High-energy pelvic ring injuries can represent life-threatening injuries in the polytraumatized patient, particularly when presenting with hemodynamic instability. These injuries mandate a systematic multidisciplinary approach to evaluation, and timely intervention to address hemorrhage while concomitantly addressing mechanical instability. These pelvic injuries are associated with potentially lethal hemorrhage originating from venous, arterial, and osseous sources. A thorough understanding of anatomy, radiographic findings, and initial physical examination can alert one to the presence of pelvic instability necessitating emergent treatment. The focus is on hemorrhage control, using techniques for skeletal stabilization, angiography, and open procedures to decrease mortality in this high-risk patient population.
Key points
- •
Pelvic ring injuries vary in severity and are frequent in the polytrauma patient population.
- •
A subset of patients presenting with complex pelvic ring injuries and hemodynamic instability require special attention secondary to significant risk of mortality.
- •
Mortality is bimodal: acutely, from lethal hemorrhage, and late from complications of multiorgan system failure.
- •
A multidisciplinary approach, and prompt intervention through an algorithmic approach, are necessary to promote survival.
- •
An understanding of the roles of resuscitation, mechanical pelvic stabilization, angiography, and pelvic packing aid in caring for this subset of extremely injured patients.
Anatomy
Knowledge of pelvic anatomy is critical to the understanding of pelvic ring injury and treatment. This knowledge allows the surgeon to interpret the readily available bony imaging obtained during the initial trauma assessment, make inferences on pelvic ring stability, temporize life-threatening injuries, anticipate associated injuries, and ultimately definitively stabilize the pelvis to improve long-term functional outcomes.
The function of the pelvis is to transmit weight bearing from the proximal femur to the spine, primarily through the posterior pelvic ring, and to protect the pelvic soft tissue contents. The anterior pelvis, whose injuries are often more easily apparent, plays a secondary role in pelvic stability by functioning primarily as strut. In fact, isolated injuries of the rami or pubic symphysis have little effect on pelvic stability. Because pelvic ring stability is dictated primarily by the posterior ring structures of the sacrum, ilium, and sacroiliac joint, or a combination of these structures, determining stability first requires an understanding of the sacral osteology and the sacroiliac ligamentous complex that connects these entities.
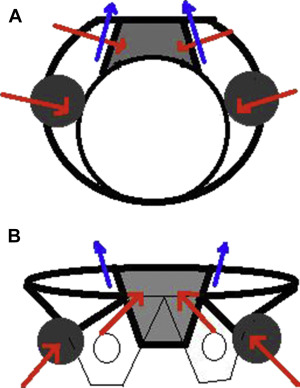
Pelvic osteology is best conceptualized on the inlet and outlet views. On the inlet view, the sacrum is shaped like a reverse keystone ( Fig. 1 A ) to resist the internal rotation vector during weight bearing in conjunction with the transverse oriented fibers of the posterior ligamentous complex and the anterior ring strut. On the outlet view, the sacrum is shaped like a true keystone ( Fig. 1 B) to resist the medially directed vector during weight bearing in conjunction with the longitudinally oriented fibers of the posterior ligamentous complex. It is easy to see that complete injuries of the sacrum, ligamentous complex, or ilium will result in posterior and cephalad displacement of the hemipelvis.
The posterior sacroiliac ligamentous complex is a collective term inclusive of the multiple ligaments that confer stability to the sacroiliac joints, connecting the ilium to the sacrum. Of these, the interosseous sacroiliac ligaments are the strongest and run transversely from the posterior superior and inferior spine of the ilium to the posterior sacrum. Posteriorly, the short and long posterior sacroiliac ligaments, collectively the posterior sacroiliac ligaments, run obliquely and longitudinally. The anterior sacroiliac ligaments pass transversely from the anterior sacrum to the anterior edge of the ilium ( Fig. 2 ). The sacrotuberous ligament is confluent with the posterior sacroiliac ligament and runs longitudinally to the ischial tuberosity ( Fig. 3 ) and forms the border of the greater sciatic notch along with the weight-bearing arch of the ilium. Another longitudinally oriented ligament is the sacrospinous ligament (see Fig. 3 ), which, as its name suggests, connects the sacrum to the iliac spine and forms the border of the lesser sciatic notch along with the ilium and sacrotuberous ligament. Finally, the iliolumbar ligament connects the L5 transverse process to the iliac crest (see Fig. 3 ).
The posterior ligaments contribute most to resisting forces across the sacroiliac joint and are known collectively as the posterior tension band. The transversely oriented fibers primarily resist rotational forces, whereas the longitudinally oriented ligaments are the primary restraint against vertical shear forces. The combination and degree of injuries to these ligaments, along with disruption to the sacrum or ilium, explains the wide spectrum of stability seen in pelvic ring injuries.
Knowledge of structures at risk for injury after a pelvic ring injury is essential because it directs the physical examination for life-threatening injuries and provides clues to pelvic stability for selecting provisional or definitive fixation.
Peripheral nerve deficit may occur with wide displacement of the hemipelvis and indicate the possibility of complete hemipelvis instability. The lumbosacral plexus ( Fig. 4 ) is derived from the anterior rami of the T12 to S4 nerve roots and courses anteriorly to the sacroiliac joint. The L4, L5, S1, and S2 nerve roots are of surgical importance because they may be injured with aberrant placement of sacroiliac screws during percutaneous fixation with sacroiliac screws or with open reduction and internal fixation of the sacroiliac joint.
Death from hemorrhage is the primary concern during the management of pelvic injuries in the unstable patient. Although blood loss is most commonly due to disruption of the pelvic venous plexus, injuries to the arteries of the pelvis can occur in isolation or combination (see Fig. 6 ). The median sacral artery, superior rectal, and iliac artery are the main arteries of the pelvis. However, it is injury to the internal iliac artery that most commonly results in early mortality.
Urethral tears, especially in males, are a common cause of comorbidity after pelvic trauma. Disruption of the sacrotuberous and sacrospinous ligaments during pelvic displacement may result in tension and injury to the pelvic floor. The urethra pierces the pelvic floor and is particularly vulnerable at this level, which may result in injury requiring repair.
Anatomy
Knowledge of pelvic anatomy is critical to the understanding of pelvic ring injury and treatment. This knowledge allows the surgeon to interpret the readily available bony imaging obtained during the initial trauma assessment, make inferences on pelvic ring stability, temporize life-threatening injuries, anticipate associated injuries, and ultimately definitively stabilize the pelvis to improve long-term functional outcomes.
The function of the pelvis is to transmit weight bearing from the proximal femur to the spine, primarily through the posterior pelvic ring, and to protect the pelvic soft tissue contents. The anterior pelvis, whose injuries are often more easily apparent, plays a secondary role in pelvic stability by functioning primarily as strut. In fact, isolated injuries of the rami or pubic symphysis have little effect on pelvic stability. Because pelvic ring stability is dictated primarily by the posterior ring structures of the sacrum, ilium, and sacroiliac joint, or a combination of these structures, determining stability first requires an understanding of the sacral osteology and the sacroiliac ligamentous complex that connects these entities.
Pelvic osteology is best conceptualized on the inlet and outlet views. On the inlet view, the sacrum is shaped like a reverse keystone ( Fig. 1 A ) to resist the internal rotation vector during weight bearing in conjunction with the transverse oriented fibers of the posterior ligamentous complex and the anterior ring strut. On the outlet view, the sacrum is shaped like a true keystone ( Fig. 1 B) to resist the medially directed vector during weight bearing in conjunction with the longitudinally oriented fibers of the posterior ligamentous complex. It is easy to see that complete injuries of the sacrum, ligamentous complex, or ilium will result in posterior and cephalad displacement of the hemipelvis.
The posterior sacroiliac ligamentous complex is a collective term inclusive of the multiple ligaments that confer stability to the sacroiliac joints, connecting the ilium to the sacrum. Of these, the interosseous sacroiliac ligaments are the strongest and run transversely from the posterior superior and inferior spine of the ilium to the posterior sacrum. Posteriorly, the short and long posterior sacroiliac ligaments, collectively the posterior sacroiliac ligaments, run obliquely and longitudinally. The anterior sacroiliac ligaments pass transversely from the anterior sacrum to the anterior edge of the ilium ( Fig. 2 ). The sacrotuberous ligament is confluent with the posterior sacroiliac ligament and runs longitudinally to the ischial tuberosity ( Fig. 3 ) and forms the border of the greater sciatic notch along with the weight-bearing arch of the ilium. Another longitudinally oriented ligament is the sacrospinous ligament (see Fig. 3 ), which, as its name suggests, connects the sacrum to the iliac spine and forms the border of the lesser sciatic notch along with the ilium and sacrotuberous ligament. Finally, the iliolumbar ligament connects the L5 transverse process to the iliac crest (see Fig. 3 ).
The posterior ligaments contribute most to resisting forces across the sacroiliac joint and are known collectively as the posterior tension band. The transversely oriented fibers primarily resist rotational forces, whereas the longitudinally oriented ligaments are the primary restraint against vertical shear forces. The combination and degree of injuries to these ligaments, along with disruption to the sacrum or ilium, explains the wide spectrum of stability seen in pelvic ring injuries.
Knowledge of structures at risk for injury after a pelvic ring injury is essential because it directs the physical examination for life-threatening injuries and provides clues to pelvic stability for selecting provisional or definitive fixation.
Peripheral nerve deficit may occur with wide displacement of the hemipelvis and indicate the possibility of complete hemipelvis instability. The lumbosacral plexus ( Fig. 4 ) is derived from the anterior rami of the T12 to S4 nerve roots and courses anteriorly to the sacroiliac joint. The L4, L5, S1, and S2 nerve roots are of surgical importance because they may be injured with aberrant placement of sacroiliac screws during percutaneous fixation with sacroiliac screws or with open reduction and internal fixation of the sacroiliac joint.
Death from hemorrhage is the primary concern during the management of pelvic injuries in the unstable patient. Although blood loss is most commonly due to disruption of the pelvic venous plexus, injuries to the arteries of the pelvis can occur in isolation or combination (see Fig. 6 ). The median sacral artery, superior rectal, and iliac artery are the main arteries of the pelvis. However, it is injury to the internal iliac artery that most commonly results in early mortality.
Urethral tears, especially in males, are a common cause of comorbidity after pelvic trauma. Disruption of the sacrotuberous and sacrospinous ligaments during pelvic displacement may result in tension and injury to the pelvic floor. The urethra pierces the pelvic floor and is particularly vulnerable at this level, which may result in injury requiring repair.
Clinical assessment
The clinical assessment of the patient is of utmost importance because the radiographic assessment most often underestimates the degree of pelvic instability seen at the time of injury owing to hemipelvis recoil, placement of a pelvic binder, and the reducing effect of the concave computed tomography (CT) table. The initial physical examination, as always, begins with a general assessment of the multiply injured patient as directed by the principles of Advanced Trauma Life Support (ATLS) guidelines. For the purposes of this review, discussion is limited to the examination of pelvic ring injuries in the polytrauma patient. Assessment begins with a history that will alert the examiner to potentially life-threatening injuries of the pelvis.
The mechanism of injury provides an overall assessment of the energy imparted to the patient, with high-energy mechanisms such as motor vehicle accidents, falls from considerable height, and industrial accidents resulting in the greatest degree of instability patterns. Determining the direction of force may help with assessing injury patterns. However, descriptions of the direction of force may confound the assessment because high-energy mechanisms often result in multiple force vectors with resulting combined instability patterns that may be overlooked. Also overlooked is the impact of the age of the patient. Pelvic ring injuries in the young require substantially high energy, and can call into question a seemingly low-energy injury mechanism. The elderly require a high index of suspicion, because although most pelvic ring injuries are due to bony insufficiency, high-energy pelvic injuries in the elderly have extremely high mortality. Medical history is also important, because it provides a risk assessment, particularly in patients with coagulopathy owing to disease or medication.
The examination begins with an interpretation of vital signs. Pelvic fractures are responsible for approximately 15% of deaths in the polytrauma population, of which acute hemorrhage is the most common etiology. Therefore, in the setting of the unstable patient, attention is turned to identify causes of hemorrhage. A systolic blood pressure of less than 104 mm Hg and need for transfusion in the trauma bay are independent predictors of pelvic fracture related arterial bleeding. The ATLS workup should exclude external, thoracic, and abdominal causes of hemorrhage. The presence of hemodynamic instability with a concomitant anteroposterior (AP) radiograph showing a displaced pelvic ring injury should prompt immediate intervention. It should be noted that a femur fracture, in isolation, should not cause hemodynamic instability, and should not draw attention from the pelvic ring injury.
The examination continues with inspection and palpation of the perineum, rectum, and vagina for open fractures, because open pelvic fractures, along with vascular injury, carry a 50% incidence of mortality. Contusions should be noted and provide clues toward instability patterns and alert the surgeon to Morel–Lavalle lesions. The urethra, especially in males, should be inspected for blood, because this finding may indicate a urogenital injury. Leg length discrepancy and rotation should also be examined and documented.
The pelvis should then be stressed with internal and externally directed force to feel for instability. This examination should be performed only once, because repeated examination may result in the loss of tamponade and hemodynamic instability in the presence of an unstable ring injury. Often, instability in the pelvis can be inferred from the initial pelvic radiograph. In this situation, “stress” evaluation of the pelvis may be unnecessary potentially avoiding disruption of early clot formation.
Neurologic examination is critical. A careful neurologic examination may reveal peripheral nerve deficiency caused by large displacement of the pelvis at the time of injury. In the absence of a known cause, this finding almost invariably indicates an unstable pelvic ring injury.
Radiographic assessment
The AP pelvis radiograph is part of the ATLS evaluation and provides the initial information needed to determine whether hemodynamic instability may be owing to a pelvic ring disruption. Significant pubic symphysis diastasis with resultant external rotation of the hemipelvis increases the pelvic volume and provides a large space for hemorrhage. Gross vertical displacement may also be seen, indicating pelvic instability. Other subtle signs of gross instability include ischial spine or sacral avulsion fractures (indicating sacrotuberous or sacrospinous ligament incompetence), or a fracture of the L5 transverse process, where the iliolumbar ligament attaches. Posterior ring instability can occur through either failure of the sacroiliac ligaments leading to a widened sacroiliac joint, through complete fracture through the sacrum at the S1 and S2 vertebral levels, or through fracture of the ilium. Although specific, the AP radiograph alone is not sensitive and requires inlet and outlet views to better demonstrate posterior and cephalad displacement, respectively.
CT scan of the chest, abdomen, and pelvis is performed routinely in the polytrauma patient after the primary and secondary surveys. The CT scan better characterizes the often difficult to visualize posterior pelvic ring injury compared with radiographs. Instability is characterized by complete fractures of the sacrum or ilium, or widening of the sacroiliac joint, and is most useful for preoperative planning of definitive fracture management. However, it should be noted that the standard pelvic radiographs offer a better assessment of gross pelvic rotation and posterior or cephalad displacement for determining the need for pelvic binder and/or traction in the acute setting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





