Miscellaneous Hip Conditions: Coxa Saltans (“the Snapping Hip”), Trochanteric Bursitis, and Meralgia Paresthetica
Kristofer J. Jones
Charles L. Nelson
Coxa Saltans (“the Snapping Hip”)
CLINICAL PRESENTATION
Coxa saltans, or “snapping hip” syndrome, is a clinical condition characterized by an audible “snap” or “pop” that typically occurs with dynamic hip motion. Several causes of this clinical entity have been implicated, and all are related to the anatomic location of the offending structure: external, internal, and intra-articular (Table 13-1).
TABLE 13-1 Etiologies of Snapping Hip | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
External Etiology
In cases of external coxa saltans, the history can be extremely helpful in establishing the diagnosis. Patients will explain a “snapping, painful” sensation over the lateral hip and commonly localize pain to the greater trochanter when asked to identify the area of maximal tenderness. Traditionally, the external snapping hip has been associated with a thickened posterior border of the iliotibial (IT) band or anterior border of the gluteus maximus, which predispose the IT band to slipping back and forth over the greater trochanter. The thickened IT band lies posterior to the greater trochanter as the hip sits in extension, and as the hip is flexed, the band forcefully slides anteriorly over the trochanter, producing pain and an audible sound. The greater trochanteric bursa, which lies between the IT band and the greater trochanter, can become inflamed as the band continuously slides over the bursa, leading to inflammation and contributing to the patient’s painful symptoms.
Internal Etiology
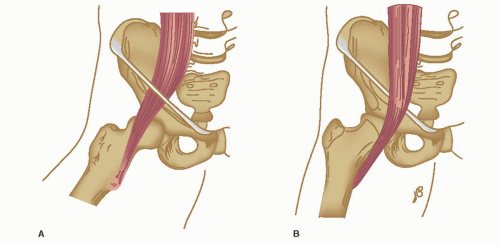
Patients with internal coxa saltans typically describe a painful clicking/popping sensation emanating from the deep, anterior groin. It is now well accepted that the source of pain and audible snapping is produced by subluxation of the iliopsoas tendon during hip range of motion. The structure most commonly responsible for transiently impeding translation of the iliopsoas tendon has been debated; however, most believe that the snapping phenomenon is due to subluxation of the tendon over the anterior femoral head and capsule or the pectineal eminence at the anterior brim of the pelvis (Fig. 13-1). A significant source of pain found in patients with internal snapping hip can be localized to the iliopsoas bursa, the largest synovial bursa in the body. The iliopsoas bursa is found between the iliopsoas tendon and anterior hip capsule, and significant inflammation of this structure from repetitive sliding of the tendon can be extremely painful for patients with this condition.
CLINICAL POINTS
The mainstay of treatment for internal or external coxa saltans is conservative therapy given the high likelihood of success.
It is rare for a case to prove refractory to an extensive regimen of nonoperative treatment.
PHYSICAL FINDINGS
External Type
On physical examination, the diagnosis of external coxa saltans can be established by reproducing the snapping motion of the tendon over the greater trochanter. In order to test the patient properly, they should lie on their side with the affected leg up. Upon flexion of the involved leg at the hip, it should be easy to palpate the area of snapping over the greater trochanter. The diagnosis can be clinically confirmed if tendon snapping is prevented with direct manual pressure applied over the greater trochanter by the examiner.
Internal Type
Focused physical examination of patients with internal coxa saltans should be performed in the supine position. In order to reproduce the snapping sensation, the examiner should bring the hip from a flexed, abducted, and externally rotated position down into extension with internal rotation. If direct pressure over the anterior hip at the level of the femoral head prevents the snapping sensation, the diagnosis of internal coxa saltans can be made with clinical confidence.
STUDIES (LABS, X-RAYS)
Coxa saltans is a clinical diagnosis that should be confirmed with physical examination. There is no clear consensus on the optimal imaging tests that should be used to establish the diagnosis. Plain radiographs are not typically useful in the diagnosis given the dynamic nature of the condition; however, they may be helpful to rule out other clinical conditions. Magnetic resonance imaging (MRI) may reveal indirect evidence of involvement if there is inflammation of the surrounding bursal structures. Iliopsoas bursography, typically used for internal coxa saltans, can be performed under fluoroscopic guidance to inject contrast material and highlight the snapping ilipsoas tendon. This imaging modality is the definitive and single most useful procedure in the diagnosis of internal snapping hip syndrome.
TREATMENT
Asymptomatic snapping hip should be considered a benign and normal occurrence, especially in young, athletic patients. For these individuals, no definitive treatment should be sought unless the condition becomes symptomatic and functionally limiting. If the patient develops symptoms over time and an external or internal etiology can be definitively diagnosed, the optimal treatment consists of conservative measures.
Nonoperative therapy involves icing the affected area to reduce any inflammation, nonsteroidal anti-inflammatory drugs (NSAIDs), and avoidance of all physical activities that reproduce the pain. For patients who experience severe symptoms such as pain with normal ambulation and other activities of daily living, an appropriate treatment protocol involves ice, rest, and hydrocortisone injection into the affected area. Of note, one should never inject corticosteroid into an area that appears infected. Steroid treatment should be followed by a detailed physical therapy program that consists of stretching the tensor fascia lata and gluteus muscles. Ultimately, conservative therapy is the mainstay of treatment in this disorder because most patients improve with a dedicated treatment regimen. Surgical intervention is rarely necessary and should only be considered for refractory cases following an extensive course of conservative modalities.1