Management of Simple Elbow Dislocation
Bradford O. Parsons
David M. Lutton
DEFINITION
Simple elbow dislocation is a dislocation of the ulnohumeral joint without concomitant fracture.
Complex instability denotes the presence of a fracture associated with dislocation.
The elbow is the second most commonly dislocated large joint.
PATHOANATOMY
Elbow stability is conferred by highly constrained osseous anatomy and the ligamentous anatomy.
The osseous architecture of the ulnohumeral joint, including the coronoid process and greater sigmoid notch of the ulna, and the trochlea of the humerus
The anterior band of the medial collateral ligament (aMCL) resists valgus stress. The aMCL originates on the anterior inferior face of the medial epicondyle and inserts on the sublime tubercle of the ulna.
The lateral ulnar collateral ligament (LUCL) resists varus stress. The LUCL originates from an isometric point on the lateral supracondylar column and traverses across the inferior aspect of the radial head, inserting on the supinator crest of the ulna.8 Unlike the aMCL, the LUCL originates in the precise center of rotation of the elbow; this is important when reconstructing the ligament.
Secondary stabilizers include the radial head and dynamic constraints such as the flexor and extensor muscles of the forearm.
When the elbow is extended, the anterior joint capsule contributes about 15% of varus-valgus stability.9
The radial head does not resist physiologic valgus stress in the presence of an intact aMCL; however, it plays a major role in the presence of aMCL insufficiency.
O’Driscoll has described the term ring of disability to describe series of pathologic events that result in ulnohumeral dislocation.
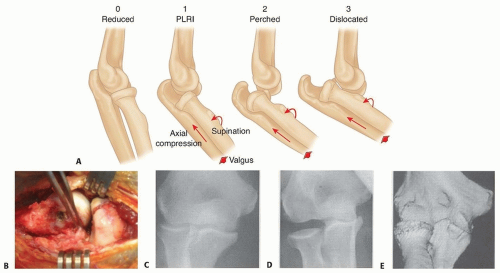
A simple elbow dislocation begins with an extension varus stress that disrupts the LUCL and progresses medially with tearing of the anterior and posterior capsules. This allows the ulna to “perch” on the distal humerus. Further soft tissue or osseous injury results in dislocation13 (FIG 1A).
Most traumatic injuries to the LUCL result in avulsion of the ligament from the lateral humerus (FIG 1B).
As forces continue from lateral to medial across the joint, the anterior and posterior capsular tissues and eventually the medial collateral ligament (MCL) may be disrupted; however, it is theoretically possible to dislocate the ulnohumeral joint with disruption of the LUCL and preservation of the aMCL.12
O’Driscoll et al12 has proposed the term posterolateral rotatory instability (PLRI) to describe the condition of chronic LUCL insufficiency resulting in rotatory recurrent ulnohumeral instability.
Fractures may occur with elbow dislocations, and the risk of recurrent instability increases significantly with complex dislocations. These fractures commonly include radial head or neck and coronoid fractures, although any fracture about the elbow may be observed.
Radial head fractures are usually readily apparent on plain radiographs.
Coronoid fractures may be subtle, and even a “fleck” of coronoid is often a hallmark of a more significant injury (eg, “terrible triad” injury), and its importance should not be underestimated.
Recently, a variant of elbow instability termed posteromedial rotatory instability (PMRI) has been described. PMRI is the sequela of a LUCL injury and a medial coronoid facet fracture. This injury pattern is most commonly observed without radial head fracture, making it potentially very subtle on plain radiographs. A computed tomography (CT) scan can delineate this injury in detail and should be obtained if any suspicion exists (FIG 1C-E).2, 11
ETIOLOGY AND CLASSIFICATION
Most elbow dislocations occur with a fall on an outstretched arm.
Forces of valgus, extension, supination, and axial compression across the joint can result in the ulna rotating away from the humerus, disrupting lateral anterior soft tissues initially, and dislocating the elbow.
Simple elbow dislocations are classified by the direction of displacement of the ulna in reference to the humerus, with posterolateral dislocation the most common.
Less common variants include anterior, medial, or lateral dislocations.
PATIENT HISTORY AND PHYSICAL FINDINGS
History is aimed at determining the timeline and mechanism of injury, frequency of dislocations, and previous treatment.
Unlike the shoulder, recurrent instability of the elbow is rare after an initial simple dislocation that was treated expediently.
Recurrent instability is more common in association with fractures (eg, the terrible triad injury).
Chronic instability, although rare in the United States, does occasionally occur, and management often requires reconstructive surgery or elbow replacement. Closed treatment is rarely successful in these patients.
Iatrogenic injury of the LUCL (during procedures such as open tennis elbow release or radial head fracture management) is a known cause of recurrent PLRI. However, these patients often complain of subtle lateral elbow pain due to subluxation of the joint with activities, such as rising from a chair, but rarely have recurrent dislocation.
Examination at the time of injury requires attention to the neurovascular anatomy.
Nerve injury can occur after elbow dislocation, and a thorough neurologic examination of the extremity is mandatory before any treatment of the dislocation.
Most nerve injuries are neurapraxia that often resolve.
The ulnar nerve is most frequently involved, although median or radial nerve injury may also occur.14
The dislocated elbow has obvious deformity, with the elbow typically held in a varus position and the forearm supinated.
After initial reduction, the neurovascular status of the limb is reevaluated. Loss of neurologic function after closed reduction is rare but can be an indication for surgical exploration to rule out an entrapped nerve.
Stability of the joint is assessed based on the amount of extension obtainable and association of pronation or supination with instability.
It is helpful to evaluate the stability throughout the elbow range of motion while the patient is still anesthetized, as this may guide treatment (examination under anesthesia).
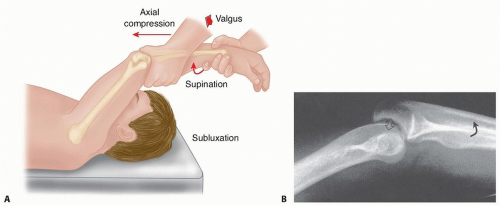
Stressing of the lateral soft tissues is performed with the lateral pivot shift maneuver, which can be performed under anesthesia and with fluoroscopic imaging12 (FIG 2).
This test can be used to assess the degree of PLRI and may aid in determining treatment.
Medial ecchymosis may be a sign of an aMCL injury and often is apparent 3 to 5 days after dislocation when the MCL has been injured.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard orthogonal radiographs of the elbow are obtained before and after reduction to assess for fracture and confirm relocation of the joint.
Congruency of the trochlea-ulna and radial head-capitellum is assessed.
Slight widing of the ulnohumeral joint (drop sign) or posterior displacement of the radial head relative to the capitellum should be noted.
Valgus stress views, once the joint is reduced, may help demonstrate an aMCL injury.
With the elbow flexed 30 degrees and the forearm in pronation, a valgus stress is placed under fluoroscopic evaluation to see if the medial ulnohumeral joint opens compared to the resting state.
Varus stress views are often not helpful.
CT scans with three-dimensional (3-D) reconstructions are obtained in any situation where a fracture may be
suspected, as it is critical to identify PMRI variants or subtle coronoid fractures, which may be an indication for surgical management.
Magnetic resonance imaging (MRI) is usually not necessary in the management of acute simple dislocation; however, it can be useful in the case of recurrent PLRI.
NONOPERATIVE MANAGEMENT
Most simple dislocations may be managed nonoperatively with splinting or bracing, guided by the degree of instability determined during the examination under anesthesia after reduction.12
Once reduced, elbow stability is assessed during flexion-extension in neutral forearm rotation.
If the elbow is stable throughout an arc of motion, it is immobilized in a sling or splint for 3 to 5 days for comfort and then range-of-motion exercises are initiated.
If instability is present in less than 30 degrees of flexion, the forearm is pronated and stability is reassessed.
If pronation confers stability, then a hinged orthosis that maintains forearm pronation is used, after 3 to 5 days of splinting, to allow protected range of motion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree