Minimally Invasive Operative Treatment of Displaced Midclavicular Fractures with a Titanium Elastic Nail
Axel Jubel
INDICATIONS (Table 7.1)
Elastic Stable Intramedullary Nailing (ESIN) is indicated in displaced fractures of the central third of the clavicle (Allman type I)1 in skeletally mature patients. Displacement is defined as the absence of cortical contact between the main proximal and distal fragments. Conservative treatment of displaced fractures in adults is associated with an increased risk of malunion and nonunion.2, 3, 4 and 5
In polytraumatized patients, operative stabilization of mid-third clavicle fractures may be necessary to facilitate nursing and to maximize the recovery and rehabilitation potential. In open clavicle fractures, fracture stabilization should be done after soft tissue and osseous debridement to reduce the incidence of infection. In fractures with associated vascular injury, ESIN is indicated after vascular repair, to prevent repair damage by fracture motion. Patients with additional lower extremity fractures that do not allow full weight-bearing can be mobilized on crutches after operative stabilization with an elastic titanium nail.
Regarding the fracture pattern, strong indications for ESIN are all types of simple fractures (two fragments) and simple wedge comminuted fractures.6, 7 and 8 According to the OTA/AO classification system9,10 the indications for ESIN comprise type B1 and type B2 fractures which correspond to type 2B1 fractures of the Robinson11 classification system.
Indications for ESIN in complex or comminuted fractures (type B3 of the OTA/AO classification or type 2B2 of the Robinson classification system) or fractures of the proximal or distal third of the clavicle (Allman type II and III)12 are less clear. In these patterns, there is a high risk of secondary shortening due to the fact that this implant is not interlocked and is length unstable, relying on intact cortices to prevent shortening. These fracture patterns are typically treated with plate fixation.8 In proximal and distal third clavicle fractures, generally there is not sufficient length of the short fragment to provide stable fixation of an intramedullary implant.
Accurate radiographic assessment of the clavicle is essential for correct analysis of displacement and the fracture type. The clavicle should ideally be radiographed in two projections: Upright anteroposterior with the arm hanging to allow gravity to demonstrate true displacement of the fragments, and 30 to 45 degrees craniocaudal tilt projection. The fracture can then be correctly classified according to the OTA/AO or Robinson classification system and the treatment indications determined.
The ESIN procedure is also indicated in symptomatic hypertrophic nonunions after midclavicular fractures as an alternative to plate fixation,13 whereas pathologic fractures and fractures in osteoporotic bone are best treated with plate fixation.
TABLE 7.1. Indications | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
PATIENT POSITIONING
The patient is positioned on a radiolucent operating table in the supine position. Clear intraoperative imaging in two orthogonal projections must be possible, which can be particularly difficult with the patient in the beach chair position. An image intensification device or C-arm is mandatory for correct placement of the titanium nail. A folded, soft radiolucent bump placed under the scapula allows for shoulder retraction, facilitating both closed and open reduction.
To have sufficient room to rotate the image intensifier, the table must be positioned such that the C-arm can be brought in ipsilateral to the fracture. This may require rotating the OR table so that the patient’s head is directed toward the middle of the operating room and the table pushed on its stand also toward the middle of the room (Fig. 7.1). Thus, the clavicle can be imaged in two planes perpendicular to each other (craniocaudal and caudocranial). These are similar to pelvic inlet and outlet views. Long ventilation tubing may be necessary for this position. The anesthesiologist and anesthesia machine are placed at the foot of the patient. Alternatively, the table may remain straight with the patient’s head at the anesthesia machine, the patient’s healthy arm tucked by the side, and the C-arm brought in from the contralateral side. The downside of this positioning is the surgeon needs to work under the C-arm.
The arm and the entire shoulder girdle on the injured side is sterilely prepared and draped, including the sternal notch medially (Fig. 7.2). This allows the arm to be manipulated to facilitate indirect reduction maneuvers. The arm is initially placed beside the body. The surgeon stands on the uninjured side to introduce the nail from medial to lateral. The assistant and the base of the C-arm are positioned on the injured side.
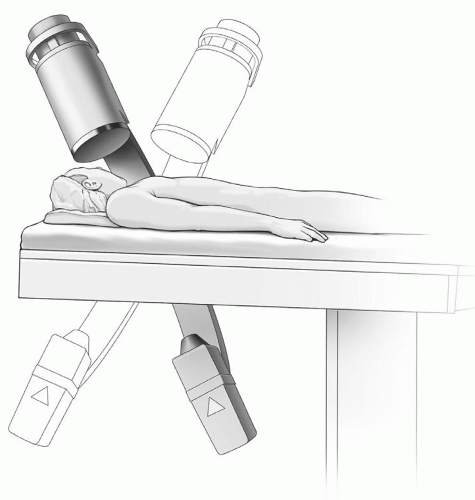 Figure 7.1 The patient is positioned supine on a radiolucent table. The C-arm is brought in from the ipsilateral side and tilted cranial and caudal to obtain near orthogonal views of the clavicle. |
 Figure 7.2 The patient’s entire upper extremity, including the contralateral sternoclavicular joint, is prepared and draped. |
SURGICAL APPROACH
A skin incision of 1 to 2 cm is made just lateral to the sternoclavicular joint (Fig. 7.3). By applying manual pressure on the supraclavicular fossa, the skin is displaced cranially preventing the incision from being directly over the end of the nail. The subcutaneous fat is dissected down to the clavicle with scissors and the ventral cortex of the clavicle is exposed without disrupting the periosteum. Two small Langenbeck retractors are inserted and the superior and inferior margins of the sternal clavicle are identified. Approximately 2 cm lateral to the sternoclavicular joint, a 2.5-mm drill guide is placed over the center of the clavicle, and a unicortical hole is drilled into the ventral cortex (Fig. 7.4). At this position, the ventral clavicle cortex is enveloped by skin and subcutaneous tissue only. There are no muscle fibers or tendinous origins or insertions. The apex of the dome-shaped cortex is identified to ensure the drill is positioned in the center of the radius. This minimizes the risk of perforation of the posterior cortex. The 2.5-mm drill hole is then enlarged using a 30-degree angulated awl.
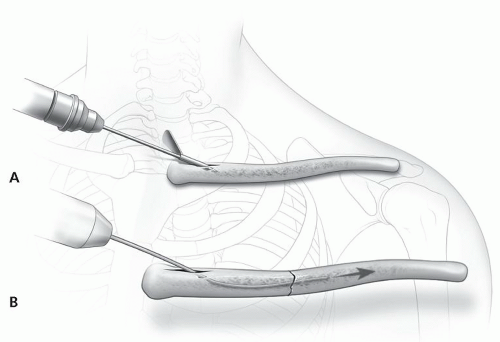 Figure 7.4 A 2.5- or 3.5-mm drill is inserted unicortically at a laterally directed 45-degree angle (A). This serves as the eventual nail insertion portal (B). |
OPEN REDUCTION
Closed reduction maneuvers are attempted initially. Shoulder retraction can provide a distraction force at the fracture site, restoring length. Typically the medial fragment is displaced proximally due to the pull of the strap muscles, and manual force can help restore this deformity. Fractures that are over 1-week old can be difficult to reduce with closed methods.
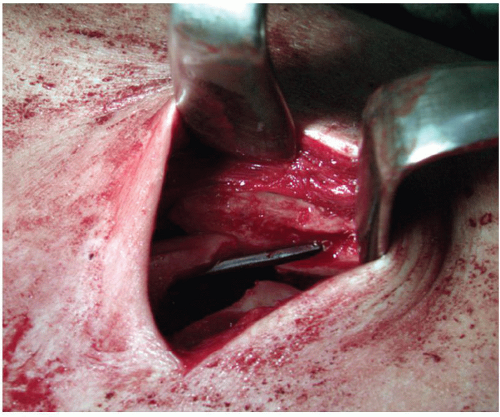
If closed reduction is unsuccessful, a 2- to 3-cm long additional incision is made in the Langer line at the lateral end of the medial main fragment. The subcutaneous fat is incised together with the underlying platysma muscle leaving thick soft tissue flaps. With acute fractures, the platysma muscle, the fascia, and the periosteum over the fracture site are often disrupted and do not require any further division (Fig. 7.5). The middle branches of the supraclavicular nerve run under the platysma muscle. There is no need for dissection of these nerves. Together with the platysma muscle the branches can be secured under a small Langenbeck retractor or a lid hook. In some cases they need to be incised to obtain optimal access to the fracture site. In many cases, trapezius muscle fibers are interposed between the main fragments. These muscle fibers are carefully removed using an elevator. Muscle and soft tissue attachments are elevated only as needed to visualize the fracture site. Small butterfly fragments usually found anteriorly should be left intact to their soft tissue attachments.
REDUCTION TECHNIQUES AND FIXATION
Acute Fractures
Under image intensification the smallest diameter of the medullary canal is estimated to assure correct nail size. As a general rule, the nail diameter should be two-thirds of the narrowest diameter of the medullary canal. If the fit is too loose, fixation may be compromised and migration or secondary loss of reduction is possible. If the fit is too tight, iatrogenic comminution or difficulty inserting the nail may occur. Generally a 2.5-mm diameter nail (in women) and a 3-mm diameter (in men) provide sufficient stability.
For insertion, the titanium is mounted on a Jacobs chuck with a T-handle or a specialized insertion chuck (Fig. 7.4B). With oscillating movements by the surgeon’s hand, the nail is advanced up to the fracture site without perforating the cortex. The bent tip of the nail acts as runner and prevents penetration of the dorsal cortex (Fig. 7.6). To ensure correct placement of the nail, fluoroscopic control is used. During nail passage through the medial fragment, the angled nail tip typically needs to be angled anteriorly to “bounce” of the posterior cortex, due to the anterior starting portal.
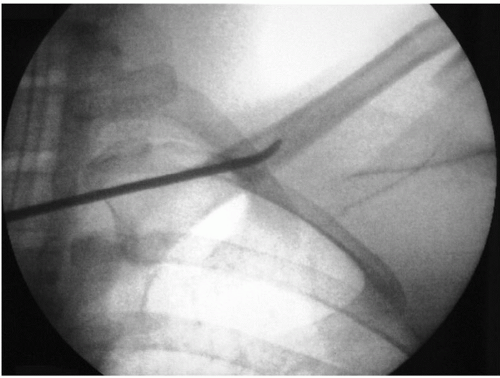 Figure 7.6 Fluoroscopy taken immediately after insertion of the nail into the medullary canal. The tip serves as a runner and prevents perforation of the opposite cortex. |
The reduction is effected indirectly by manipulation of the medial fragment with the nail mounted on the chuck. The chuck acts as a joystick and the lateral end of the medial fragment can easily be moved in all directions. The manipulation of lateral fragment is effected by moving the free draped arm. External rotation of the arm leads to an anterior movement of the medial end of the lateral fragment, whereas internal rotation results in posterior translation. External rotation and elevation of the arm leads to a dorsal rotation and caudal movement of the lateral fragment. Forearm traction in a caudal direction and adduction leads to cranial displacement of the medial end of the lateral clavicle. Depending on the required displacement, the arm is manipulated by the assistant, while the surgeon manipulates the medial fragment with the chuck. In addition, the bent tip of the nail can be used as a reduction finger. The accuracy of the reduction can be directly visualized or palpated and secured under the skin between the thumb and the index finger. Serrated reduction forceps that crush the periosteum should be avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree