Nerve root pain such as sciatica or femoral neuropathy may be related to a lumbar neurinoma . To our knowledge, meralgia paresthetica (MP) caused by lumbar neurinoma has never been described. We report a case of MP with back pain related to an L2-level neurinoma seen on MRI, the best investigation to explore the roots of the cauda equina and spinal cone and specify the foraminal extension. This pseudo-MP can be explained by 2 mechanisms: the theory of recovery by Ribuffo et al. and a mechanism related to the cluneal nerves.
1
Case report
A 50-year-old Arabic man, a sedentary office worker with no unusual medical history, had 6 months previously experienced low back pain, then 1 month later, bilateral radicular pain covering the trochanteric region. The pain was excrutiating, with mixed burning and tingling, and no associated signs. The symptoms were accompanied by insomnia and weight loss of 12 kg over the 6 months.
Examination revealed lumbar spinal rigidity. The DN4 neuropathic score was 7/10. The patient had no evidence of progressive nerve root damage. Moreover, neurologic and perineal examinations were normal. Lumbar spinal radiographs showed no signs of spinal disc disease, osteoarthritis or abnormal curvature; biologic examinations revealed no inflammatory syndrome.
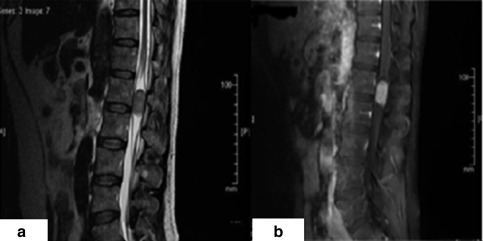
Medical therapy and rehabilitation did not improve the condition. MRI revealed a swelling next to the L2 vertebra in the intraductal posterolateral left position without foraminal extension. The intradural, oval, tissue lesion measured 3 cm on its vertical axis. The process was isointense in T1- and T2-weighted images, partly repressing the roots of the cauda equina, with intense homogeneous increased signals on gadolinium injection ( Fig. 1 a and b ). Motor and sensory nerve conduction of the lower limbs was normal, and sensory conduction velocity in the region of the lateral cutaneous nerve of the thigh (formerly femoral cutaneous nerve [LCNT]) was normal. The diagnosis of a schwannoma was confirmed by postoperative pathology.
Symptoms improved immediately after tumor resection, with no postoperative complications. Indeed, the pain completely disappeared on the right side; but a neurologic residual pain persisted on the left trochanter, 2/10 on a visual analog scale and DN4 score. The pain responded well to pregabalin, 150 mg/d. After 4 months, both the patient’s condition and sleep were improved. Ear, nose, and throat as well as skin and eye examinations did not reveal neurofibromatosis lesions.
2
Discussion
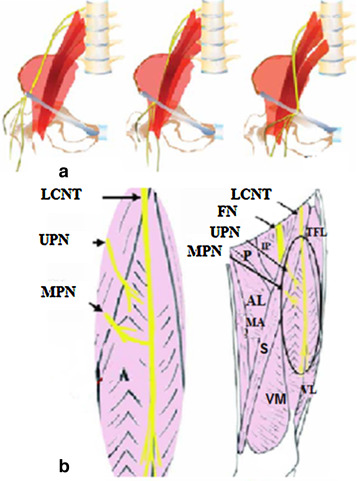
We describe a case of MP at the pre-trochanteric level somewhat resembling the symptomatic distribution of LCNT injury. The latter injury involves 2 branches: a posterior (gluteal) branch that leads to the greater trochanter and innervates part of the buttock and posterior thigh, and an anterior (femoral) branch that ensures the innervation of the anterior and external regions of the thigh . However, researchers have demonstrated variability in the nerve’s course as it exits the pelvis. Anatomic and clinical studies have demonstrated a variable course of the LCNT during its passage through the inguinal ligament . The nerve could pass just near the anterior superior iliac spine. In the latter case, the nerve is distributed more laterally at the thigh ( Fig. 2 a ) .
Neuromas contribute to the genesis of low back pain, sciatica and cruralgia . Often neuromas express as lumbosciatica, which is difficult to distinguish from common sciatica due to disc herniation in the differential diagnosis . MP symptomatic lumbar neurinoma is a possible etiology but to our knowledge has never been reported.
Two mechanisms can explain our case. The first is the theory of recovery by Ribuffo et al. , explained by the anastomosis or recovery of the LCNT by the posterior femoral cutaneous nerve (PFCN; formerly small sciatica) and the upper and middle perforating nerves from the femoral nerve ( Fig. 2 b) . The LCNT is a sensory nerve specifically arising from the dorsal lumbar plexus branches of L2 and L3 . The location of the sensory lesion at the side of the thigh is usual. PFCN arises from the S1 and S2 lumbosacral trunk and has 2 branches: motor (lower gluteal nerve) to the gluteus maximus, and sensory (dorsal cutaneous nerve of the thigh) from S2, whose terminal branches diverge toward the buttocks and dorsal femoral region. The presence of anastomosis can limit the deficit to an atypical small lateral or anterior territory . In addition, the area of skin innervated by the LCNT varies among individuals . Moreover, this nerve is absent in 5 to 10% of cases . In our case, the skin area was innervated by the femoral nerve .
In the second mechanism, the sensory innervation of the superior and lateral gluteal region is within the upper cluneal nerves from the dorsal rami of L1 to L3, where the neurofibroma in our case was located. Therefore, in our case, the MP is not relevant because of the location other than the LCNT.
Clinically, sensory and motor deficits are rare because of the nature of non-infiltrating tumors, which explains the normality seen on electromyography . The diagnosis of MP is sometimes difficult as compared with the locoregional disease initially diagnosed . In many cases, MP is idiopathic (61%) , but it can have another etiology . A proximal irritation of LCNT must always be sought if no improvement occurs after injection of an anaesthetic agent at the anterior superior iliac spine .
LCNT anatomical variations may present with different signs and symptoms. The knowledge of these potential variations can be useful in examination and management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




