The most common pathologic disorder affecting the medial clavicle is osteoarthritis.
Others include rheumatoid arthritis, seronegative spondyloarthropathies, crystal deposition disease, sternoclavicular hyperostosis, condensing osteitis, and avascular necrosis.12
Infection, although rare, must be considered. When suspected, the sternoclavicular joint should be aspirated for culture, Gram stain, and cell counts and then treated with irrigation and débridement.
Traumatic instability of the sternoclavicular joint is rare and classified by the direction of displacement of the clavicular head as superior, anterior, or posterior.
Posterior instability has been associated with a variety of potentially fatal comorbidities.
Atraumatic instability is usually anterior and is often seen in patients with generalized ligamentous laxity.
Symptomatic traumatic instability is best treated with closed reduction and possible reconstruction of the joint, not resection of the clavicle head.
The sternoclavicular joint is saddle-shaped and contains an intra-articular disc.22
Important ligamentous restraints to motion include the anterior capsule (restrains anterior and posterior translation), the posterior capsule (restrains posterior translation),20 and the costoclavicular ligament (which is the pivot point for motion in the axial plane).4
The interclavicular ligament seems to provide little function (FIG 1).
The anterior sternoclavicular ligament covers the disc and is the gateway into the clavicular and sternal side of the joint.22
Proximity to vital structures: brachiocephalic vein closest; common carotid (right) and aortic arch (left), next closest.17
Osteoarthritis is the most common cause for surgical excision.
Osteoarthritis is most commonly seen in male laborers, in women during the perimenopausal years, and after radical neck dissection.
Rheumatologic disorders can affect the sternoclavicular joint as part of the systemic disease. Involvement of the sternoclavicular joint is usually late.
Other atraumatic conditions are less common and the pathogenesis is largely unknown.
Traumatic instability typically develops from a blow to the shoulder girdle.
If the force impacts the anterior shoulder, it will push the shoulder girdle posteriorly. The clavicle pivots over the first rib, forcing the head of the clavicle anteriorly.
If the force impacts the posterior shoulder, it will push the shoulder girdle anteriorly. The clavicle pivots over the first rib, dislocating the head of the clavicle posteriorly.
Direct blows to the sternoclavicular joint can also dislocate the clavicle head posteriorly.
Atraumatic instability develops insidiously without a history of trauma.
Many people have asymptomatic sternoclavicular joint arthritis.
Patients with symptoms may find relief with activity modification and time. This is particularly true with the pain and swelling seen in perimenopausal women.
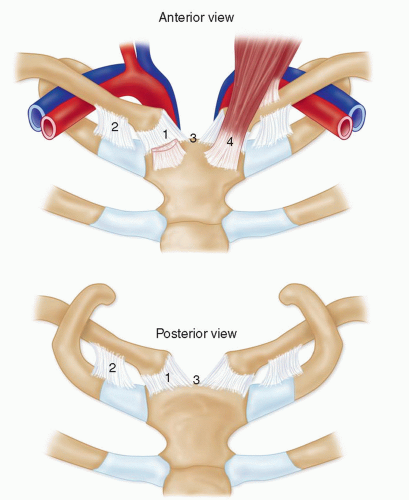
FIG 1 • Anterior and posterior anatomy of sternoclavicular joint. 1, capsule; 2, costoclavicular ligament; 3, interclavicular ligament; 4, sternocleidomastoid tendon.
Table 1 Clinical Features of Atraumatic Disorders of the Sternoclavicular Joint
Disorder
Age (y)
Gender
Side
Pain
Erythema
Associated Conditions and Risk Factors
Osteoarthritis
>40
M = F
B
+
Rare
Manual labor, radical neck dissection, postmenopausal women
Rheumatoid arthritis
Any
F > M
B
+
+
Symmetric polyarthritis
Seronegative spondyloarthropathies
<40
M > F
B
Occasional
−
Urethritis, uveitis, nail pitting
Septic arthritis
Any
M = F
U
+++
+++
HIV, IVDA, DM
Crystal deposition disease
>40
M > F
U
+++ during flare
++
Other joint involvement
Sternoclavicular hyperostosis
30-60
M > F
B
+
−
Synovitis, acne, pustulosis, hyperostosis, osteitis
Condensing osteitis
25-40
F > M
U
+
−
None
Friedreich disease
Any
F > M
U
+
−
None
Atraumatic subluxation
10-30
F > M
U
Infrequent
−
Generalized ligamentous laxity
M, male; F, female; B, bilateral; U, unilateral; IVDA, intravenous drug abuse; DM, diabetes mellitus.
Infection may present with a relatively benign clinical picture but will progress and may become serious.
It is rare for the sternoclavicular joint to be the primary joint involved in rheumatologic conditions or crystal deposition disease.
Traumatic instability may result from high-energy injuries (eg, motor vehicle collision) or may be related to contact in athletics.
Traumatic intra-articular fracture of the medial clavicle is also commonly associated with high-energy injury and a 20% 1-month mortality rate from multisystem trauma.21
Posterior instability may be life-threatening as the clavicular head may compress vascular structures, the trachea, or the esophagus.
Atraumatic instability may have an insidious onset and is often associated with other signs of generalized ligamentous laxity (eg, patellar subluxation, glenohumeral subluxation).
Atraumatic disorders
Localized sternoclavicular joint pain, potentially referred up the sternocleidomastoid and trapezius11
Infection is typically unilateral with pain and significant erythema (Table 1).
Osteoarthritis, rheumatoid arthritis, seronegative spondyloarthropathies, and sternoclavicular hyperostosis are typically bilateral, with mild pain and rare erythema.
Crystal deposition diseases, condensing osteitis, and Friedreich disease are typically unilateral and mildly painful.
Traumatic disorders
Acute trauma presents with pain and unwillingness to raise the arm. Patients may describe difficulty with swallowing or breathing with posterior dislocations.
The sternoclavicular joint is often swollen and tender.
If vascular compression is present, the affected arm may demonstrate circulatory changes and swelling.
Physical examination may not be helpful in determining if the instability is anterior or posterior.
Special radiographic projections include the Rockwood (serendipity), Hobbs, Heinig, and Kattan views but are somewhat difficult to interpret (Table 2).9
Computed tomography (CT) is particularly useful in trauma as it demonstrates displacement of the joint including direction (anterior or posterior) and bony anatomy.9
Arteriography should be considered in posterior dislocations if vascular injury is suspected.
Magnetic resonance imaging (MRI) is helpful in atraumatic disorders to evaluate the soft tissues and can delineate marrow abnormalities, joint effusions, and disc and cartilage injury.9
Laboratory findings in atraumatic disorders of the sternoclavicular joint are covered in Table 3.
Table 2 Radiographic Features of Atraumatic Disorders of the Sternoclavicular Joint | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








