Miscellaneous Problems: Synovitis, Degenerative Joint Disease, and Tumors; Miscellaneous Conditions: Ligamentum Teres, Synovial Disease, Degenerative Joint Disease, Tumors
Thomas G. Sampson
LIGAMENTUM TERES
The ligamentum teres is located deep within the central compartment of the hip and is amenable to arthroscopic inspection. Injury to the ligament and many of the pathologic conditions involving it are associated with developmental dysplasia of the hip. Fortunately, dysplastic hips are more flexible, making it easier to distract the hip and diagnose and treat injuries and pathologies of the ligamentum teres. Patients usually present with groin pain and a limp or clicking.
Gray and Villar (1) classified pathology of the ligamentum teres using arthroscopic surgery. After looking at 472 consecutive hip arthroscopies, they identified 20 patients with ligamentum teres tears pathology. They placed them in three categories: Group 1, complete ligamentum teres rupture; group 2, partial tear of the ligamentum teres; and group 3, degenerative ligamentum teres (Fig. 52.1). All were treated with debridement. There were a few case reports of either tears or avulsion fractures involving the ligamentum teres (2, 3); however, Byrd prospectively looked at 23 patients with ligamentum teres tears and found 7 occurred from violent injuries, such as motor vehicle accidents, 3 from a fall from a height, 3 from football injuries, 1 from snow skiing, 1 from ice hockey and included 6 dislocations. The remaining 8 patients sustained twisting injury. He found a lengthy duration before diagnosis and surgery with an average of 28.5 months. All of his patients experienced groin pain, and 19 of them experienced catching, popping, locking, or giving way, as well as pain with activities. He used a variety of diagnostic tests such as MRI, CT scan, and radionuclide bone scans. The indication for surgery was intractable hip pain.
Simpson and Villar (4) described a method for ligateres reconstruction in a 20-year-old using an artificial graft and Endo button. It appears that they are very rare indications, such as persistent hip pain and instability between the head and the acetabulum.
SYNOVIAL DISEASE
Synovitis of the hip has many causes. Five of the pathologic entities causing primary synovitis are (1) rheumatoid arthritis (RA) (2), calcium pyrophosphate dihydrate (CPPD) crystal deposition disease (3), fatty deposition disease (hyperlipoproteinemia) (4), hemochromatosis, and (5) pyarthrosis.
The role of arthroscopic synovectomy in treating synovial diseases was apparent to the earliest arthroscopists. In almost all pathology of the hip, synovitis is present. We had several undiagnosed cases of hip pain with effusions that were shown to be seronegative rheumatioid arthritis with synovial biopsy. In 1988, Ide et al. (5) performed arthroscopic synovectomy for RA on six hips in three patients using mechanical shavers through a two-portal technique with good results. With the advent of laser and radiofrequency (RF) ablation, there are now three modalities used to debride the synovium. It remains difficult to reach 100% of the joint. However, with newer, more effective medical management, debulking of the diseased synovium seems to be adequate.
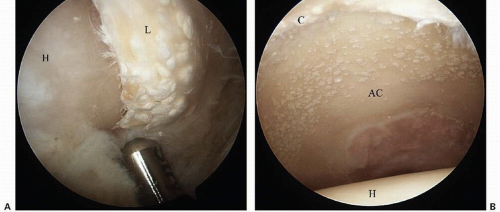
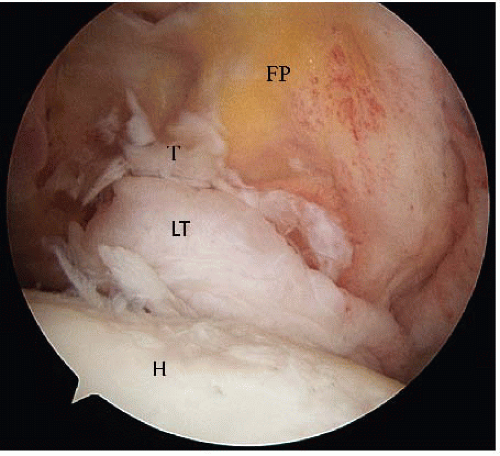 FIGURE 52.1. Degenerative tear ligamentum teres in a 48-yearold female with mild hip dysplasia. LT (ligamentum teres), T (tear), H (head), FP (fat pad). |
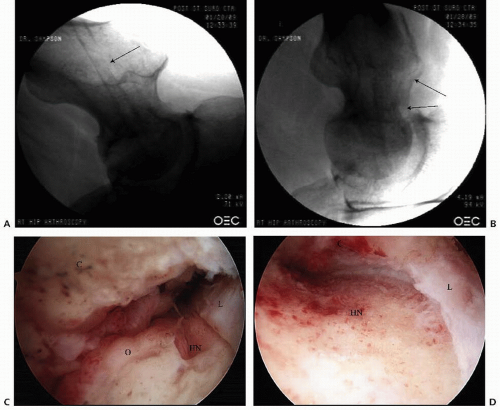
CPPD crystal deposition disease has not been reported as frequently in the hip as it has in the ligamentum flavum and in the knee associated with RA (6, 7). We have performed synovectomy on two patients for CPPD associated with femoroacetabular impingement (FAI). Clearly, it is an entity that should be considered in the differential diagnosis of patients with refractory synovitis (Fig. 52.2 A-B).
There are no reports in the arthroscopic literature on the treatment of hyperlipoproteinemia, hemochromatosis, or any of the metabolic arthropathies. We have performed partial synovectomy in a few patients thought to have fatty deposition and in one patient with hemochromatosis associated with arthritis (Fig. 52.3). It is presented here only to make the arthroscopic surgeon aware that metabolic arthropathies exist (8). Metabolic arthropathy appears as white or yellowish plaques on the articular cartilage associated with a mild synovitic reaction. The plaque cannot be removed without destroying the articular cartilage and therefore should be treated with synovectomy only.
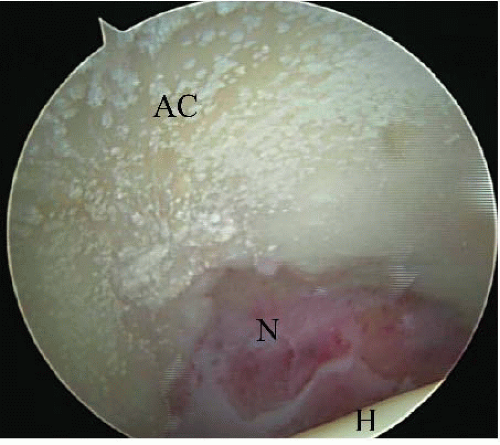 FIGURE 52.3. Lipid deposition on the articular cartilage of the acetabulum (arrow), AC (acetabular cartilage), N (notch), H (femoral head.) |
Arthroscopic debridement and lavage has become the treatment of choice for septic arthritis in children, adolescents, and adults. This modality has been associated with minimal morbidity and an excellent cure rate (9, 10, 11 and 12). McCarthy et al. (13) reported on successful treatment of septic total hips in two patients using arthroscopic debridement, lavage, and intravenous antibiotics. We have successfully treated arthroscopically four patients with late hematogenous infections of their total hips. No recurrence has been noted, with the longest follow-up being
20 years when one patient passed away owing to natural causes at the age of 93 years.
20 years when one patient passed away owing to natural causes at the age of 93 years.
DEGENERATIVE JOINT DISEASE
The arthroscopic treatment of degenerative joint disease (DJD) of the hip remains controversial, challenging, and difficult. Even the most experienced hip arthroscopists avoid the procedure because there are few benchmarks to predict a successful outcome. Prior to 2001, DJD was treated with arthroscopic debridement, labrectomy, synovectomy, and abrasion chondroplasty. In 28 of 290 patients who had partial labrectomies with DJD, only 21% had a good result compared with a 71% good result rate in those without DJD (14). Subsequently, with the recognition of FAI and the added correction of the abnormal morphology, the modified Harris Hip Score improved significantly from 72 to 92 with an average of 4 years follow-up (15, 16 and 17).
A residual head-neck deformity from femoral neck fractures has been a cause of FAI and DJD. Reshaping of the deformity has been done using an open surgical dislocation by Eijer et al. (18). We have treated the DJD and deformity with an arthroscopic head-neck osteoplasty and debridement, synovectomy, and abrasion chondroplasty with microfracture in three patients (Fig. 52.4 A-F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree