Minimally Invasive Total Shoulder Arthroplasty
Laurent LaFosse
Kalman J. Piper
Total shoulder arthroplasty (TSA) remains the gold standard for treatment of osteoarthritis, rheumatoid arthritis, fractures and their sequelae, and avascular necrosis. It provides reliable and predictable pain relief with good to excellent long-term outcomes in the majority of patients. Complications associated with the rotator cuff, and in particular the reattachment of the subscapularis tendon after a standard approach, have long been recognized as a potential source of poor patient outcomes (1, 2). Subscapularis tear after reinsertion is an indication for early revision, often with very poor results after the revision procedure. In order to avoid complications associated with the rotator cuff, postoperative rehabilitation is slow and often delayed for 6 weeks, to allow the tendon reattachment to heal before it is tested.
To avoid the complications associated with failure of cuff healing, several techniques have been developed, including lesser tuberosity osteotomy rather than tenotomy (3, 4, 5); transacromial, transsupraspinatus approaches (6); and, most recently, the minimally invasive, rotator cuff sparing technique. Initially, the minimally invasive technique utilized the superior, transdeltoid approach to expose and perform the arthroplasty via the rotator interval (7). While the technique achieved the goal of avoiding a tenotomy and facilitated faster, unrestricted postoperative rehabilitation, access to the inferior aspect of the joint was poor. In our initial review of this technique, we found many patients had residual inferior osteophytes on the humeral side and a small proportion of patients had problems caused by the deltoid spilt. In direct response to these problems, the technique was modified. The technique now uses the deltopectoral approach and incorporates an inferior arthrotomy below the subscapularis tendon to allow visualization and removal of inferior osteophytes, prior to preparation and insertion of the TSA via the rotator interval.
INDICATIONS AND CONTRAINDICATIONS
To date, the technique has been used for treatment of mild to moderate primary glenohumeral osteoarthritis in patients with an intact rotator cuff. Performance of the technique requires a relatively mobile glenohumeral joint as the arm needs to change position to facilitate access to the appropriate parts of the joint via the superior and inferior “windows” or arthrotomies. The technique is contraindicated in patients with immobile joints or grossly deformed glenohumeral joints. During the development of this procedure, two patients had humeral components positioned too high due to excessive joint stiffness and inability to place the jigging system correctly. It should be noted, however, that in difficult cases or during the learning curve associated with this technique, the procedure can quickly and easily be converted to the traditional technique via detachment of the subscapularis tendon, with or without an osteotomy, at any stage.
PREOPERATIVE PLANNING
In addition to standard preoperative assessment from the medical and anesthetic teams, a full shoulder examination is performed, including a neurological assessment. No neurological complications have been reported; however, the creation of the inferior window involves identification and exposure of the axillary nerve, and its normal
function should be documented prior to the procedure. All patients undergo a preoperative CT arthrogram to ensure the rotator cuff is intact and to accurately assess the bone stock and glenohumeral joint deformity.
function should be documented prior to the procedure. All patients undergo a preoperative CT arthrogram to ensure the rotator cuff is intact and to accurately assess the bone stock and glenohumeral joint deformity.
SURGERY
Anesthesia, Patient Positioning, and Draping
After combined general and interscalene regional anesthesia, the patient is positioned in the beach-chair position with approximately 45 degrees of tilt of the backrest. The hips and knees are flexed, and bony prominences are padded. Scapular motion is minimized by ensuring that the scapula is fully supported by the backrest; however, the arm should be able to be extended by the side of the table. The arm is free draped and occlusive drapes are positioned far enough medially to allow full access to the deltopectoral interval. The drapes are held in position with antimicrobial adhesive sheets. The patient is given a single prophylactic dose of cefazolin at the time of surgery. Two assistants are used during the procedure.
Deltopectoral Approach
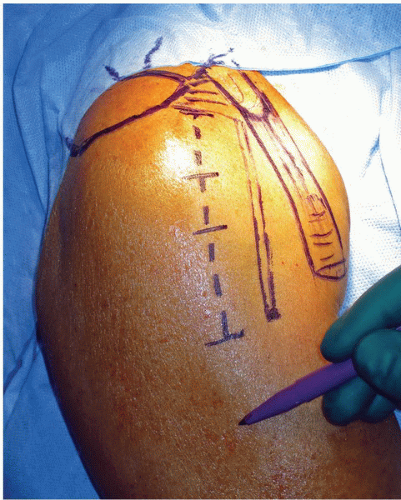
A 10-cm skin incision is made, approximately 2 to 3 cm lateral and parallel to the deltopectoral interval, beginning at the level of the coracoid and extending distally toward the midhumerus (Fig. 41-1). The lateralized skin incision ensures that the cephalic vein can be quickly identified on the medial side of the wound. A lateralized incision also improves visualization of the glenoid and improves scar formation. After superficial dissection, the cephalic vein is used to identify the deltopectoral interval, and the vein is retracted laterally as the interval is opened from the clavicle to the humerus. A curved retractor is used to retract the skin and deltoid muscle laterally, and a standard Hohmann retractor is placed behind the coracohumeral ligament superiorly.
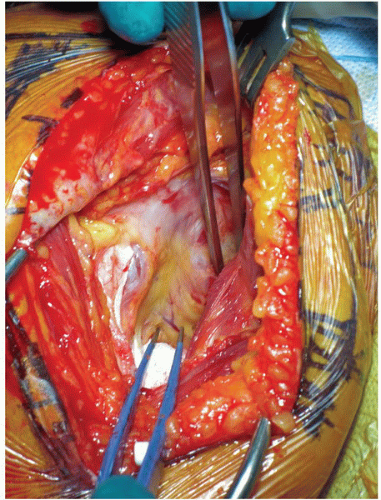
The clavipectoral fascia is sharply incised and a self-retaining retractor is then used to retract the conjoint tendon medially and the deltoid muscle laterally. Excessive retraction is avoided due to the risk of damage to the musculocutaneous nerve medially, behind the conjoint tendon. The superior border and inferior borders of the subscapularis tendon are identified, using the anterior circumflex humeral vessels as a guide to the inferior aspect of the tendon (Fig. 41-2).
Inferior Window
The inferior window is the first arthrotomy made and is used to expose the inferior aspect of the joint for removal of osteophytes. The inferior window can also be used to check component positioning during trialing
and insertion. The window is opened below the subscapularis tendon, medially as far as the glenoid and laterally to the tendon insertion of subscapularis.
and insertion. The window is opened below the subscapularis tendon, medially as far as the glenoid and laterally to the tendon insertion of subscapularis.
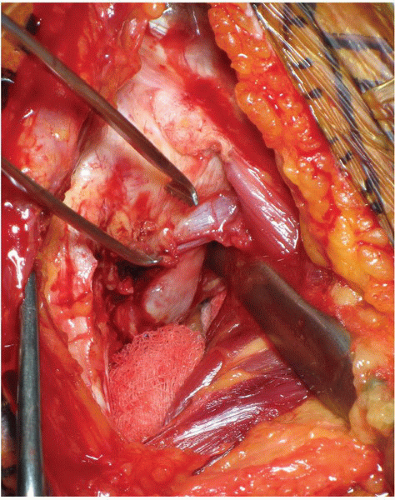
To open the window, a 1-cm partial tenotomy of the superior part of the pectoralis major tendon is performed, exposing the underlying latissimus dorsi tendon. The anterior circumflex humeral vessels are ligated and cauterized. The arm is then flexed to approximately 60 degrees and externally rotated approximately 20 degrees. The plane between the subscapularis tendon and the joint capsule is developed and the tendon is retracted superiorly, exposing the anteroinferior joint capsule (Fig. 41-3). The axillary nerve is located and exposed adjacent to the joint capsule inferior to the glenoid neck and a small Hohmann retractor is placed to protect the nerve.
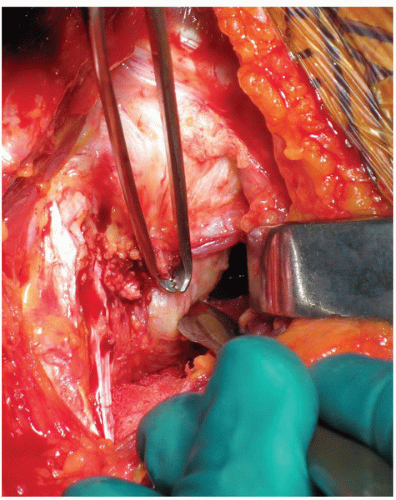
The inferior arthrotomy is then performed into the axillary pouch (Fig. 41-4).The capsulotomy is extended laterally along the capsular attachment to the humerus and medially along the glenoid neck, and the capsule is fully excised (Fig. 41-5). Once completed, a second retractor is placed at the inferior aspect of the humeral head exposing the osteophytes anteriorly and inferiorly. The osteophytes are resected using curved osteotomes and rongeurs (Fig. 41-6). Complete removal of the osteophytes can be confirmed by palpation. It is important to ensure that the posterior osteophytes, which are difficult to access, have been removed. After removal of the osteophytes, the inferior aspect of the glenoid can be visualized and an inferior soft-tissue release performed (Fig. 41-7). The position of the axillary nerve should be considered at all times during the capsulotomy and removal of the osteophytes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree