Minimally Invasive Treatment of Ankle Fractures
Jodi Siegel
The goal in treating ankle fractures is to have a well-aligned mortise at union. Open reduction and internal fixation of unstable ankle fractures is the most frequent surgical intervention used to achieve an anatomic reduction and stable fixation. In certain circumstances, minimally invasive treatment options may be more appropriate. Compromised soft tissue envelopes or patients with significant medical comorbidities may benefit from these techniques.
EXTRAPERIOSTEAL PLATING OF PRONATION-ABDUCTION ANKLE FRACTURES
Indications
Pronation-abduction ankle fractures, as described by Lauge-Hansen,1 are caused by translation rather than rotation. The medial side fails first under tension. The fibula fails last, typically resulting in a transverse fracture associated with lateral comminution several centimeters proximal to the joint. This fracture may be more effectively treated with extraperiosteal plating.
Patient Positioning
The patient is positioned supine on a standard operating room table with a small bump placed under the ipsilateral hip so that the knee is straight up and down.
Surgical Approaches
If a supracollicular medial malleolus fracture is present, it is repaired first as it will help restore congruence of the talus beneath the plafond, thereby assisting with reduction of the lateral malleolus.
Turning attention laterally, the ankle is positioned on bolsters placed at the level of the joint and not under the heel. Placing the bolters under the heel can cause anterior subluxation of the talus and cause a malreduction. The reduction maneuver is performed (see Reduction Techniques section). After assessing the reduction, a lateral incision is made over the posterior half of the fibula. Care is taken when dividing the subcutaneous tissue onto the periosteum, as the periosteum is located immediately subcutaneous. Sharp Weitlaner retractors can aid by applying tension to the skin causing the subcutaneous tissue to peel off the periosteum. Often there are rents in the periosteum due to the injury. Take care to leave the remaining periosteum intact; do not strip or further handle the fracture fragments. At this point, retractors should be removed as tension on the surrounding tissues can cause shortening of the fibula.
Reduction Techniques
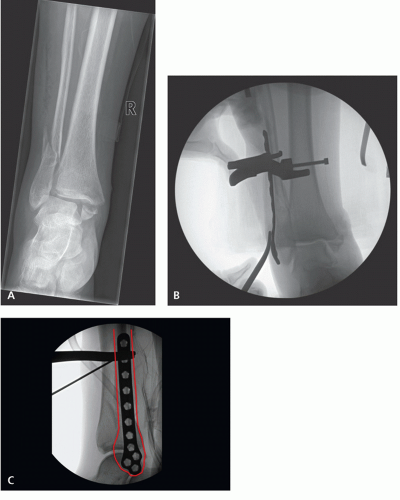
Prior to the lateral incision, the ankle is placed on a bolster. The foot is adducted and medially translated to center the talus in the mortise. This aids in obtaining fibular length as the lateral ankle ligaments typically remain intact. Fluoroscopic images are used to determine
fibular length (Fig. 14.1). Although the lateral cortex is comminuted, the medial cortex often involves a single fracture line and can be used to assess length. In addition, the talocrural angle is compared to the uninjured ankle to confirm fibular length.2 Once the necessary reduction maneuver is confirmed, one can proceed with the approach.
fibular length (Fig. 14.1). Although the lateral cortex is comminuted, the medial cortex often involves a single fracture line and can be used to assess length. In addition, the talocrural angle is compared to the uninjured ankle to confirm fibular length.2 Once the necessary reduction maneuver is confirmed, one can proceed with the approach.
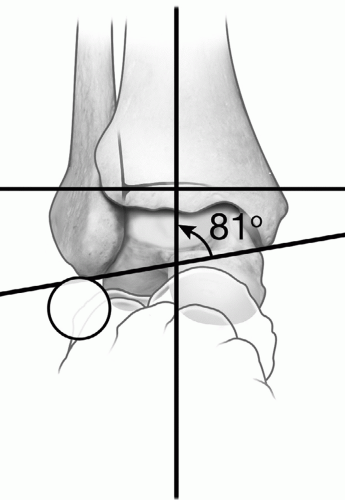 Figure 14.1 Assessing fibular length radiographically is aided by measuring the talocrural ankle, for which normal is reported at 83 ± 4 degrees.2 The contralateral ankle can be used as a control. In addition, the “ball sign” is described as the smooth curve made by the distal tip of the fibula and the lateral process of the talus.21 |
After the extraperiosteal dissection is completed, a reduction is affected by manipulating the foot. A lateral fluoroscopic image is then obtained to ensure there is no angulation or translation of the fibula. Returning to the coronal plane imaging, a precontoured, underbent direct lateral fibular plate is placed directly lateral on the fibula. Take care to position the plate in the center of the bone by palpating the anterior and posterior borders of the fibular shaft as the intact soft tissues will preclude adequate visualization. A fluoroscopic lateral view will confirm appropriate position, which is essential as the plate must apply a direct medial force to accurately reduce the fracture. Any angulation at the fracture site must be corrected, often simply by adjusting the bolsters. Once appropriate position is confirmed, the plate is temporarily secured by Kirschner wires, provisional fixation pins, or a reduction clamp. Residual lateral translation will be corrected by the plate (Fig. 14.2). Bicortical nonlocking screws are then placed from proximal to distal, pushing the fibula (and the talus) medially to its position under the plafond. Fluoroscopic imaging confirms reduction.
The syndesmosis is then evaluated either by applying an abduction stress on the foot (if the medial malleolus is intact) or by using a clamp on a fibula to apply the stress (if the medial malleolus is a fracture that was repaired) and is reduced and stabilized if unstable.
Fixation
Precontoured direct lateral fibular plates or straight one-third tubular small fragment plates that are contoured to the shape of the distal fibula are ideal. Underbent, flexible plates allow the plate to correct and buttress the lateral translation of the fibula. Nonlocking, bicortical screws are placed from proximal to distal within the plate to allow the implant to effect a reduction.
Complications
Hardware irritation due to lateral plating is a common complaint from patients. Functional outcome scores are worse for patients with hardware-related pain, and implant removal does not guarantee resolution of pain.3
Accurately assessing and obtaining appropriate fibular length is mandatory to restore proper ankle mechanics.4,5 Fibular shortening leads to lateral talar tilt and medial clear space widening. With only 1 mm of lateral talar shift, there is 42% decrease in contact area, thereby increasing the risk of post-traumatic arthritis.5 Symptoms may present as late as 5 years after malunion with varying degrees of radiographic arthritis present.6 Proper reduction of fibular length and rotation, leading to a reduced mortise, will prevent talar tilt and medial widening and decrease the risk of late arthritic pain.
Rehabilitation Protocol
Postoperatively, patients are placed into a short leg cast and kept non-weight-bearing for 6 weeks. If syndesmotic fixation is needed, weight-bearing may be deferred for 12 weeks. Active and passive range of motion is started at 4 to 6 weeks.
Outcomes
Historically, pronation-abduction ankle fractures have the highest nonunion rate and authors have recommended bone grafting after traditional fixation techniques.7,8 A small series stabilized using this extraperiosteal technique reported union of all fractures within 10 weeks and no deep infections.9
SYNDESMOTIC-ONLY FIXATION FOR WEBER-C ANKLE FRACTURES
Indications
The Danis-Weber ankle fracture classification describes the level of the fibula fracture in relationship to the syndesmosis. Fibula fractures that occur above the syndesmosis, with an adequate segment of intact fibula for placement of at least two syndesmotic screws, can
be repaired with syndesmotic-only fixation, provided adequate fibular length and mortise reduction is achieved.
be repaired with syndesmotic-only fixation, provided adequate fibular length and mortise reduction is achieved.
Patient Positioning
Patients are positioned supine with a bump under the affected hip, which allows the leg to be easily internally rotated, granting access to the fibula.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree