. However, it seems that treatment lasting at least sixteen hours provides an improvement in functional capacities .
1.2.2
Task-specific training (TST)
Functional, i.e. task-specific training has shown its efficacy in improving walking when delivered intensively In addition, it should always be integrated in therapies, since functional improvement is their final purpose .
For instance, standing up from a chair (known as chair-rise) is a complex motor task that requires adequate postural control and dynamic movement. The movement mainly requires muscular strength, coordination and balance. The main muscles involved in getting up from a chair are the quadriceps and hamstring muscles . When the movement is performed rapidly, it shows better symmetry in standing position, and improvement in postural stability and in directional control .
1.2.3
Intensive aerobic exercising
It has been demonstrated that the combination of muscle strengthening and aerobic exercising have a positive effect among elderly subjects. In addition, as a result of this type of exercising, an improvement is observed in the recruitment of motor units and in walking speed .
The intensity of exercising can be calculated with the Karvonen formula, which uses the heart rate reserve (HRR) to define the exercise heart rate. Among stroke patients, the target intensity of aerobic exercising is 50 to 70% of the HRR .
1.2.4
Functional electrical stimulation (FES)
Functional electrical stimulation is a tool that uses the transmission of electrical signals to the muscle . This type of training mobilises more muscular fibres and thus increases their metabolic activity .
Certain articles report on electrical stimulation combined with cycling . This appears more beneficial for patients than manual guidance with FES when walking. This technique enables the patient to re-learn a correct, complete movement and to increase the sensory feedback from the movement as a result of the bilateral cycling motion .
1.3
Measures
Two walking tests recur regularly in the literature. The Six Minutes Walking test (6MWT) has exhibited a significant, positive relationship with strength of the lower limbs . Among stroke patients, a difference of 50 metres between two tests on the same patient is required to conclude to substantial improvement . The second widely-used test is the 10-Metre Walking test (10MWT) which assesses fast walking . For this test, a substantial improvement corresponds to a difference of 0.10 metres a second .
There are different ways of measuring strength among stroke patients. One of them consists in calculating maximum strength (1 RM) . In untrained subjects, the maximum load can be calculated using a formula such as that proposed by Brzycki .
The Manual Muscular test (MMT), which is applied using the Medical Research Council scale (MRC) has been validated for use among stroke patients .
Regarding the manual dynamometer, reliability and precision seem good, provided the test is applied by one and the same investigator .
The Timed Up-and-Go (TUG) is a quantitative test enabling the assessment of balance, fall risk and walking . The minimum detectable change is 23% . A fairly similar test is the five times sit-to-stand test. The minimum detectable change for this test is 3.6 seconds. These two tests have excellent reliability among stroke patients .
The Berge Balance Scale (BBS) also measures functional activity capacities, testing balance in 14 tasks. Its validity and reliability have been repeatedly established . This test carries a total of 54 points. A significant change is observed from 5.8 points difference with the same tests taken previously .
2
Methods
2.1
Inclusion criteria for studies in this review
The aim of this work was to analyse the effect of muscle strengthening on walking, strength and balance among chronic hemiplegic patients following a stroke, and to observe results in the long-term. A systematic review of the literature was performed, followed by a meta-analysis.
The inclusion criteria targeted solely randomised controlled trials (RCTs) published up to January 20th 2014 in French, English or German. RCT follow-up studies were also considered. The participants were to be adults (over 18 yrs) following stroke and presenting hemiparesis. They were to be in chronic post-stroke phase. On account of disagreement on this subject, only studies including patients 3 months post-stroke or more were considered, or studies that stipulated that they included patients in subacute and chronic phase.
In the search, we included strengthening methods aiming to improve motor function in the lower limbs via specific, intensive exercises for particular muscle groups.
The exclusion criteria were the use of robotic devices, since in most rehabilitation centres they cannot be used on account of their cost, and the use of medication. Articles concerning the upper limbs and trunk were also excluded.
2.1.1
Outcomes and measures
To measure the effect of strengthening on walking, two tests were considered, the 6-Minute Walking test (6MWT) and the 10-Metre Walking test (10MWT). Then, to observe the effects of muscle strengthening on strength in the hemiplegic limb, we divided up the results according to the muscles tested. Priority was given to isokinetic tests, followed by manual dynamometers and MMT. As maximum strength was targeted, excentric tests took priority .
We also looked at balance in the course of functional activities as measured by the Berg Balance Scale (BBS) and the Timed Up-and-Go test (TUG). The five times sit-to-stand test was included with the TUG in our analyses.
2.2
Search strategy
Our literature search was performed on the databases Pubmed, Cochrane, Cinhal, Web of Science et Embase. The following search strategy was implemented: (stroke OR “cerebrovascular accident” OR “cerebrovascular disease” OR CVA OR hemipleg* OR hemipar*) AND (strength* OR power OR force OR “muscle performance” OR “resistance training” OR “task oriented training” OR “task specific training” OR FES OR “functional electrical stimulation”) AND (gait OR walk OR locomotion OR ambulation OR 6MWT OR “Berg balance scale” OR BBS OR “timed up-and-go” OR TUG OR “Barthel index” OR strength OR 1 RM OR isokinetic OR 10MWT). The last search on these databases was on January 20th 2014.
Methodological filters were combined with this search strategy so as to target clinical studies as described by Wong et al. for Embase and Web of Science. For PubMed and Cinal, we used the “clinical queries” proposed by Haynes .
2.3
Data collection and analysis
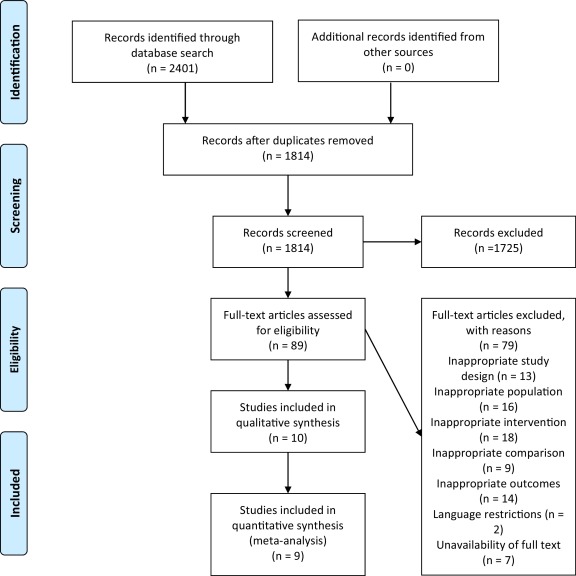
After completion of the electronic searches, articles were sorted in three distinct steps, first individually by two reviewers , and then disagreements were solved conjointly. In the first stage, duplicates were removed. The second stage consisted in perusing titles and abstracts for inclusion and exclusion criteria. Finally, the full articles were perused, and unsuitable studies were removed.
The evaluation of risk of bias was performed using the Cochrane Collaboration Risk of Bias (ROB) tool . The results are presented in a table with different colours. Green indicates low risk, red indicates high risk, and yellow indicates that the risk of bias could not be estimated for lack of information.
Means and standard deviations for the different groups were then extracted for continuous measures, using the result at the end of the intervention for all outcome measures. The results of follow-up studies were extracted for walking measures, strength and TUG. For the meta-analyses, the results of continuous measures were calculated from the standardised mean difference (SMD) and the corresponding 95% confidence interval. A randomised effect model was used for all the meta-analyses. The value of the effect was established according to the method described by Cohen (where 0.8 is a marked effect, 0.5 a moderate effect, and 0.2 a small effect).
The I 2 index was used to classify statistical heterogeneity. The guide by Higgins and Green was followed to interpret the I 2 statistics (from 75% to 100% indicates considerable heterogeneity, 50 to 90% substantial heterogeneity, 30 to 60% moderate heterogeneity and 0–40% fairly low heterogeneity). All the statistical analyses were performed on Review Manager 5.2 software. To enhance reporting procedures, the PRISMA guidelines were used .
2
Methods
2.1
Inclusion criteria for studies in this review
The aim of this work was to analyse the effect of muscle strengthening on walking, strength and balance among chronic hemiplegic patients following a stroke, and to observe results in the long-term. A systematic review of the literature was performed, followed by a meta-analysis.
The inclusion criteria targeted solely randomised controlled trials (RCTs) published up to January 20th 2014 in French, English or German. RCT follow-up studies were also considered. The participants were to be adults (over 18 yrs) following stroke and presenting hemiparesis. They were to be in chronic post-stroke phase. On account of disagreement on this subject, only studies including patients 3 months post-stroke or more were considered, or studies that stipulated that they included patients in subacute and chronic phase.
In the search, we included strengthening methods aiming to improve motor function in the lower limbs via specific, intensive exercises for particular muscle groups.
The exclusion criteria were the use of robotic devices, since in most rehabilitation centres they cannot be used on account of their cost, and the use of medication. Articles concerning the upper limbs and trunk were also excluded.
2.1.1
Outcomes and measures
To measure the effect of strengthening on walking, two tests were considered, the 6-Minute Walking test (6MWT) and the 10-Metre Walking test (10MWT). Then, to observe the effects of muscle strengthening on strength in the hemiplegic limb, we divided up the results according to the muscles tested. Priority was given to isokinetic tests, followed by manual dynamometers and MMT. As maximum strength was targeted, excentric tests took priority .
We also looked at balance in the course of functional activities as measured by the Berg Balance Scale (BBS) and the Timed Up-and-Go test (TUG). The five times sit-to-stand test was included with the TUG in our analyses.
2.2
Search strategy
Our literature search was performed on the databases Pubmed, Cochrane, Cinhal, Web of Science et Embase. The following search strategy was implemented: (stroke OR “cerebrovascular accident” OR “cerebrovascular disease” OR CVA OR hemipleg* OR hemipar*) AND (strength* OR power OR force OR “muscle performance” OR “resistance training” OR “task oriented training” OR “task specific training” OR FES OR “functional electrical stimulation”) AND (gait OR walk OR locomotion OR ambulation OR 6MWT OR “Berg balance scale” OR BBS OR “timed up-and-go” OR TUG OR “Barthel index” OR strength OR 1 RM OR isokinetic OR 10MWT). The last search on these databases was on January 20th 2014.
Methodological filters were combined with this search strategy so as to target clinical studies as described by Wong et al. for Embase and Web of Science. For PubMed and Cinal, we used the “clinical queries” proposed by Haynes .
2.3
Data collection and analysis
After completion of the electronic searches, articles were sorted in three distinct steps, first individually by two reviewers , and then disagreements were solved conjointly. In the first stage, duplicates were removed. The second stage consisted in perusing titles and abstracts for inclusion and exclusion criteria. Finally, the full articles were perused, and unsuitable studies were removed.
The evaluation of risk of bias was performed using the Cochrane Collaboration Risk of Bias (ROB) tool . The results are presented in a table with different colours. Green indicates low risk, red indicates high risk, and yellow indicates that the risk of bias could not be estimated for lack of information.
Means and standard deviations for the different groups were then extracted for continuous measures, using the result at the end of the intervention for all outcome measures. The results of follow-up studies were extracted for walking measures, strength and TUG. For the meta-analyses, the results of continuous measures were calculated from the standardised mean difference (SMD) and the corresponding 95% confidence interval. A randomised effect model was used for all the meta-analyses. The value of the effect was established according to the method described by Cohen (where 0.8 is a marked effect, 0.5 a moderate effect, and 0.2 a small effect).
The I 2 index was used to classify statistical heterogeneity. The guide by Higgins and Green was followed to interpret the I 2 statistics (from 75% to 100% indicates considerable heterogeneity, 50 to 90% substantial heterogeneity, 30 to 60% moderate heterogeneity and 0–40% fairly low heterogeneity). All the statistical analyses were performed on Review Manager 5.2 software. To enhance reporting procedures, the PRISMA guidelines were used .
3
Results
3.1.1
Studies included
In all, 2401 articles were identified according to the above search procedure ( Fig. 1 ). Of these, 587 were duplicates, 1725 were excluded on title and abstract, and 79 on full-text perusal. Finally, the 10 studies meeting the inclusion criteria were selected for the systematic review. A critical overview of the data in each study is provided in Table 1 .
| Type | Study | Population | Intervention | Comparison | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age (SD) | Time Post-Stroke (SD) | Description | Duration | Frequency Length | Intensity | |||||||
| I | C | I | C | I | C | ||||||||
| PRT | Akbari et al. (2006) | 17 | 17 | 49.3 (7.1) | 48.8 (3) | 34.5 (26.37) months | 35.3 (27.5) months | Concentric isotonic muscle strengthening (Flex-Ext-Abd Hip; Flex-Ext Knee; DE-PF) Functional exercises, balance | 4 weeks 12 sess. | 3×/week 3 h | 70% 1 RM | Same exercises without muscle strengthening | Isometric strength (dynamometer) flex + ext + abd H, flex + ext K, DE + PF |
| Byun et al. (2011) | 15 | 15 | 59.1 (10.2) | 58.7 (13.8) | 9.4 (3.7) months | 9.9 (5.4) months | Strength on “sliding rehabilitation machine” + Bobath | 2 weeks 10 sess. | 5×/week 30 min | Conventional training based on Bobath concept | 6MWT, TUGT, BBS, MMT (Knie) | ||
| Flansbjer et al. (2008) | 15 | 9 | 61 (5) | 60 (5) | 18.9 (7.9) months | 20 (11.6) months | Strengthening on Leg Extension/Curl Rehab machine Passive Stretching of Knee extensors + flexors | 10 weeks 20 sess. | 2×/week 90 min (PRT 6 min) | 5 rep.25% 1 RM 2 × 6–8rep. 80%1 RM | ADL and other training (not PRT) | Dynamic strength K flex + ext, isokinetic strength K flex + ext, TUG, 6MWT, 10MWT | |
| Flansbjer et al. (2012) | 11 | 7 | Follow-up after 4 years. For baseline results, see Flansbjer et al. (2008) | Dynamic strength K flex + ext, isokinetic strength k flex + ext, TUG, 6MWT, 10MWT | |||||||||
| Lee et al. (2008) | 24 | 24 | Gr1: 60.5 (10.6) | Gr3: 67.2 (10.6) | Gr1: 63.2 (40.5) | Gr3: 52.4 (2.2) | Gr1: Strengthening on pneumatic resistance equipment ext H + K unilateral; abd-ext-flex K; FP; ED | 10–12 30 sess. | 3×/week 60 min | PRT 50%–80% 1 RM Active cycling: 50%Vo2max | Gr3 bilateral: exercises without resistance + active cycling | 6MWT, 10MWT | |
| Lee et al. (2010) | Gr2: 62.9 (9.3) | Gr4: 65.3 (6) | Gr2: 44.2 (63.9) month | Gr4: 65.8 (42.3) months | + Active cycling Gr2: same as Gr1 but passive cycling (motorised) | Gr4: like Gr3, but passive cycling | Strength dynamic PF + DE + flex k + ext k + ext H, isometric abd H | ||||||
| Ouellette et al. (2004) | 21 | 21 | 65.8 (2.5) | 66.1 (2.1) | 31.8 (3.3) months | 25.6 (4) months | Leg-Press bilateral and Ext k + PF + DE unilateral | 12 weeks 36 sess. | 3×/week | 3 sets of 8–10 × 70% 1 RM | ROM bilateral and upper body exercises | 1 RM, 6MWT, stand up, 10MWT | |
| TST | Tung et al. (2010) | 16 | 16 | 51 (12.1) | 52.7 (14.1) | 26.9 (16) months | 12.8 (12.3) months | Sit-to-stand + global Physio (balance, walking, leg strengthening) | 4 week 12 sess. | 3×/week 15 min Strength + 30 min global physio | Global physio (balance, walk, leg strengthening) | BBS, isometric strength ext H + k + PF (dynamometer) | |
| Aerobic | Jin et al. (2012) | 68 | 65 | 57 (6) | 56 (7) | 18 (5.2) months | 17.9 (4.8) months | Aerobic cycling exercise training with additional weight on paretic side Stretching and balance | 8 weeks 40 sess. | 5×/week 40 min | 3% max body weight (hemi-side) 50–70% HRR | Low intensity walking Stretching and balance | 6MWT, excentric strength ext k, BBS |
| FES | Janssen et al. (2008) | 6 | 6 | 54.2 (10.7) | 55.3 (10.4) | 12.3 (5.4) months | 18.3 (9.9) months | ES-LCE | 6 weeks 12 sess. | 2×/week 25–30 min | LCE | Isometric strength ext K, 6MWT, BBS | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






