Abstract
Objective
To compare the effects of a standardized supervised physical therapy versus a controlled home-based programs on the rate of shoulder motion and functional recovery after arthroscopic anterior shoulder stabilization.
Methods
Twenty-seven patients (18–35 years) underwent arthroscopic anterior shoulder stabilization. Patients were randomized into two groups. A supervised group ( n = 14) received a rehabilitation program, 3 sessions/week for 24 weeks and a controlled home treated group ( n = 13) who followed a home-based program for same period. Range of motion (ROM) of the shoulder was assessed 4 times after each phase of rehabilitation and function was assessed after the 3rd and 4th phase of rehabilitation.
Results
Both groups achieved a significant progressive increase in all shoulder motions throughout the study period. Patients in the supervised group achieved 92.6% and 94.2% of the contralateral side in abduction and forward elevation respectively. The controlled home-based group achieved 87.1% and 94.7% of abduction and forward elevation respectively. For external rotation, the percentage ROM achieved was 81.1% for the supervised group and 76.4% for the controlled home-based group. For function assessment, the two groups showed a significant improvement. However, the two groups were not significantly different from each other in all measured variables.
Conclusion
A controlled home-based physical therapy program is as effective as a supervised program in increasing shoulder range of motion and function after arthroscopic anterior shoulder stabilization.
Résumé
Objectif
Comparer les effets d’un programme standardisé de rééducation supervisée à ceux d’un programme supervisé à domicile, sur la récupération de la fonction et de la mobilité de l’épaule après une stabilisation antérieure de l’épaule sous arthroscopie.
Méthodes
Vingt-sept patients (âgés de 18 à 35 ans) ont bénéficié d’une stabilisation antérieure de l’épaule sous arthroscopie. Les patients ont été randomisés en deux groupes. Un groupe supervisé ( n = 14) a bénéficié d’un programme de rééducation comportant 3 séances/semaine pendant 24 semaines et un groupe traité à domicile et ( n = 13) qui a suivi un programme supervisé à domicile de même durée. La mobilité de l’épaule a été mesurée à quatre reprises.
Résultats
Les deux groupes ont amélioré progressivement de façon significative toutes les mobilités de l’épaule au cours de la période d’étude. Les patients du groupe supervisé ont obtenu respectivement 92 % et 94,2 % de mobilité en abduction et élévation antérieure, par rapport au côté controlatéral. Le groupe à domicile contrôlé a recouvré respectivement 87,1 % et 94,7 % de mobilité en abduction et élévation antérieure. Concernant la rotation externe, la mobilité atteignait 81,1 % dans le groupe supervisé et 76,4 % dans le groupe à domicile. En ce qui concerne l’évaluation fonctionnelle, une amélioration significative a été observée dans les deux groupes. Cependant, aucune différence significative n’a été observée entre les deux groupes pour aucune des variables évaluées.
Conclusion
Un programme de rééducation réalisé à domicile et contrôlé est aussi efficace qu’un programme supervisé dans l’amélioration de la mobilité et de la fonction de l’épaule après une stabilisation antérieure de l’épaule sous arthroscopie.
1
English version
1.1
Introduction
Shoulder instability is a condition characterized by abnormal symptomatic slip of the humeral head out of the glenoid cavity . The incidence of anterior instability accounts for 80% of all types of instabilities including posterior and multidirectional instability . Anterior shoulder instability is a consequence of primary dislocation, with associated lesions such as Bankart lesion (detachment of the anterior inferior labrum) and Hill Sach’s lesion (a compression fracture at the posterolateral margin of the humeral head) that has not been properly treated. Recurrent dislocation frequently occurs in patients under 40 years (79%) than in those over 40 years (15%) .
Recurrent anterior shoulder instability is recently managed by arthroscopic techniques, which have been developed to reattach the labrum without an open incision and without subscapularis detachment. Therefore, better external rotation range was achieved following arthroscopic techniques . There are three categories for arthroscopic reattachment of the labrum:
- •
a transglenoid suture technique ;
- •
arthroscopically delivered and tied suture anchors ;
- •
arthroscopically delivered biodegradable tacs .
The American Society of Shoulder and Elbow Therapists (ASSET) designed a consensus rehabilitation guideline for use with patients who have undergone arthroscopic anterior capsule-labral repair in which the detached labrum is suture-anchored back to the glenoid rim and/or capsular tension is restored through suture tightening of the plicated capsule. The development of this rehabilitation guidelines was based on basic science and mechanistic studies, along with ASSET members’ expertise and clinical opinion because of the lack of clinical trials . Clinical trials comparing the effect of different rehabilitation programs after arthroscopic anterior capsule-labral repair using suture anchor and capsular shift are very scarce. A recent review of literatures revealed a single randomized clinical trial that reported the effect of accelerated rehabilitation versus the conventional rehabilitation with 3 weeks of immobilization . The recommendation was the use of the accelerated program to speed up recovery for selected cases.
The widely used arthroscopic techniques for anterior capsulolabral repair of the shoulder, together with the lack of evidence based rehabilitation programs and randomized clinical trials to dictate postoperative rehabilitation, raises many unanswered questions:
- •
Is supervised physical therapy program required after such minor invasive surgery or is a home-based program sufficient?
- •
Could a home-based program produce the same rate as supervised program with regards to motion and function recovery, after arthroscopic anterior shoulder stabilization?
Therefore, the purpose of this study was to compare the effects of a supervised physical therapy versus a controlled home-based programs, on the rate of shoulder motion and functional recovery. We hypothesized that the rate of motion and functional recovery would be different in patients who received a supervised rehabilitation versus a controlled home-based physical therapy programs following arthroscopic anterior shoulder stabilization.
1.2
Materials and methods
This study is a single-blinded randomized controlled trial that was conducted from February 2011 to June 2012 and approved by the Institutional Review Board of our university. Thirty patients diagnosed with recurrent anterior shoulder instability and who had undergone arthroscopic anterior shoulder stabilization were referred by an expert surgeon at the university hospital. All thirty patients were enrolled in this study. Patients were eligible to participate in the study if they met the following inclusion criteria:
- •
age ranged between 18 to 35 years;
- •
underwent unilateral anterior capsule-labral repair using suture anchors and capsular shift by the same surgeon;
- •
the cause of anterior instability was traumatic dislocation;
- •
chronic dislocation with at least one recurrent episode prior to surgery.
Subjects were excluded from the study if:
- •
the instability was caused by atruamatic dislocation or acute initial instability;
- •
presence of a bony Bankart lesion or any other associated lesions, such as ipsilateral rotator-cuff tear, or superior labrum anterior posterior (SLAP) lesions reported by the surgeon.
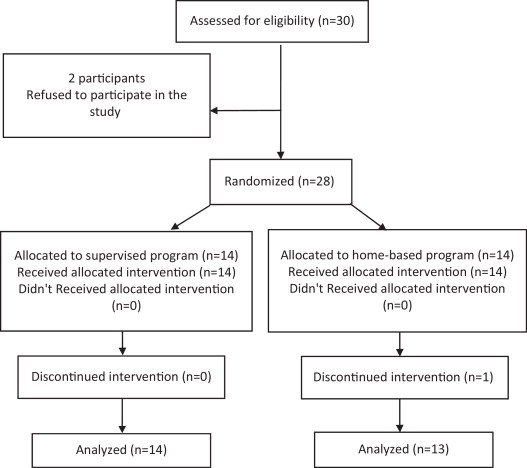
From the initial 30 patients assessed for eligibility, two refused to participate in the study. All twenty-eight patients who agreed to participate signed a detailed informed consent. Participants were blindly randomly assigned into two groups by an independent research assistant who opened opaque sealed envelope containing a card for either, the supervised or, the home-based rehabilitation program.
1.2.1
Treatment procedures
For the supervised group ( n = 14), patients received three sessions per week, for 24 weeks at the out-patient Physical Therapy clinic located at the university hospital. The design of the supervised program was based on the most popular guidelines for post-arthroscopic Bankart repair (ASSET , Voight et al. , Blackburn and Guido ) and Kim et al. accelerated rehabilitation program after arthroscopic Bankart repair. The rehabilitation program consisted of four phases: protective, restrictive, active and functional phases. The first and second phase lasted for 3 weeks each. Whereas the third and the fourth phase lasted for 6 weeks. Each phase was characterized by specific goals for the range of motion as was recommended by the ASSET consensus , strengthening, proprioceptive training and functional activities ( Tables 1–4 ). The duration and components of each phase was similar to that designed by the guideline of Blackburn and Guido and Voight et al. . The exercises were selected from all the four guidelines and the accelerated rehabilitation program of Kim et al. . Examples of the exercises are show in Figs. 1–4 .
| Goals | Intervention |
|---|---|
| Control of shoulder pain/edema | Cryotherapy |
| Maximally protect the surgical repair | Day 0: rest with a sling |
| Use a sling for 2 weeks during sleep only | |
| Achieve staged ROM | At 1st day |
| PFE = 90° | Pendulum exercise (unweight) |
| PER = 10–30° at 20° ABD | Active ROM of uninvolved joints; elbow & wrist flexion/extension |
| (PER at 90° ABD is contraindicated) | At 3rd day |
| 2–3 set of 10–25 repetitions | PFE in scapular plane |
| PFE not exceeds 90° at day 7 | |
| AAROM: with a stick to achieve staged ROM goals listed | |
| Step-backward exercise | |
| At 2nd POW | |
| PER in the scapular plane at 20° ABD | |
| AAROM with a stick to achieve staged ROM goals listed | |
| Scapular exercises (elevation, depression, protraction, retraction) | |
| Strengthening (within the protected ROM) 3–5 set of 10 repetitions | From 2nd to 3rd POW |
| Progressively weights will be used and increasing the load as tolerated (0–2 kg) using dumbbells | Start isometric exercise by flexion, ADD, ABD, extension, IR and ER (sub-maximal isometrics with 6 s hold) |
| Raising shoulders with scapular ADD (retraction) | |
| Push-ups without load – OKC – with weight (scapular protraction) | |
| ABD in scapular plane | |
| Prone horizontal ABD | |
| Bent row (scapular retraction) | |
| ER with arm at side | |
| Modified ER 90°/90° (in a prone position) | |
| IR with limb adducted at side | |
| Proprioception training (within the protected ROM) | At 2nd POW |
| 10–15 repetitions per session | Manual rhythmic stabilization (eyes opened then closed): at 90° flexion in the scapular plane against sub-maximal resistance |
| In IR | |
| In ER at 45° ABD | |
| Transfer of load (ball against wall) | |
| Goals | Intervention |
|---|---|
| Achieve staged ROM | AROM exercises |
| PFE 90–135° | PFE 90–135° |
| AFE ∼ 115° | AFE ∼ 115° |
| PER up to 35–50° at 20° ABD | At 4th POW |
| PER up to 45° PER at 90° ABD | Up to 35–50° PER at 20° ABD |
| ∼ 45–60° IR | At 6th POW |
| Up to 45° PER at 90° ABD | |
| ∼ 45–60° IR | |
| Strengthening (within the protected ROM) | Progressive strengthening exercises for the whole joint range available (increase weights as tolerated) |
| Grade 3 to 4/5 MMT | Push-ups with load – CKC – from a seated position |
| 3–5 set of 10 repetitions | Plyometrics: two hands pass |
| Progressively weights will be used and increasing load as tolerated (up to 2.5 kg) | |
| Proprioception (within the protected ROM) | Progressive load in an OKC and CKC exercises as quadruped progressed to tripod position (no push-ups from these positions) |
| 10–25 repetitions per session | PNF |
| Activities | All daily sedentary activities |
| Goals | Intervention |
|---|---|
| Achieve staged ROM | ROM exercises to achieve staged ROM goals listed (PFE, AFE, PER at 20 and 90° ABD, IR) |
| PFE: 155°–full elevation | Gradual increase in passive stretching |
| AFE: 145°–full elevation | |
| PER: 50–65° to full ER at 20° ABD | |
| 75° to full ER at 90° ABD | |
| Complete IR | |
| Strengthening | Modified push-ups exercise |
| Grade 4 to 5 MMT | Seated row |
| 3–5 set of 10 repetitions | Biceps curls |
| Progressively weights will be used and increasing the load as tolerated (up to 5 kg) | Triceps curls |
| Proprioception | Proprioceptive exercises in an OKC and CKC close to the maximum limit of the joint range |
| 10–25 repetitions per session | CKC with progressive load (knee push-ups) |
| OKC exercises | |
| Activities | Sedentary daily activities as tolerated |
| Light, non-repetitive overhead | |
| Lift light weight | |
| Goals | Intervention |
|---|---|
| Strengthening | Progressive active and passive ROM to full or sufficient joint function to participate in a sport |
| Grade 5 MMT | Continue previous exercises with gradual increasing of load using dumbbells |
| 3–5 series × 10 repetitions per session | Push-ups full loaded (military press exercise) |
| Progressive weights will be used and increasing the load as tolerated (up to 20 kg) | |
| Proprioception | CKC: full load on an unstable surface |
| 10–25 repetitions per session | Plyometrics: one hand throwing in elevated functional positions |
| Activities | Gradual progression of all activities |
| Gradual return to sport-related activity | |




For the controlled home-based group ( n = 14), the rehabilitation program consisted of 3 weeks protective phase of absolute immobilization in a sling. The goals and the exercises of the three following phases (restrictive, active and function) were the same as the supervised group. Patients were trained at the beginning of each phase on how to perform exercises. ROM to be avoided, was demonstrated to the patients and warnings about disruption of healing and recurrent dislocation were given. In addition, written instructions, illustrations and advice for exercises and ROM for each phase were given. Patients were allowed to contact the physical therapist by telephone or direct contact by visit if they required any further information.
1.2.2
Outcome measures
The primary outcome measure of this study was shoulder range of motion (ROM). In addition, functional recovery was also assessed. ROM was assessed after the completion of each phase of the rehabilitation program, whereas functional recovery was assessed after the third (12 weeks postoperative) and the fourth (24 weeks postoperative) phases. All assessments were carried out by the same assessor who was blinded to patients’ treatment allocation.
Shoulder forward flexion, abduction, internal rotation and external rotation at 90° and zero abduction of the two sides were measured using a handheld Universal goniometer. Goniometry was proved to be valid and reliable method for range of motion measurement. The intratester, intraclass correlation coefficients (ICCs) for all motions ranged from 0.87 to 0.99 .
Each motion range was measured 3 times and the average was calculated and expressed as a percentage of the normal side.
Functional performance was assessed using the Functional Impairment Test-Hand and Neck/Shoulder/Arm (FIT-HaNSA) and Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST). The FIT-HaNSA was developed and tested for validity and reliability in shoulder pathology by MacDermid et al. . Performance testing was done using commercially-available wooden shelves, nickel Chrome grid plates, stands and 3 plastic 1 kg containers as shown in Fig. 5 . The test consisted of 3 subtasks (‘waist-up’, ‘eye-down’, and ‘overhead work’). Each task could last up to 5 minutes, unless terminated based on the following stopping rules:
- •
the subject stopped or stated it was too painful to continue;
- •
the subject was out of pace provided by a metronome to the extent that they he/she was unable to complete one repetition of the movement within 2 beats of the metronome (for 5 successive repetitions);
- •
the subject substituted with the trunk/whole body movements and was not able to stop the substitution with verbal feedback for 5 successive repetitions of the same task;
- •
the examiner decided that the subject was at risk of injury or adverse events if the test were to be continued.
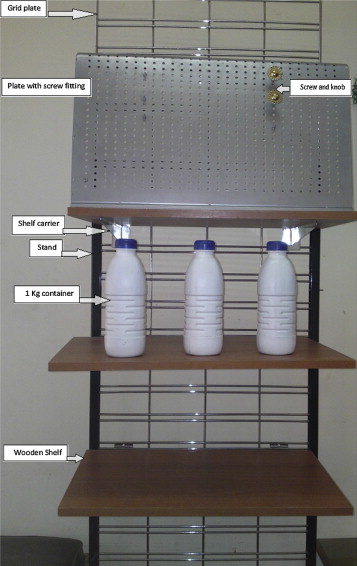
In the first task, or waist-up, a shelf was placed at patient’s waist level and a second shelf was placed 25 cm above. Three (1 kg) containers were placed 10 cm apart on the lower shelf. Using the affected arm, the patient was instructed to lift up the 3 containers, one at a time, from one shelf to the other, at a speed of 60 beats per minute, controlled by a metronome. Patients were instructed to continue with the task until 5 minutes have elapsed or they felt unable to continue. The time needed to complete the task was measured by a stopwatch.
For the second task, or eye-down, the shelves were adjusted so that one shelf was placed at the subject’s eye level and the second shelf was placed 25 cm below it. The patients were again instructed to use their affected arm to move the three containers between the shelves at a speed of 60 beats per minute.
In the third task, overhead work, a shelf was placed at the subject’s eye level with a screw fitting plate placed over the shelf. Patients were instructed to use their affected arm to repeatedly screw and unscrew a cupboard knob in a specific pattern, the knob in notch 1 (top) moves down to notch 2 (middle); the knob in notch 3 (bottom) moves up to notch 1; the knob in notch 2 moves down to notch 3 into the plate. Arms were required to be maintained elevated throughout the task execution. There was an approximately 30 s rest period in between each of the three tasks to allow shelves height adjustment.
CKCUEST is a reliable tool for functional evaluation of the shoulder with ICC of 0.922 for test-retest reliability. Two pieces of adhesive tape (1.5-in width) were placed on the ground parallel to each other 36 in apart. To start, the patient assumed a push-up position, with one hand on each piece of tape and the body kept as straight and parallel to the ground as possible. The shoulders were positioned directly over the hands. The subjects were instructed that from the starting position they were to use one hand to reach across their body and touch the piece of tape lying under the opposing hand and then return the hand to the original line. The subject then repeated the same movement with the other hand. A single test consisted of these alternating movements for 15 s as recorded by a stopwatch. Each subject performed 3 trials with a rest period of 45 s between trials. Subjects attempted as many “touches” as possible within the allotted time during the maximal tests. A touch was defined by one hand crossed over and touched the opposite line. The 3 maximal tests were averaged and normalized per body height (average number of touches/height) to be used as the subject’s test score.
1.2.3
Data analysis
The primary outcome measure in this study was shoulder ROM percentage improvement in forward elevation, abduction, internal rotation at 90° abduction, external rotation at 90° and at zero degree abduction. To determine the effects of the intervention programs, ROM variables were analyzed using 2-factor mixed model analyses of variance (ANOVAs) (2 groups by 4 time measurement points). The model was set with the group as the independent factor and measurement times (3 postoperative week [POW]; 6 POW, 12 POW and 24 POW) as the repeated factor, with a post-hoc test employed using Bonferroni correction. CKCUEST/height and FIT-HaNSA score were analyzed using independent t -test to determine difference between groups and paired t -test to determine difference within group. Statistical significance was set at P < 0.05. For statistical analyses, SPSS 21.0 software was used.
1.3
Results
1.3.1
Subjects
Out of the 28 patients who participated in the study, one subject from the home-based group did not continue in the study before first time measurement due to migration of one anchor that required revision surgery ( Fig. 6 ). The anchor migration was due to difficulty encountered in the surgical procedure and improper immobilization, not to error in exercise realization. Demographic data for the remaining 27 patients who completed the two rehabilitation programs are presented in Table 5 .
| Subject characteristics | Supervised group ( n = 14) | Controlled home-based group ( n = 13) | P value |
|---|---|---|---|
| Age (y) a | 26.4 ± 4.5 | 27.4 ± 9.3 | 0.71 b |
| Height (cm) a | 170.7 ± 6.7 | 171.3 ± 7.5 | 0.81 b |
| Weight (kg) a | 75.9 ± 11.4 | 85.9 ± 30.6 | 0.26 b |
| Gender (females, males) | 2, 12 | 1, 12 | 0.58 c |
| Dominant arm (right, left) | 13, 1 | 13, 0 | 0.32 c |
| Affected arm (dominant, non-dominant) | 7, 7 | 11, 2 | 0.06 c |
| Sport participation n (%) | 6 (42.8) | 6 (46.1) |
1.3.2
Range of motion
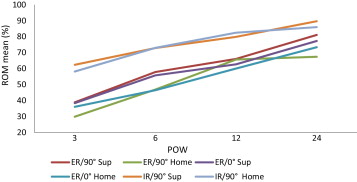
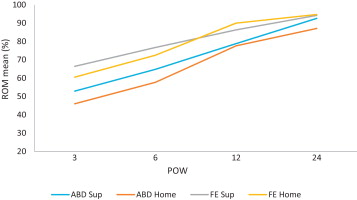
Shoulder abduction, forward elevation, internal rotation at 90° abduction and external rotation at 90° and zero degree abduction from the 3rd to the 24th weeks postoperative revealed non-significant group-by-time interaction in all measured ROM ( P > 0.05). There was a significant main effect across time in all measured ROM tests while there was no group main effect ( Table 6 ). Post-hoc tests revealed significant changes from 3 POW to the end of 24 weeks of rehabilitation in abduction and forward elevation in both groups with P < 0.05. However, the pairwise analyses for external rotation at 90° abduction and at side revealed no significant change from 6 POW to 12 POW in the supervised group only. The pairwise analysis of internal rotation at 90° abduction revealed no significant change from the 3 POW to the 6 POW and again from 12 POW to 24 POW in the supervised group. For the controlled home-based group, internal rotation at 90° abduction significant increased until the 12 POW and then the increase was not significant from 12 POW to the 24 POW. Figs. 7 and 8 present the data for shoulder ROM at the 4 measured times (3, 6, 12 and 24 POW). These graphs show progressive improvement of shoulder motion in both groups with no significant difference between groups detected.
| ROM (% of normal side) | 3 POW | 6 POW | 12 POW | 24 POW | P value (time effect) |
|---|---|---|---|---|---|
| ABD | |||||
| Sup | 52.9 ± 6.4 | 64.8 ± 11.6 | 78.8 ± 16.8 | 92.6 ± 10.5 | 0.001 |
| Home | 46 ± 7.2 | 57.7 ± 6.8 | 77.6 ± 12.9 | 87.1 ± 10.4 | |
| P value (group effect) | 0.11 | ||||
| FE | |||||
| Sup | 66.4 ± 11.7 | 76.7 ± 11.7 | 86.3 ± 6.6 | 94.2 ± 4.9 | 0.001 |
| Home | 60.5 ± 10.8 | 72.5 ± 9.6 | 90 ± 2.8 | 94.7 ± 3.0 | |
| P value (group effect) | 0.59 | ||||
| ER/90° | |||||
| Sup | 38.9 ± 19.8 | 57.9 ± 24.8 | 66.1 ± 24.1 | 81.1 ± 18.5 | 0.001 |
| Home | 29.9 ± 21.1 | 46.9 ± 18.6 | 65.7 ± 15.7 | 76.4 ± 15.1 | |
| P value (group effect) | 0.37 | ||||
| ER/0° | |||||
| Sup | 38.4 ± 15.1 | 55.8 ± 20.0 | 62.7 ± 19.1 | 77.3 ± 14.6 | |
| Home | 36.1 ± 20.5 | 46.5 ± 17.4 | 60.07 ± 15.5 | 73.4 ± 11.6 | 0.001 |
| P value (group effect) | 0.44 | ||||
| IR/90° | |||||
| Sup | 62.4 ± 20.4 | 72.9 ± 17.8 | 79.9 ± 16.9 | 89.7 ± 13.0 | 0.001 |
| Home | 58.2 ± 21.7 | 73.01 ± 19.9 | 82.5 ± 14.1 | 86 ± 8.2 | |
| P value (group effect) | 0.8 | ||||
1.3.3
Function
Table 7 shows the 12 POW and 24 POW results of the two functional tests (CKCUEST and FIT-HaNSA) for both groups. There were no significant differences between the two groups at all measured times ( P > 0.05). However, the score achieved in both tests significantly increased from 12 POW to 24 POW in both groups ( P < 0.05) with a large effect size (Cohen’s d = 0.95) in supervised group and medium effect size (Cohen’s d = 0.379) in the controlled home-based group for FIT-HaNSA. The effect size achieved in the CKCUEST/height was large in both groups (Cohen’s d = 1.26 and 0.86 for Sup and Home group respectively).
| Variables | Sup ( n = 14) | Home ( n = 13) | P value |
|---|---|---|---|
| CKCUEST/height | |||
| 12 POW | 0.106 ± 0.01 | 0.105 ± 0.02 | 0.87 |
| 24 POW | 0.126 ± 0.02 | 0.127 ± 0.03 | 0.91 |
| P value | 0.001 | 0.001 | |
| FIT-HaNSA | |||
| 12 POW | 251.5 ± 39.5 | 240.3 ± 52.7 | 0.53 |
| 24 POW | 284.4 ± 28.9 | 261.2 ± 57.6 | 0.2 |
| P value | 0.027 | 0.05 | |
1.4
Discussion
This study aimed at evaluating the effects of a supervised physical therapy program versus controlled home-based program on the rate of shoulder motions and function recovery after arthroscopic anterior shoulder stabilization. Analysis of the results showed that there were no significant differences between the supervised group and the controlled home-based group in the rate of recovery of all shoulder motions and function performance. However, there was a significant increase of all measured shoulder motions and function performance throughout the study period in both groups.
To achieve the aim of this study, we designed two physical therapy programs that were identical regarding the type of exercises used. However, the two programs differed with regard to the close supervision of performance as well as the immobilization period permitted. In the supervised program, the therapist followed up the patient, 3 sessions per week for 24 weeks. ROM performance was supervised and monitored by the therapist. In this group, arm immobilization was restricted to one week and during sleep only thereafter. In the home-based program, the patient performed the ROM independently and unsupervised, however, patient was seen by the therapist at the end of each rehabilitation phase only. Due to the lack of close supervision, the operated arm was immobilized for the first 3 weeks. This was for fear of patient may exceed the permitted range as pain after arthroscopy was relatively low . Following shoulder instability surgeries, Gibson et al. recommended immobilization of patient’s arm when passive ROM exceeds 90% and the joint end feel is elastic.
One of the ultimate goals after arthroscopic anterior shoulder stabilization is to gradually achieve full active ROM in order not to interfere with the healing process . We selected to follow up changes in ROM as indicators of recovery rate and restoration of functional ROM required to resume previous activities. ER was particularly important as Silvestro et al. found that ER in the unstable shoulder with the arm abducted 90°, averaged 14° less than that in the uninjured shoulder and 11° less than that measured with the arm at the side. Although, the external rotation with the arm 90° abduction required to perform functional tasks was found by Namdari et al. to be 59 ± 10°, the loss of 14° of external rotation indicated the liability of more restriction if physical therapy program was not properly designed to increase external rotation gradually during the healing process after surgery.
Our rehabilitation program addressed proprioception and function. Therefore, we intended to use a tool that objectively and directly assess function performance rather than using a functional rating scale or quality of life questionnaire which constitute subjective evaluation of therapeutic outcomes . We found that a new tool like FIT-HaNSA developed by MacDermid et al. can be used to assess functional performance for upper extremity activity. This tool depends in all its tasks on shoulder joint motion. These tasks require at least 120° of shoulder flexion, 25° of external rotation and at least 30° of external rotation . These ranges had to be maintained throughout the testing period at a preselected metronome speed. These tasks simulate daily activity of lifting and sustained overhead work in the household or workplace and assess both stabilization and movement . This tool was also found to correlate with the disabilities of the arm, shoulder and hand (DASH) questionnaire used in previous studies to assess patient upper extremity disability after arthroscopic anterior shoulder stabilization. However, it is recommended to investigate the sensitivity and size effect of this tool especially in shoulder instability population.
The CKCUEST was chosen for assessment as it addresses dynamic and static stabilities, which are important for our patients to return to previous activities. The CKC activities improve dynamic stability through joint approximation and co-contraction . They also stimulate mechanoreceptors and improve proprioception. The CKCUEST provides objective data to help therapist determining patient’s readiness to return to activity. It has the advantage of being easy for patient to understand and is cost effective .
The results of this study revealed significant improvement of all ROM of the shoulder in both groups. However, ER at 90° and at zero degree abduction remained without significant change from the 6 POW to 12 POW in the supervised group. This could be attributed to the close monitoring of ROM gain by the therapist. In the supervised group, after 3 weeks, ER/90° was 38.9% while that of the controlled home group was nearly 29.9%. By the end of 6th week, the ER/90° reached 57.9% in the supervised group, therefore, the therapist had to slowdown such increase in order to prevent stressing the healing tissue. Meanwhile, the controlled home group continued to gain range significantly.
The progress in internal rotation range was more rapid than external rotation in both groups. In the supervised group, at 3 POW the ROM was nearly 62%, whereas at 6 POW the control exerted by the therapist made range increase not significant. Being approximated to full ROM in both groups, the changes from 12 POW to 24 POW were not significant in both groups. It was recommended by Gaunt et al. to discontinue ROM exercises in the plane where stages ROM goals were exceeded. They also recommended not to stretch into end range external rotation, particularly at 90° abduction because they directly stress the anterior or anterior inferior glenohumeral capsule.
The continuous improvement of all ROM throughout the rehabilitation period can be attributed to different exercises in the rehabilitation program. Exercises used to regain forward elevation included stick-assisted elevation in supine and table step-back exercise. To regain external rotation, the therapist performed passive external rotation to the advised range and stick-assisted exercises. Gradual increase of passive stretching was introduced for all ROM from the 6 to 12 weeks postoperative.
By the end of the rehabilitation period, the results of active abduction and FE approached ROM of the healthy side in both groups. However, for active external rotation at 90°, the range of motion was 81.1% and 76.4% of the normal side in the supervised and home-based group respectively. Our results disagree with that of O’Neill , who found only 54% of the patients achieved full ROM after a mean duration follow up period of fifty-two months. This difference is due to three factors. First, their patients underwent arthroscopic transglenoid suture stabilization and not suture anchors. Second, their postoperative regimen was a conventional program that used a sling immobilization for 4 weeks and then instructions for exercises. Third, no follow up was done after each phase.
Only one study has prospectively compared accelerated and conventional rehabilitation programs. They reported faster gain in ROM of external rotation than conventional program in contrast to our results. Our patients in the supervised group reached to 81.1% of external rotation at 24 POW. Kim et al. allowed their patients to do external rotation at 90° of abduction to tolerance by the 5th week. According to the American Society of Shoulder and Elbow Therapists’ consensus rehabilitation guideline, passive ER at 90° abduction is allowed up to 45° by the 6th week. Kim et al. recommended the use of the accelerated rehabilitation program in selected cases who are not actively participating in any sport with healthy labrum and Bankart lesion limited to 1 cm above the midglenoid notch. Forty-four percent of our patients participated in sports and Bankart lesion was reported by the surgeon to be with different lengths requiring the use of 2 to 4 anchors.
Our results are in consistence with the conclusion of the systematic review conducted by Grumet et al. on the results of arthroscopic stabilization after recurrent instability followed by traditional physical therapy program. This program consists of 3 to 6 weeks of immobilization followed by active ROM program at 3 to 6 weeks and strengthening at 6 to 12 weeks. They reported nearly 100% of forward elevation and abduction, 80% to 90% of external rotation at 90° of abduction. These results were obtained at follow up period ranged from 24 to 52 months. We expected that our patients would progressively gain external rotation range by 24 weeks as they have gained 76.4% and 81.1% of ER/90° in the home and supervised groups, respectively. A follow up will be conducted annually in addition to quality of life and recurrence rate assessment. However, no recurrent dislocation was noted in any case in either group throughout the study period.
The focus of this study is the rehabilitation program outcomes and not the surgical outcomes. Our program addresses many aspects of rehabilitation including strength, proprioception and function. To the author’s knowledge, there are no previous studies that assessed functional performance after arthroscopic anterior shoulder stabilization. Therefore, it was difficult to compare the current results of CKCUEST and FIT-HaNSA with other studies.
However, we found a significant improvement in the score of both tests. The maximum score in FIT-HaNSA is 300 s, which is the score that must be achieved by healthy individuals. Our patients reached 284.4 s and 261.2 s in the supervised and home groups, respectively. This means 94.8% and 87% of the maximum possible score. The strength and proprioceptive training were gradually increased in difficulty using different exercises, load and repetition. Weight bearing through the upper extremity as in the CKC exercises were included in the rehabilitation program through pressing a ball against the wall, push-up from seated position, quadruped and tripod position with progressive load on the upper extremity, modified push-up that progressed to knee push-up then military press, and CKC with full load on unstable surface. These exercises maximize the use of mechanoreceptors and allow for more accurate position sense, and increase overall stability of the glenohumeral joint. This was reflected in the greater improvement of FIT-HaNSA and CKCUEST that require stability, mobility, strength and proprioception.
One important point we have noticed was that all patients in the controlled home-base rehabilitation program were compliant with the program and many calls were received to ask about performance and rate of exercises needed. In addition, they attended every training given at the beginning of each phase. However, no supervision was done thereafter.
There were three limitations in this study:
- •
first, the patients in the supervised group dropped some physical therapy sessions especially in the last month of the final phase of rehabilitation (which was ranged from 1 to 2 sessions/week);
- •
second, our sample size is small. However, this was a result of including only patients operated by the same surgeon. This in itself is an advantage as it ensures standardization of surgical technique. However, a larger sample size is recommended before generalization of the current results;
- •
third, the lack of measurement of function through questionnaire could make the study difficult to be included in meta-analysis.
In conclusion, this study demonstrated that supervised physical therapy and controlled home-based programs progressively improve ROM and function after arthroscopic anterior shoulder stabilization. We suggest using the supervised program if the patient is non-compliant and prefer not to be immobilized. On the other hand, the controlled home-based program may be more appropriate to those who do not mind immobilization and who are able to follow instructions or not able attend regular physical therapy sessions. A further study is recommended to study patient preference effect on ROM and function outcomes. A point which still needs to be investigated is cost-ratio analysis to optimize the selection of controlled home-based versus supervised rehabilitation program.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
L’instabilité de l’épaule est une pathologie caractérisée par la luxation symptomatique anormale de la tête humérale hors de la cavité glénoïde . Le taux d’incidence de l’instabilité antérieure représente 80 % de tous les types d’instabilité y compris l’instabilité postérieure et l’instabilité multidirectionnelle . L’instabilité antérieure de l’épaule est une conséquence d’une dislocation primaire, avec des lésions associées telles que la lésion de Bankart (détachement du bourrelet antéro-inférieur) et la lésion de Hill-Sachs (fracture par compression au bord postéro-latéral de la tête humérale) , et qui n’a pas été traitée correctement. La dislocation récurrente se produit plus fréquemment chez les patients de moins de 40 ans (79 %) que chez les plus 40 ans (15 %) .
L’instabilité antérieure récurrente de l’épaule est depuis peu traitée par des techniques d’arthroscopie qui ont été développées pour ré-attacher le labrum (bourrelet glénoïdien) sans pratiquer de grande incision et sans détachement du sous-scapulaire. Ainsi, une meilleure mobilité en rotation externe est obtenue après les techniques sous arthroscopie . Il existe trois méthodes de ré-attachement du labrum par arthroscopie :
- •
une technique par suture trans-glénoïdienne ;
- •
des ancres de suture insérées et fixées par arthroscopie ;
- •
des implants bio-absorbables de type tacs insérés par arthroscopie .
L’ASSET (American Society of Shoulder and Elbow Therapists) a établi par consensus une directive de recommandations portant sur la rééducation des patients ayant bénéficié d’une réparation capsulolabrale antérieure par arthroscopie où le labrum détaché a été re-suturé-ancré au bord de la glène et/ou la tension capsulaire est restaurée par des sutures resserrant la plicature capsulaire. Ces recommandations destinées à la rééducation ont été développées à partir d’observations scientifiques fondamentales et d’études mécanistiques, mais aussi grâce aux connaissances et à l’avis clinique des membres de l’ASSET, étant donné le manque d’essais cliniques . Les essais cliniques comparant l’efficacité de différents programmes de rééducation après réparation capsulolabrale antérieure sous arthroscopie à l’aide d’ancres de suture et stabilisation capsulaire de l’épaule sont très rares. Une récente revue de la littérature n’a permis de trouver qu’un seul essai clinique randomisé qui rapporte l’efficacité d’une rééducation accélérée par rapport à la rééducation conventionnelle après 3 semaines d’immobilisation . Leur recommandation était de choisir le programme court pour accélérer le rétablissement dans certains cas.
Le fait que les techniques arthroscopiques sont largement utilisées dans la réparation capsulolabrale antérieure de l’épaule, associé au manque de programmes de rééducation fondés sur des données expérimentales ainsi que d’essais cliniques randomisés permettant d’imposer une rééducation postopératoire, soulève de nombreuses questions pour lesquelles nous n’avons pas encore de réponses :
- •
Un programme de physiothérapie supervisé est-il nécessaire après une opération chirurgicale invasive mineure ou un programme effectué à domicile serait-il suffisant ?
- •
Après une stabilisation antérieure de l’épaule sous arthroscopie, un programme effectué à domicile peut-il permettre une récupération de la mobilité et de la fonction aussi rapidement qu’un programme supervisé ?
Par conséquent, le but de cette étude est de comparer les effets d’un programme de physiothérapie supervisée à ceux d’un programme à domicile contrôlé, sur la vitesse de récupération de la fonction et de la mobilité de l’épaule. Nous avons formulé l’hypothèse que la rapidité de récupération de la fonction et de la mobilité serait différente entre les patients qui bénéficiaient d’un programme de rééducation supervisée et ceux qui suivaient un programme de physiothérapie à domicile contrôlé après une stabilisation antérieure sous arthroscopie de l’épaule.
2.2
Patients et méthodes
Cette étude est un essai randomisé en simple insu comparatif qui a été réalisé de février 2011 à juin 2012 après approbation du comité d’éthique de la recherche de notre université. Trente patients ayant reçu un diagnostic d’instabilité antérieure récurrente de l’épaule et qui avaient bénéficié d’une stabilisation antérieure de l’épaule sous arthroscopie ont été référés au centre hospitalo-universitaire par le chirurgien spécialisé. Les trente patients ont été inclus dans l’étude. Pour participer à l’étude, les patients devaient satisfaire aux critères d’inclusion suivants :
- •
âge entre 18 et 35 ans ;
- •
patient ayant bénéficié d’une réparation capsulolabrale antérieure unilatérale à l’aide d’ancres de suture et stabilisation capsulaire réalisés par le même chirurgien ;
- •
la cause de l’instabilité antérieure est une dislocation traumatique ;
- •
luxation chronique avec au moins un épisode récurrent avant chirurgie.
Les sujets n’étaient pas inclus dans l’étude si :
- •
la cause de l’instabilité est une dislocation non traumatique ou une instabilité initiale aiguë ;
- •
présence d’une lésion osseuse de type Bankart ou tout autre type de lésions associées, telles qu’une rupture de la coiffe des rotateurs ipsilatérale, ou des lésions SLAP (antéro-postérieures du labrum supérieur) rapportées par le chirurgien.
Sur les 30 patients évalués pour l’inclusion, deux ont refusé de participer à l’étude. Les vingt-huit patients ayant accepté de participer ont signé une fiche détaillée de consentement éclairé. Les participants ont été répartis de façon aléatoire dans les deux groupes par un assistant de recherche indépendant en ouvrant des enveloppes scellées opaques contenant un carte désignant soit le programme de rééducation supervisée soit celui à domicile.
2.2.1
Procédures thérapeutiques
Dans le groupe supervisé ( n = 14), les patients avaient trois séances de rééducation par semaine, pendant 24 semaines à la clinique de physiothérapie en ambulatoire située au centre hospitalo-universitaire. Le schéma du programme supervisé était basé sur les recommandations les plus suivies dans le cas de la réparation d’un Bankart post-arthroscopie (ASSET , Voight et al. , Blackburn et Guido ) ainsi que le programme de rééducation accélérée de Kim et al. . Le programme de rééducation comportait quatre phases : une phase protective, une phase restrictive, une phase active et une phase fonctionnelle. Les deux premières phases duraient 3 semaines chacune. La troisième phase et la quatrième phase duraient 6 semaines chacune. Chaque phase était caractérisée par des objectifs spécifiques à atteindre en mobilité articulaire (d’après les recommandations du consensus ASSET ), en renforcement, en travail proprioceptif et pour les activités fonctionnelles ( Tableaux 1–4 ). La durée et les composantes de chaque phase étaient semblables à celles décrites dans la directive de Blackburn et Guido et Voight et al. . Les exercices ont été choisis dans les quatre directives et le programme de rééducation accélérée de Kim et al. . Des exemples d’exercices sont présentés sur les Fig. 1–4 .









