Minimally Invasive Plating of the Distal Tibia
Daniel J. Stinner
Michael J. Beltran
Cory A. Collinge
INDICATIONS
Minimally invasive percutaneous plate osteosynthesis (MIPPO) is a technique indicated for fractures of the distal tibial metaphysis, including those with simple involvement of the articular tibial plafond. This includes both low- and high-energy extra-articular metaphyseal fractures, and select high-energy axial loading plafond injuries (i.e., pilon fractures) without articular comminution (OTA type A and C1/2 fractures) (Figs. 13.1 and 13.2). While metadiaphyseal and metaphyseal distal tibia fractures may also be well treated with modern intramedullary nails—despite articular extension and short distal segments, recent literature has indicated a higher incidence of angular malalignment after nailing compared to plating, and anterior knee pain remains a common long-term outcome.1, 2 and 3 Strategies for minimally invasive surgery around the distal tibia are not new. External fixation has been used around the distal tibia with good results, where biology is preserved and stability provided by external fixation allows for early healing in most cases. The difference between internal and external fixation is in the risk/benefit profile, as well as the mechanics and the resulting healing process. For example, while scant metal is implanted at the fracture site with external fixation, pin problems exist, the fixator crosses the ankle making stiffness a concern, it requires removal, and high rates of malunion have been reported.
MIPPO of the distal tibia may be utilized when the surgeon desires either absolute or relative fracture stability based on the fracture pattern being treated. Noncomminuted oblique or spiral fractures with or without simple articular extension are well treated with absolute stability techniques and implants if they can be anatomically reduced. Adjuvant reduction tools (percutaneous clamps, joysticks, etc.) can often be used to help obtain an anatomic reduction, which is then stabilized with lag screws either through or outside of the plate. In the latter case, the percutaneous plate is applied in a neutralization mode. Highly comminuted fractures, conversely, are usually best managed with relative stability, and in these circumstances plates should be placed in a bridging mode. In these situations, the plate itself can be used as a reduction aid to restore mechanical alignment, in addition to other adjuvant reduction aids. In either circumstance, the goals of percutaneous fracture surgery are met—preservation of fracture biology and minimization of soft tissue complications.
Select situations pose particular challenges for distal tibia MIPPO, and under these conditions an alternative fixation strategy should be employed. Severe compromise of the distal leg soft tissue envelope, particularly medially, may increase the chances for infection and wound breakdown even when small incisions are used. Intramedullary nailing, open reduction through a different approach, or external fixation should be considered under these circumstances. Furthermore, type C3 pilon fractures with articular comminution are best managed, in most cases, with a fully open approach and anatomic reconstruction of the articular surface. This is especially true in the younger, more active population. Finally, simple fractures at the metaphysis or metadiaphyseal junction of the distal tibia, while amenable to MIPPO, may be well treated with intramedullary nailing. With intramedullary nailing, there may be theoretical benefit to apply a local bone graft in nailed distal tibias, as well as the ability to dynamically compress and load certain fracture patterns during weight bearing.
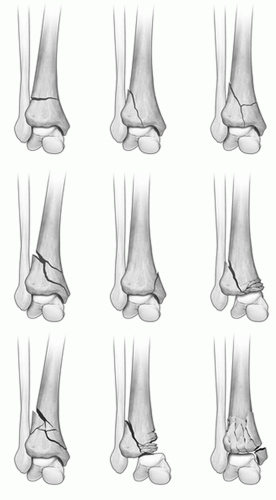 Figure 13.1 Orthopedic Trauma Association alphanumeric classification of distal tibia (43) fractures. |
 Figure 13.2 Illustrative case, a 43-year-old man with an OTA 43-C1 injury treated as demonstrated by associated figures. |
PATIENT POSITIONING
The patient is positioned in the supine position on a radiolucent table (Fig. 13.3). A small bump is placed under the hip to place the entire lower extremity in a neutral position, which aids in obtaining orthogonal radiographs and does not compromise the surgical approaches necessary for the technique. If the fracture is already spanned with an external fixator and the pins are ideally placed to aid in indirect fracture reduction, the bar and clamp components are removed and the pins prepped into the field. After prepping, we prefer to isolate the pin sites with small sponges to reduce contamination of the sterile surgical wounds.
SURGICAL APPROACHES
Approaches for MIPPO of the distal tibia include the workhorse medial approach and, less commonly, the anterolateral approach. Nearly all metaphyseal fractures can be managed via the medial approach. While large, open medial incisions have previously been associated with high wound complication rates, the small incisions, preserve biology, and careful soft tissue handling used in MIPPO techniques have not led to adverse soft tissue problems in larger series of patients.1,4,5
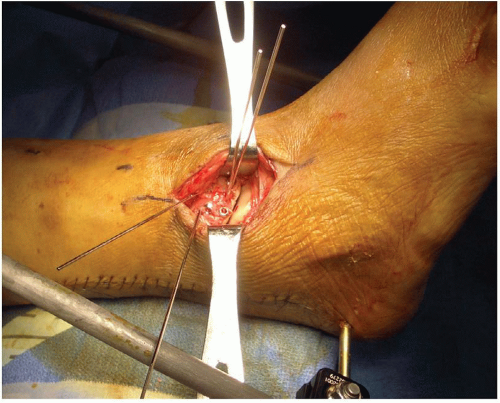
The medial approach involves a 2- to 3-cm incision at the tip of the medial malleolus, taking care to preserve the saphenous vein and nerve with the superficial dissection (Figs. 13.4 and 13.5). Once the dissection reaches the periosteal level, a subcutaneous, extraperiosteal tunnel is developed proximally using an elevator or the plate itself, taking diligent care to stay along the anteromedial face of the tibia and not deviate anteriorly or posteriorly. A small 2- to 3-cm proximal window is often helpful to pass the plate centrally on the medial tibia and ensure its proper proximal position.
We prefer the use of modern, precontoured, locking small fragment plates medially because they can be used as indirect reduction aids themselves and allow for fixed-angle stability when managing short metaphyseal segments. In contrast, nonlocking plates can be used and have been associated with good results in a recent series.1 If the surgeon is bending plates for the medial distal tibia, the local anatomy must be appreciated or else deformity may be imparted. While the coronal plane flare of the medial distal tibia is evident on an AP radiograph (an approximate 20-cm radius of curvature, Figure 13.6A), there is also torsional contour of the medial face of the distal tibia (Fig. 13.6B) that must be addressed. Mast has recommended bending 25 degrees of torsion into the plate, then using a bending press to apply a mild concavity to the plate. As a general rule, (1) the torsional bend is more important to the final reduction than the concavity and (2) the stiffer the implant, the more precise the bend must be or else deformity may be imparted. If the indirect reduction has already been obtained with other adjuvant measures, the plate is fixed proximally and distally with a combination of locking and nonlocking screws (i.e., hybrid plate constructs). In general, we prefer the use of locking screws in the distal metaphysis and nonlocking screws proximally.
 Figure 13.4 The anatomy is drawn out and a 2- to 3-cm incision at the tip of the medial malleolus is made for subcutaneous plate insertion. |
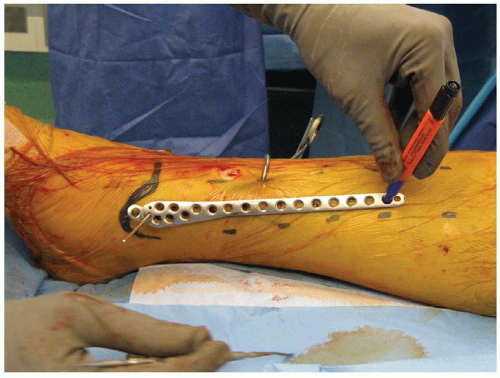 Figure 13.5 The plate itself can be used before its insertion to plan incisions. Alternatively, laying a similar plate over the inserted one, allows for marking the incisions. |
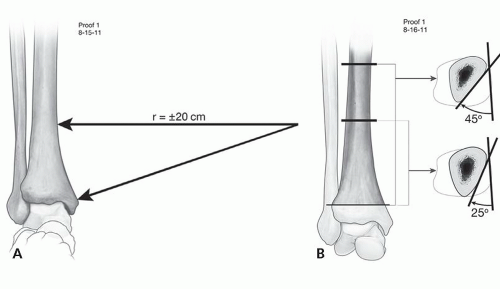 Figure 13.6 The distal tibia’s bony anatomy includes (A) the flare of the medial supramalleolar at 20 cm, and (B) in internal torsion of 20 to 25 degrees. |
When the fracture pattern is simple and amenable to compression, we recommend obtaining distal fixation first then compressing the fracture with either a lag screw tangential to the fracture, with axial compression using an eccentrically drilled hole through the plate, or with the use of an articulated tensioning device. For comminuted fractures in which the plate will be used as a reduction aid, screw placement strategy is variable and depends on the fracture pattern and displacement vectors being reduced (see next section).
The anterolateral approach is particularly useful for pilon fractures with a simple anterolateral articular fracture lines. The incision is 3 to 4 cm in length and centered between the fibula and tibial crests generally in line with the fourth ray and directly over the tibiotalar joint (Bohler incision, Figure 13.7). Care must be exercised with the superficial dissection to avoid injury to the superficial peroneal nerve, which often crosses in the field. The extensor retinaculum is incised and isolated as a separate layer for closure to avoid tendon bowstringing. The underlying extensor digitorum brevis may be gently mobilized laterally in the distal aspect of the incision, if necessary. Capsulotomy exposes the anterolateral plafond, and exposure medially along the anterior surface is necessary to place screws through the anterior plate holes. Anterolateral plates from most manufacturers involve locking anterior to posterior options. After anatomic reduction of the articular surface, the plate can be slid proximally again in an extraperiosteal, submuscular tunnel along the lateral aspect of the tibia deep to the anterior compartment. Unlike the medial approach, the anterolateral MIPPO approach requires a separate proximal incision to identify and protect the deep neurovascular structures, which are intimately related to the anterolateral tibia at this level. These structures may be compressed under the plate, or injured by percutaneously applied screws if not carefully protected.6 Because of the anterolateral leg muscles proximally, anterolateral plates are difficult to use as reduction aids, and are most often placed after other reduction techniques have been used.
Reduction Techniques
Fracture reduction and implant insertion, while leaving a small surgical “fingerprint,” is the art that complements the science of fracture fixation. Indirect fracture reduction is used to avoid disruption of the fracture environment and to avoid soft tissue problems. Below we present our reduction methods for treating distal tibia fractures using MIPPO technique.
For fractures with intra-articular extension, direct or indirect reduction of major articular fragments is performed preceding metaphyseal fracture fixation. Open versus closed reduction of the joint is dictated by the injury pattern, soft tissue concerns, and patient factors. Indirect reduction of the articular surface may be attempted using percutaneously placed clamps, joysticks, lag screws, or manipulation with a freer elevator. MIPPO can then be performed. We feel strongly that anatomical reduction of the articular surface with rigid internal fixation using lag screws is the mainstay of treatment for articular injuries.
The authors use an algorithm for the reduction of metaphyseal distal tibia fractures to regain appropriate length, axial alignment, and rotation across the metaphyseal fracture.
 Figure 13.8 An external fixator in traction or femoral distractor is nearly universally helpful at gaining and holding length and gross reduction.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|