1
Introduction
Approximately, 1.4 million traumatic brain injuries occur each year in the United States. Among these incidents, 1.1 million result in emergency department visits, 235,000 result in hospitalizations and 50,000 result in death. This does not include an additional estimated 200,000 who are treated in outpatient settings, nor those treated at military facilities both domestic and abroad . Decompressive craniectomy (DC) is frequently used for the treatment of medically refractory intracranial hypertension for patients with severe traumatic brain injury (TBI) . Additionally, DC has been found to reduce mortality rates and improve outcomes in patients with malignant middle cerebral artery infarction, which accounts for 10% of stroke patients .
The syndrome of the trephined (ST), also known as the “sinking skin flap syndrome”, is a disorder of delayed neurological deterioration . By convention, ST refers to the development of those symptoms that are reversible after cranioplasty . This is a complication that occurs in patients with large cranial defects following a DC. Related clinical deterioration occurs weeks to months after the surgery. The symptomatology and clinical signs can include: focal neurological deficits, aphasia, headache, dizziness, lethargy, irritability, inattention, memory problems, depression, anxiety, mood swings, behavioral disturbances, seizures, mutism, worsening hemiplegia, hemi-neglect, and diabetes insipidus As these symptoms are non-specific, early diagnosis is difficult to establish, which can lead to significant neurological decline.
2
Case description
A 21-year-old male bicyclist was brought to the emergency department after being struck by a car. Upon presentation, the patient had a Glasgow Coma Scale (GCS) score of 11, a left hemotympanum, a fixed and dilated left pupil, and flaccid paralysis of the right upper extremity (RUE). The patient was sedated and intubated for airway protection and agitation management. Initial non-contrast head computed tomography (NCHCT) revealed a left epidural and subdural hematoma, diffuse subarachnoid and punctate intra-parenchymal hemorrhages, and a left temporal bone fracture. The patient required an emergent, left-sided DC to relieve his high intracranial pressure (ICP). After medical stabilization in the intensive care unit (ICU) and, subsequently, in an acute medical/surgical ward, the patient was transferred to an acute TBI rehabilitation unit.
His initial exam on the rehabilitation service revealed a large left craniectomy defect with a sunken skin flap. Motor testing revealed 3/5 strength in the left upper extremity (LUE) and flaccid paralysis in the RUE with spasticity noted at the elbow. He had poor sitting and standing balance. He had poor attention and inconsistently followed one-step commands with findings of motor apraxia, fluent aphasia, severe dysarthria, right unilateral body and spatial neglect, and asomatognosia. He required total assistance for all functional mobility and activities of daily living (ADLs).
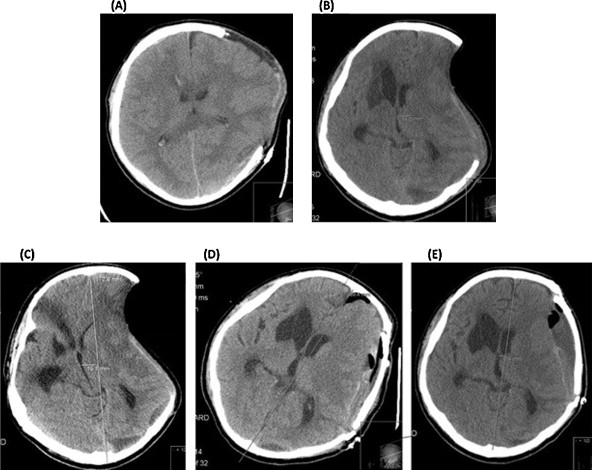
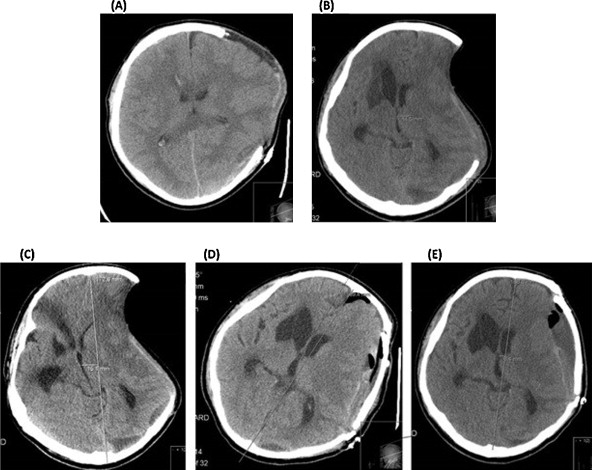
Initially, he made modest but significant functional gains both cognitively and physically. He became able to ambulate on the unit with minimal assistance and perform ADLs with moderate to maximum assistance. He began to verbally communicate and interact with his environment and followed simple commands. He had minimal improvement in RUE strength and tone continued to fluctuate. About three weeks into his admission, he reached a functional plateau. Over the next month, he functionally declined cognitively and physically, developing mutism, requiring greater assistance with ADLs, and returned to use of a wheelchair for mobility. Follow-up imaging and medical work-up revealed no clear findings to explain his decline or lack of progression, but did reveal a sunken craniectomy defect and associated shift in brain parenchyma. After review and discussion with neurosurgery and the patient’s family, the decision was made to proceed with a cranioplasty to improve his clinical status and functional recovery. Non-contrast head CT scans before and after the cranioplasty procedure are shown in Fig. 1 .
Following the cranioplasty and medical stabilization, the patient was re-admitted to the rehabilitation service. The patient demonstrated immediate improvement. He had improved functional mobility, tone, strength, attention, awareness, memory, speech, social interaction, and emotional range. He began to communicate verbally and follow commands. He ambulated 1000 feet and negotiated 20 steps with minimal assistance to supervision. His AROM in both upper extremities were within functional limits. He was able to perform transfers at a contact guard to supervision level, ambulate with supervision, and perform activities of daily living at a supervision to moderate assist level. After a 3-month course of rehabilitation, he was discharged home with his family.
2
Case description
A 21-year-old male bicyclist was brought to the emergency department after being struck by a car. Upon presentation, the patient had a Glasgow Coma Scale (GCS) score of 11, a left hemotympanum, a fixed and dilated left pupil, and flaccid paralysis of the right upper extremity (RUE). The patient was sedated and intubated for airway protection and agitation management. Initial non-contrast head computed tomography (NCHCT) revealed a left epidural and subdural hematoma, diffuse subarachnoid and punctate intra-parenchymal hemorrhages, and a left temporal bone fracture. The patient required an emergent, left-sided DC to relieve his high intracranial pressure (ICP). After medical stabilization in the intensive care unit (ICU) and, subsequently, in an acute medical/surgical ward, the patient was transferred to an acute TBI rehabilitation unit.
His initial exam on the rehabilitation service revealed a large left craniectomy defect with a sunken skin flap. Motor testing revealed 3/5 strength in the left upper extremity (LUE) and flaccid paralysis in the RUE with spasticity noted at the elbow. He had poor sitting and standing balance. He had poor attention and inconsistently followed one-step commands with findings of motor apraxia, fluent aphasia, severe dysarthria, right unilateral body and spatial neglect, and asomatognosia. He required total assistance for all functional mobility and activities of daily living (ADLs).
Initially, he made modest but significant functional gains both cognitively and physically. He became able to ambulate on the unit with minimal assistance and perform ADLs with moderate to maximum assistance. He began to verbally communicate and interact with his environment and followed simple commands. He had minimal improvement in RUE strength and tone continued to fluctuate. About three weeks into his admission, he reached a functional plateau. Over the next month, he functionally declined cognitively and physically, developing mutism, requiring greater assistance with ADLs, and returned to use of a wheelchair for mobility. Follow-up imaging and medical work-up revealed no clear findings to explain his decline or lack of progression, but did reveal a sunken craniectomy defect and associated shift in brain parenchyma. After review and discussion with neurosurgery and the patient’s family, the decision was made to proceed with a cranioplasty to improve his clinical status and functional recovery. Non-contrast head CT scans before and after the cranioplasty procedure are shown in Fig. 1 .