Lower Extremity Considerations: Knee
Brian J. Cole
Richard Berger
Victor M. Goldberg
Aaron Rosenberg
Osteoarthritis of the Knee
Osteoarthritis (OA) of the knee is a disease with profound physical and economic impact. As the most common form of arthritis, it (along with hip OA) accounts for more dependency and disability of the lower extremity than any other disease. OA is considered a spectrum of cartilage failure ranging from the symptomatic focal chondral defect to established arthrosis. Clinically, OA consists of joint symptoms due to articular cartilage structural changes that are generally demonstrated on plain radiographs.1 OA is characterized pathologically as cartilage erosion, and it is defined epidemiologically through radiographic evaluation because this is the most readily available means to assess joints on a large scale. Not uncommonly, however, radiographic evidence of OA does not correlate with the patient’s symptoms.
The inability of cartilage to repair itself after traumatic injury and the progression of the untreated osteoarthritic process, once it is initiated, are discussed elsewhere in this book. The etiology of OA is controversial and seems to represent a combination of qualitative biologic change with loss of biochemical homeostasis and biomechanical failure of the joint cartilage due to physical forces. Independent of the etiology, OA is heralded by damage to the articular cartilage with diffuse fraying and fibrillation and hypertrophic changes in adjacent bone.
Epidemiology
The incidence and prevalence of OA in any joint are correlated with age. Before the age of 50 years, men have a higher incidence and prevalence, but after the age of 50 years, women have a higher incidence and prevalence. Gender differences increase progressively with advancing age until approximately 80 years.2
OA of the knee can be either primary or secondary. Primary OA is a progressive “wear and tear” degenerative condition that increases in prevalence nonlinearly with age after 50 years. It is estimated that 25% to 30% of people 45 to 64 years of age and more than 85% of individuals older than 65 years have radiographically detectable OA.3
Secondary OA of the knee may occur much earlier, however, after significant injury resulting in varus or valgus malalignment, intra-articular fracture, or ligamentous and meniscal deficiency.4,5 Rangger and colleagues6 reported radiographic increases in OA after partial arthroscopic medial (38% increase) and lateral (24% increase) meniscectomy at an average follow-up of 53.5 months in 284 consecutive patients. The effect of focal articular damage on joint function and the development of secondary OA is difficult to predict.7 The progression to arthrosis from focal articular damage is believed to be exacerbated when it is associated with meniscectomy.8
Cross-racial studies can often produce insights, but with respect to knee OA, there is conflicting evidence. The greater relative body weight of African-American women may predispose them to higher rates of knee OA. Generalized OA appears to have a strong genetic susceptibility, and knee OA may develop more as a function of inheritance than as a result of repeated mechanical insults or other lifestyle factors.9
The Framingham study demonstrated that men with jobs that require both carrying and kneeling or squatting have twice the risk of developing knee OA than that of men whose jobs do not require those activities. Elite athletes in several sports have increased risk of knee OA, even those without a history of injury.10 However, there is no evidence that recreational running predisposes to OA. Despite a lifetime of activity, no data to date support the development of or association with premature arthrosis of the knee in active patients.11
By any definition of OA, overweight individuals develop knee OA more often than do those who are not overweight.
Furthermore, studies confirm that increased weight precedes the occurrence of OA. Obese women with unilateral disease are at increased risk for development of bilateral disease, and overweight persons are at higher risk of experiencing progressive disease. These strong relationships between obesity and knee OA persist even when other factors associated with obesity are adjusted for. Weight loss has been associated with reduction in risk for development of symptomatic knee OA and improvement in symptoms in those with this condition.12
Furthermore, studies confirm that increased weight precedes the occurrence of OA. Obese women with unilateral disease are at increased risk for development of bilateral disease, and overweight persons are at higher risk of experiencing progressive disease. These strong relationships between obesity and knee OA persist even when other factors associated with obesity are adjusted for. Weight loss has been associated with reduction in risk for development of symptomatic knee OA and improvement in symptoms in those with this condition.12
The Meniscus and Osteoarthritis
It is estimated that the lateral meniscus normally carries 70% of the lateral compartment load and the medial meniscus 50% of the medial compartment load with the knee fully extended.13 The interrelationship between the loss of the load-bearing role of the meniscus after meniscectomy and the development of arthritis is well documented, with loads increasing up to threefold in the involved compartment.8,14,15 Patients who have had total meniscectomies have high risk of subsequent knee OA; those who receive partial meniscectomy also appear to be at increased risk.16 Not uncommonly, the young and previously active patient presents with disabling unicompartmental arthritis with progressive deformity as a result of previous subtotal or total meniscectomy. As discussed in the section on surgical options, these patients pose a treatment challenge with additional surgical options available, such as allograft meniscal transplantation, osteotomy, and unicompartmental knee replacement.
Biomechanics of Osteoarthritis of the Knee
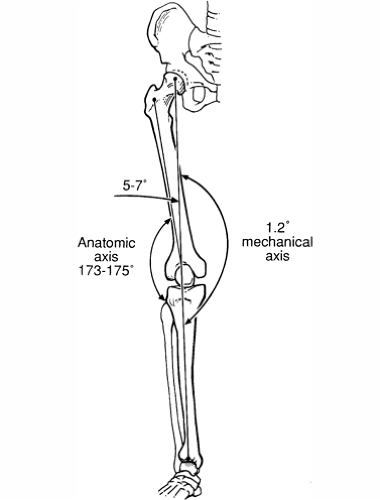
Standing weight-bearing anteroposterior radiographs that include both extremities from the hips to the ankles determine mechanical and anatomic axes of the limb. The mechanical axis is based on a line connecting the center of the femoral head and the center of the tibiotalar joint; it averages 1.2° of varus and generally passes through the center of the knee. The anatomic axis represents the longitudinal orientation of the femur with respect to the longitudinal orientation of the tibia; it is the angle formed by the intersection of the anatomic axes of the femoral and tibial shafts (Fig. 21B-1). The difference between the anatomic and mechanical axes is usually between 3° and 7°.17,18
A relatively neutral mechanical axis alignment allows the stress on the knee to be evenly distributed during weight bearing. With varus or valgus deformity, a line drawn between the center of the femoral head and the center of the ankle falls medial or lateral to the center of the knee, respectively. Therefore, in the varus knee, more forces are transmitted to the medial compartment; in the valgus knee, more forces are transmitted to the lateral compartment. This situation leads to a vicious circle once the arthritic process is initiated.
During activities of daily living, the knee is subjected to forces ranging between three and seven times body weight. Under these normal circumstances, the medial side of the knee is loaded about 50% more than the lateral side of the knee. This relative difference is due to the adduction moment normally produced at the knee during weight bearing and ambulation. These factors help to explain why 90% of knee arthritis begins in the medial compartment whereas only 10% of knee arthritis begins in the lateral compartment.
Conditions that increase the stress (or pressure) on the articular surface of the knee can lead to mechanical and biologic breakdown of the articular cartilage. Although the initiation of this process may be subject to conjecture or be purely idiopathic, once the process begins, progression of disease is affected by biomechanical abnormalities leading to relative increases in joint stress or pressure.
The interplay between biomechanical abnormalities and OA is complex and self-perpetuating. Factors such as primary articular cartilage degeneration, the effects of meniscectomy, and developmental deformities such as post-traumatic arthritis and fracture malunion often lead to a vicious circle of progressive degeneration with associated deformity.
Conditions such as a flexion deformity, which develops as a result of the arthritic condition, may similarly adversely affect the knee. For example, a flexion contracture of the knee reduces the contact area between the tibia and femur; this is because the largest area of contact between the tibia and femur occurs with the knee in nearly full extension and decreases with flexion. Therefore, fixed
flexion deformity, which is common in the arthritic process, can further accelerate the degeneration process by increasing the stresses across the knee as the forces are distributed over a smaller surface area.
flexion deformity, which is common in the arthritic process, can further accelerate the degeneration process by increasing the stresses across the knee as the forces are distributed over a smaller surface area.
Because individuals often compensate with the use of assistive devices, reduced activity levels, and adaptive changes in activities of daily living, progressive arthritis does not occur in all cases of abnormal knee biomechanics. Similarly, predicting who will develop progressive arthritis in the setting of abnormal biomechanics is difficult and dependent on many factors including genetics, habitus, activity levels, ligamentous stability, alignment, status of the meniscus, and overall condition of the articular cartilage.
Evaluation
There are several causes of knee arthrosis that are most often determined by the findings of the history, physical examination, and plain radiographs. If the findings are inconsistent, alternative diagnoses such as primary disease of the hip or back with referred pain to the knee, osteonecrosis, and stress fractures around the knee should be entertained. A complete history and physical examination of the spine, neurovascular system, and contiguous joints are imperative to avoid missing additional sources of knee symptoms.
History
A comprehensive history focusing on the patient’s symptoms includes factors commonly elicited during any evaluation of the musculoskeletal system (Table 21B-1). A patient’s employment, activity level, and symptoms are important factors in determining the appropriate treatment option. The patient’s occupation and current and desired activity levels are determined. Questioning the patient about activities that require adequate knee function, such as getting out of a chair or car, climbing stairs, and walking on level ground, provides insight into the patient’s ability to function on a daily basis.
Response to medical management (i.e., nonsteroidal anti-inflammatory drugs, analgesics, and injections) is sought. The response to modalities such as physical therapy, recent body weight or activity level changes, and assistive devices is reviewed.
Clinical Manifestations
The main symptoms of OA of the knee are joint pain and stiffness. The pain is generally related to activity and tends to worsen throughout the day. Rest pain implies severe OA, and sharp pains occasionally occur with particular activities. Pain localized to one compartment (i.e., unicompartmental) of the knee is common early in the disease process, especially in secondary OA. Alternatively, in long-standing OA, pain may be more diffuse. Atypical, severe pain should alert the clinician to other possibilities, such as osteonecrosis, inflammatory arthritis, or mechanical symptoms due to an intra-articular pathologic process (e.g., loose bodies, unstable meniscal or articular cartilage flap tears). In some patients with disorders of the spine and hip, pain can be referred to the knee. Patients with periarticular disorders such as anserine, infrapatellar, or prepatellar bursitis may be incorrectly diagnosed as having knee OA.
TABLE 21B-1 COMPONENTS OF A COMPREHENSIVE HISTORY | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stiffness in the morning is usual but brief, in contradistinction to inflammatory arthritis such as rheumatoid arthritis. The signs of OA include joint swelling, crepitus, reduced range of motion, pain on active movement and at the extremes of movement, and joint tenderness. A mild inflammatory reaction is sometimes present. Periarticular syndromes such as bursitis and tendinitis are common, as are muscle wasting and weakness. Weakness may be an important cause of both symptoms and disability.
Swelling related to a joint effusion or synovitis may be intermittent or constant. Small or moderate joint effusions are common; large effusions are rare. The synovial fluid has less than 2000 white blood cells/mm3, but cartilage fragments or calcium pyrophosphate crystals are common. Active OA results in the release of abnormal quantities of cartilage matrix molecules into the synovial fluid and in turn into blood.19 The value and meaning of these biochemical markers of OA are under investigation (see Chapter 12).
Mechanical symptoms of intermittent catching or locking may suggest gross articular surface irregularity, a loose osteochondral fragment, or meniscal disease commonly seen in secondary OA. It is important to consider the patient’s complaints of instability, pain, or a combination of both when ligamentous deficiency and arthrosis coexist. In addition, instability due to pain, effusion, and subsequent quadriceps inhibition is to be differentiated from instability due to ligamentous insufficiency, which may or may not be associated with pain.
Physical Examination
The components of a comprehensive physical examination are outlined in Table 21B-2. Body habitus and gait are observed. Antalgia, medial or lateral thrusts, and other dynamic compensatory gait patterns (quadriceps avoidance, out-toeing) are determined. Clinically, static limb alignment and deformity serve as a rough index of the duration and severity of the disease process. In long-standing primary OA or secondary OA after trauma or meniscectomy, genuvarum suggests medial compartment involvement and genu valgum suggests lateral compartment involvement. With long-standing deformity, patients may exhibit pseudolaxity due to stretching of the collateral ligaments on the contralateral side of the affected compartment.
TABLE 21B-2 COMPONENTS OF A PHYSICAL EXAMINATION | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Range of motion with side-to-side comparison is assessed in the supine and prone positions. Patients may commonly present with a mild flexion contracture (i.e., <10°) and lack full flexion (i.e., by >20°). Larger losses of motion are unusual in active individuals. Patients may complain of swelling or perceive stiffness due to swelling. Patellofemoral or joint line crepitus is a common finding.
Patellofemoral evaluation includes patellar tilt, lateral and medial patellar glide, and patellar facet tenderness as described in the section on anterior knee pain and patellofemoral disorders. Stability in the coronal plane (i.e., varus or valgus at 0° and 30° of flexion) and sagittal (anteroposterior) plane is determined. Positive results of the Lachman and pivot shift tests may indicate chronic anterior cruciate ligament insufficiency. Similarly, loss of the normal 5 to 10 mm of anteromedial tibial step-off relative to the medial femoral condyle or the presence of a tibial “sag sign” with the hip and knee held in 90° of flexion in the supine position may be indicative of chronic posterior cruciate ligament insufficiency.
Evaluation for joint line tenderness and swelling, and provocative meniscal tests such as the McMurray test are performed.20 The McMurray test is performed with the patient in the supine position with the hip and knee flexed to 90° while the axially loaded foot is maneuvered from a position of abduction and external rotation to one of adduction and internal rotation to elicit a painful “pop” or “click” in the affected compartment. The hip, back, and neurovascular status are evaluated for additional pathologic changes including losses in motion, with the need for radiographic imaging of these regions if a concomitant pathologic process is suspected.
Diagnostic Imaging
Plain Radiographs
Reproducible radiographs are examined in a systematic manner (Table 21B-3). Careful comparison of affected and unaffected knees helps to document subtle radiographic changes. A standard anteroposterior view with the patient
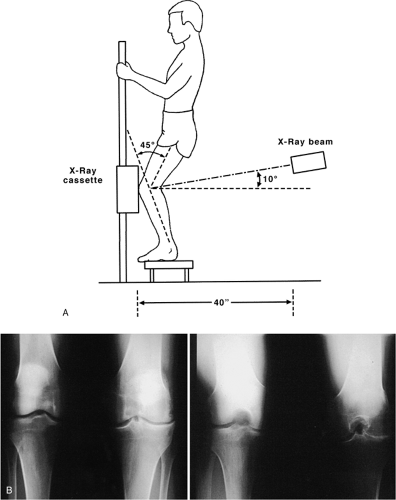
standing with the body weight evenly distributed on both legs is commonly obtained, but a 45° flexion weight-bearing posteroanterior radiograph as described by Rosenberg and colleagues21 is particularly valuable. In addition, a non-weight-bearing true 45° flexion lateral view and a 45° axial view of both patellae according to Merchant22 are obtained.
standing with the body weight evenly distributed on both legs is commonly obtained, but a 45° flexion weight-bearing posteroanterior radiograph as described by Rosenberg and colleagues21 is particularly valuable. In addition, a non-weight-bearing true 45° flexion lateral view and a 45° axial view of both patellae according to Merchant22 are obtained.
The 45° flexion weight-bearing posteroanterior radiograph may demonstrate subtle loss of joint space indicative of early arthrosis that traditional extension views fail to show (Fig. 21B-2), especially in the lateral compartment. The earliest loss of cartilage is typically in the 30° to 60° flexion zone and thus is easily overlooked with radiographs obtained in full extension. Symptoms of joint line
pain and a loss of cartilage clear space by 2 mm or more are likely to be due to chondrosis rather than meniscal disease.21 Because the 45° posteroanterior view provides a view of the notch, changes consistent with chronic anterior cruciate ligament deficiency are also evaluated, such as peaking of the tibial spines and narrowing of the intercondylar notch. Several important findings are determined from these views (Table 21B-4). For example, Fairbank23 changes seen after meniscectomy include osteophyte formation along the periphery of the tibia, flattening of the femoral condyles, and joint space narrowing.
pain and a loss of cartilage clear space by 2 mm or more are likely to be due to chondrosis rather than meniscal disease.21 Because the 45° posteroanterior view provides a view of the notch, changes consistent with chronic anterior cruciate ligament deficiency are also evaluated, such as peaking of the tibial spines and narrowing of the intercondylar notch. Several important findings are determined from these views (Table 21B-4). For example, Fairbank23 changes seen after meniscectomy include osteophyte formation along the periphery of the tibia, flattening of the femoral condyles, and joint space narrowing.
A history of prior meniscectomy, tibial plateau fracture, or clinically significant angular deformity is evaluated by standing, weight-bearing anteroposterior radiographs that include both extremities from the hips to the ankles to determine mechanical and anatomic axes of the limb (Fig. 21B-1).
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) scans of patients with knee arthritis are not routinely ordered. However, if there is a question of mechanical derangement such as a meniscal or cruciate ligament tear, or osteochondral fracture, osteonecrosis, or an isolated chondral defect, MRI may be informative. MRI is most useful in the setting of minimal arthritic change on radiographs in patients with localized pain and clinical findings consistent with meniscal disease. Not uncommonly, degenerative meniscal tears are present with OA, and one should avoid the temptation to operate solely on this finding without clinical correlation. Special MRI techniques to evaluate articular cartilage, including proton-density images, fat suppression or saturation techniques, and gradient-echo techniques with or without intra-articular gadolinium contrast enhancement, are gaining greater acceptance.24 In most cases, however, if joint space narrowing is present on the 45° flexion weight-bearing view, MRI is not indicated.
TABLE 21B-4 RADIOGRAPHIC FINDINGS | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Bone Scintigraphy
Technetium scintigraphy may be useful in difficult cases in which plain radiographs are normal despite a clinical scenario consistent with “arthritis-like” symptoms.25 For example, abnormal osseous activity detected by a bone scan (i.e., increased uptake in the patellofemoral compartment) may support findings of a periarticular pathologic process in the setting of a normal radiograph or normal findings on MRI. Abnormal findings on bone scans are likely in the presence of symptomatic OA, meniscal tears, osteonecrosis, and osteochondral lesions. Alternatively, diffuse soft tissue uptake may be associated with reflex sympathetic dystrophy.
Treatment Options
No treatment has yet been shown to definitively stop the osteoarthritic process; thus, the therapeutic goals must focus on reducing pain and improving function. Before considering therapeutic options in an individual with OA of the knee, the physician should be certain that the patient’s knee pain is attributable to OA. If the physician is in doubt about the diagnosis, consultation with a specialist is recommended.
TABLE 21B-5 NONSURGICAL MANAGEMENT OF OSTEOARTHRITIS | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Chronologic age is clearly only a relative consideration, and physiologic age often drives decision-making. Nonsurgical management (Table 21B-5) includes
nonpharmacologic (rehabilitation, lifestyle modification, shoe wear modifications, orthotics, bracing) and pharmacologic modalities. Intolerable lifestyle changes or a poor response to nonsurgical management may ultimately dictate surgical treatment.
nonpharmacologic (rehabilitation, lifestyle modification, shoe wear modifications, orthotics, bracing) and pharmacologic modalities. Intolerable lifestyle changes or a poor response to nonsurgical management may ultimately dictate surgical treatment.
Surgical modalities (Table 21B-6) include joint arthroscopy and reconstructive procedures (osteotomy, arthroplasty, arthrodesis, resection arthroplasty) and may include preventive measures, such as meniscal transplantation and articular cartilage restoration (marrow-stimulating techniques, osteoarticular allografts or autografts, and autologous chondrocyte implantation). Knowledge of the indications and outcomes for each of these procedures is important for appropriate management of the patient’s potentially unrealistic goals and expectations.
TABLE 21B-6 SURGICAL MANAGEMENT OF OSTEOARTHRITIS | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Nonsurgical Management
Nonsurgical therapy is divided into nonpharmacologic and pharmacologic modalities. The treatment plan is determined by numerous factors, including the presence of comorbid conditions, which may influence decisions about drug therapy. Details regarding nonsurgical approaches are provided in Chapters 14,15, 16 and 17.
Surgical Management
When nonoperative treatment of OA of the knee fails to alleviate pain and knee function is compromised, operative intervention is warranted. The timing of and recommendation for the most appropriate surgical procedure require great skill and cooperation between the patient and physician. Patients with severe symptomatic OA of the knee who have pain that has failed to respond to medical therapy and have progressive limitations in activities of daily living should be referred for surgical consideration (Table 21B-6).
Surgical options include arthroscopy and joint reconstruction. Joint reconstruction options include osteotomy, replacement, and arthrodesis. Joint replacement can be in the form of either unicompartmental or total knee arthroplasty. The symptomatic focal chondral defect limited to one of the femoral condyles or trochlea can be managed by a variety of techniques, and allograft meniscal transplantation may be a viable option when arthritis is unicompartmental and less severe.
The principles of management of the adult arthritic knee follow a relatively intuitive algorithm. Arthroscopy is primarily indicated as a first-time procedure in patients who often present with a relatively acute or subacute onset in pain. Mechanical symptoms caused by unstable articular cartilage flap tears, meniscal tears, or loose bodies are common indications to proceed with arthroscopy and débridement. To improve the prognosis after arthroscopy and débridement, patients should not have significant malalignment, ligament instability, or end-stage arthritis.
Osteotomy is principally indicated for unicompartmental arthritis and corresponding malalignment or for symptomatic post-traumatic malunions about the knee associated with painful knee arthritis. Unicompartmental knee arthroplasty is primarily indicated for the patient with lower physical demands and arthritis of a single compartment. Arthroplasty (total knee replacement) is indicated in the patient who is not a candidate for arthroscopy or osteotomy, in patients with more diffuse arthritic involvement, and for salvage of the failed osteotomy or unicompartmental knee replacement. Last, arthrodesis is most commonly indicated for the salvage of failed arthroplasty.
Arthroscopy
In OA, degenerating articular cartilage and synovium release proinflammatory cytokines (e.g., interleukin-1, tumor necrosis factor-α, transforming growth factor-β). These cytokines induce chondrocytes to release lytic enzymes leading to type II collagen and proteoglycan degradation. Arthroscopic lavage and débridement may “wash out” or dilute these inflammatory mediators.26 The effectiveness of joint lavage alone has been suggested by Livesley and colleagues.27 These authors compared the results of 37 painful arthritic knees treated with lavage by one surgeon with the results of 24 knees treated with physiotherapy alone by a second surgeon and suggested that there was better pain relief in the lavage group at 1 year. Edelson and coworkers28 demonstrated that lavage alone had good or excellent results in 86% at 1 year and in 81% at 2 years with use of the Hospital for Special Surgery score.
Jackson and Rouse29 reported the results of arthroscopic lavage alone versus lavage combined with débridement with 3-year follow-up. In the 65 cases treated with lavage alone, 80% showed initial improvement, whereas only 45% maintained improvement at follow-up. Of the 137 cases treated with lavage plus débridement, 88% showed initial improvement and 68% maintained improvement at follow-up. Gibson and associates30 demonstrated no significant improvement with either method, even in the short term. Patients who present with flexion deformities
associated with pain or discomfort with osteophyte formation around the tibial spines may benefit from osteophyte removal and notchplasty as demonstrated by Puddu and colleagues.31
associated with pain or discomfort with osteophyte formation around the tibial spines may benefit from osteophyte removal and notchplasty as demonstrated by Puddu and colleagues.31
The efficacy of lavage with or without débridement is controversial; some studies suggest that arthroscopic lavage and débridement, when appropriately indicated, will provide pain relief in 50% to 70% of patients lasting several months to several years (i.e., 2 to 4 years).32,33,34,35 In a recent Veterans Administration randomized trial comparing arthroscopic lavage, débridement, or sham procedures involving 180 patients, no statistically significant differences between study arms was demonstrated at a 2-year follow-up. Caveats related to the study included a 44% dropout rate; recruitment of only male patients; and nonspecific indications for surgical intervention.36 By contrast, Aaron reported a study of 122 consecutive patients who had failed conservative treatment and underwent arthroscopic débridement of the knee.37 At 34 months follow-up, 90% of the patients with objective mild arthritis demonstrated marked improvement by 6 months after surgery. However, there was little improvement in those patients with high grade OA according to clinical and radiographic signs. Specific débridement techniques such as microfracture when used for local cartilage defects may be very effective in preserving joint function.
Drilling and abrasion arthroplasty do not appear to offer additional benefit to arthroscopic débridement, although intermediate-term results in noncontrolled trials suggest that microfracture may offer some benefit.38,39 Arthroscopy is also a sensitive way to evaluate the extent and location of articular disease when osteotomy or unicompartmental knee arthroplasty is contemplated because plain radiographs and MRI often underestimate the extent of OA.40
Several factors may be relevant to prognosis after lavage and débridement (Table 21B-7). Those who appear to benefit most present with a history of mechanical symptoms, symptoms of short duration (i.e., <6 months), normal alignment, and only mild to moderate radiographic evidence of OA.32,33,34 It is not uncommon for patients to have unrealistic expectations after arthroscopic débridement. Thus, it is important to counsel patients about the limited indications and often palliative results. Patients who have undergone a minimum of 3 months of supervised nonsurgical treatment with normal alignment and only mild to moderate OA on 45° flexion weight-bearing posteroanterior radiographs may be considered candidates for arthroscopic débridement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree