Management of Bone Loss in Primary Anatomic Shoulder Arthroplasty
Jason J. Scalise
Joseph P. Iannotti
INTRODUCTION
Total shoulder arthroplasty (TSA) for glenohumeral osteoarthritis (OA) has demonstrated excellent long-term clinical results and patient satisfaction.2,4,14,18,20 TSA can be a technically demanding procedure with respect to sufficient surgical exposure and soft-tissue balancing. Glenoid deficiency presents an additional challenge as the ability to securely implant a prosthetic glenoid in the correct orientation may be compromised. This has led some surgeons to favor hemiarthroplasty in such circumstances. Given that TSA has shown superior clinical outcomes when directly compared to hemiarthroplasty for OA, managing glenoid deficiency is important in promoting durable outcomes for TSA in cases of primary OA.4,14,18,22
BASIC CONCEPTS
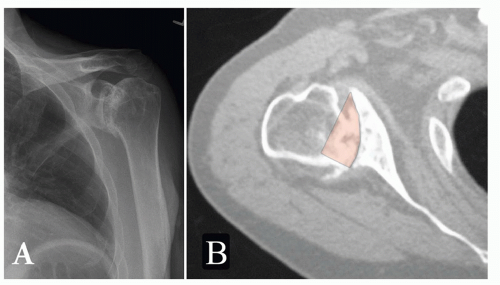
In the setting of OA, it is important to assess the degree and location of glenoid bone loss and any associated humeral head subluxation. Walch et al. introduced a classification system for glenoid wear in OA shoulders38 (Fig. 20-1). This scheme provides a conceptual framework that is helpful. In its basic form, it categorizes the glenoid as having central (concentric) or peripheral (eccentric) wear; types A and B, respectively. An additional component of the classification system is the extent of humeral head subluxation relative to the glenoid fossa. Typically with OA, anterior capsular tightness develops, which limits external rotation. This in turn promotes fixed posterior humeral head translation and may lead to preferential posterior glenoid wear, posterior glenoid bone loss, and an increase in glenoid retroversion. As described by Walch, the humeral head may only articulate with the posterior glenoid, resulting in a ridge separating the anterior and posterior glenoid, the socalled biconcave glenoid.
Within the Walch classification system, type C glenoids demonstrate retroversion greater than 25 degrees, regardless of the extent of humeral head subluxation. This may be seen in cases of glenoid hypoplasia where the posteroinferior ossification center of the glenoid fails to adequately form during development. Since the anterior ossification center forms normally, the resultant lack of posterior glenoid bone stock leads to substantial glenoid retroversion and often exceeds 25 degrees. A thick meniscoid posterior labrum complex typically develops in the place of the missing bony glenoid and reduces the tendency for posterior humeral head subluxation. This “soft-tissue glenoid” often degenerates in the third or fourth decade leading to early glenohumeral arthrosis associated with excessive glenoid retroversion.
When significant wear does occur in OA, it is often seen posteriorly. If not corrected, the increased glenoid retroversion may result in excessive and eccentric forces on the prosthetic glenoid, which risks premature implant failure.18,11,16,32,35,36
Different wear patterns can be encountered outside of classic OA. In general, inflammatory arthropathies are associated with a greater degree of centralized wear. Rotator deficient
arthritis typically shows superior glenoid wear. Chronic dislocations can lead to truly massive glenoid bone loss either anteriorly or posteriorly, depending upon the direction of the instability. Similarly, glenoid fossa fractures and the resultant post-traumatic arthrosis may present with large glenoid defects. Glenoid deficiency encountered in revision arthroplasty cases represent special challenges due to cavitary and segmental defects and are beyond the scope of the present discussion but are expertly discussed in Chapter 24.
arthritis typically shows superior glenoid wear. Chronic dislocations can lead to truly massive glenoid bone loss either anteriorly or posteriorly, depending upon the direction of the instability. Similarly, glenoid fossa fractures and the resultant post-traumatic arthrosis may present with large glenoid defects. Glenoid deficiency encountered in revision arthroplasty cases represent special challenges due to cavitary and segmental defects and are beyond the scope of the present discussion but are expertly discussed in Chapter 24.
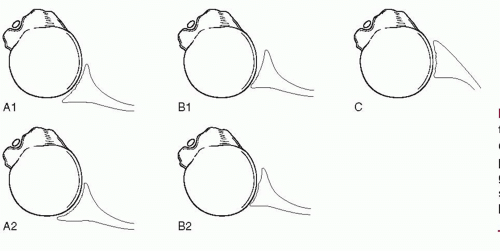 FIGURE 20-1. The glenoid wear classification described by Walch et al.38 The significant difference between types A and B is the presence of humeral head subluxation. The glenoid is classified as type C if retroversion is greater than 25 degrees, regardless of humeral head position. |
PREOPERATIVE EVALUATION
The preoperative evaluation of the extent of glenoid deficiency is a critical step in establishing the best method of surgical management or selection of a prosthetic component. An appreciation of the location and extent of glenoid wear is crucially evaluated in the preoperative setting. The main purpose of preoperative imaging in evaluating glenoid version and wear is to determine the strategies by which pathologic glenoid changes will be addressed intraoperatively. Increased glenoid retroversion, as is often encountered in glenohumeral OA, should be corrected toward more neutral version. This recommendation is based on the findings that excessive glenoid version will lead to higher shear forces on the prosthetic glenoid implant, resulting in early loosening and failure.25 Glenoid version can vary in normal individuals anywhere from anteverted to retroverted.6,8,9,10 The average glenoid tilt has been shown to be slightly retroverted in anatomic studies.6,37 Therefore, striving for glenoid version correction towards zero degrees of retroversion or slight retroversion in order to promote balanced compressive forces across the glenoid would seem to be a reasonable goal. It has not been established whether the component version should be corrected to a single position for all patients or individualized to the patient’s native premorbid version.
Nowak et al. demonstrated in a study of three-dimensional (3D) radiographic reconstructions that glenoid retroversion of 18 degrees or more leads to peg perforation of the glenoid prosthesis if the correction of the version to neutral was performed with anterior reaming alone.23 Iannotti et al. have shown that glenoid with 19 degrees of retroversion cannot be corrected to being perpendicular to the plane of the scapula without peg perforation.17 Similarly, Clavert et al. reported the results of a cadaveric study where correction of retroversion of 15 degrees or more by reaming along resulted in perforation of the peripheral pegs of the glenoid prosthesis.7 Excessive asymmetric reaming results in medializing the joint line by 1 to 2 cm and removes a significant amount of bone. Subsequent glenoid loosening will result in significant difficulty in managing the bone loss resulting from the combined effects of the original pathology, the loss from reaming, and the subsequent loss from having a failed component.
Plain radiographs will demonstrate the obliteration of the glenohumeral joint space and osteophytes characteristic of advanced OA. An axillary or West Point view must be included in any complete radiographic evaluation. This view demonstrates the glenoid profile in the axial plane and will demonstrate humeral head subluxation as well as pathologic glenoid version and erosions. Although plain radiographs may give a macroscopic appreciation of subluxation or glenoid wear, they are insufficient to accurately measure glenoid retroversion, to quantify bone loss, or to help detailed planning for a possible glenoid bone graft should that be necessary. Instead, computed tomography (CT) has been shown superior to plain radiographs in this regard3,12,24,38,40 (Fig. 20-2).
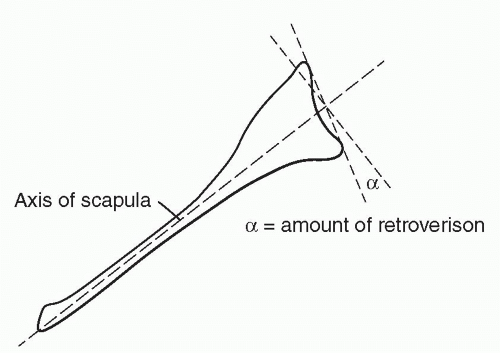
Friedman et al.12 described the most common method by which glenoid version is measured on conventional CT axial images (Fig. 20-3). On the mid-axial image, a line is drawn from the most medial aspect of the scapula body to the center of the glenoid fossa, bisecting a line drawn connecting the anterior and posterior margins of the glenoid fossa. The resultant angle represents the degree of glenoid tilt or version. As demonstrated by others subsequent to Friedman’s description, image acquisition perpendicular to the plane of the scapula is important for accurate version measurements and is contingent upon obtaining correct gantry of X-ray beam.3,30
Three-dimensional reconstructions of the 2D CT images can help to correct this common occurrence.27,30,40 The scapula can be rotated as a free body and viewed as a whole from any vantage using 3D images. The angle at which the images were acquired becomes irrelevant. Instead, the true plane of the scapula can be determined with the glenoid version accurately measured. Also, accurate measurements of the glenoid volumetric deficit are facilitated on the 3D views (Fig. 20-4).
New Methods to Measure Glenoid Bone Loss and Version
An idealized and consistent 3D model of the glenoid vault dimensions has been developed. It has been shown fit (in vivo and in a virtual environment) consistently within the glenoid
vault cavity and acts as a template (correcting for size) for normal vault anatomy and glenoid version. In severe cases of glenoid bone loss, it can be valuable as a guide for the reconstitution of the normal glenoid shape8,10,13,30,29 (Fig. 20-5).
vault cavity and acts as a template (correcting for size) for normal vault anatomy and glenoid version. In severe cases of glenoid bone loss, it can be valuable as a guide for the reconstitution of the normal glenoid shape8,10,13,30,29 (Fig. 20-5).
For example, correcting pathologic retroversion of 20 degrees to 0 degree of retroversion may overly correct a normal retroversion of 4 degrees. Overcorrection would result in some medialization of the joint line. As the medialization increases, the length-tension ratio of the rotator cuff worsens and may result in clinical weakness. Furthermore, perforation of the glenoid prosthesis may occur as the anterior-posterior dimensions of the vault decrease with progressive medialization. The ability to predict normal glenoid version for a particular individual using advanced techniques, such as the glenoid vault model, may demonstrate further clinical utility13 (Fig. 20-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree