Lower Extremity Considerations: Foot and Ankle
James Michelson
Overview of Osteoarthritis in the Foot and Ankle
Normal Biomechanics
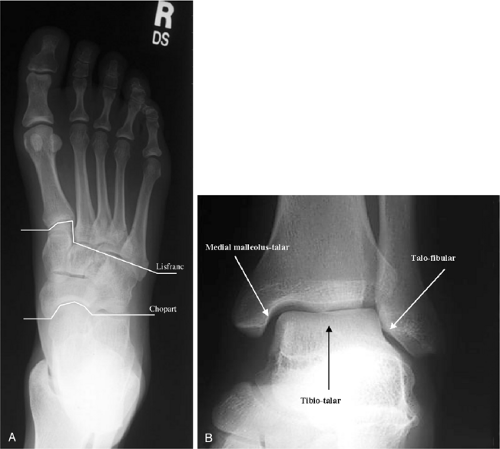
The entire complex of the foot and ankle encompasses 30 bones having 38 distinct articulations, all of which must work in smooth coordination to withstand peak loads in excess of one body weight for each normal stride. Relatively small alterations in the functioning of any of these articulations, such as in osteoarthritis (OA), can lead to significant disability (Fig. 21C-1). The joints in the foot and ankle have two functional roles: to bear load and to provide for motion. These two activities are interactive in the sense that an alteration in the range of motion of a given joint will alter its ability to bear load. Table 21C-1 summarizes the phases of gait during which there is load bearing for the various articulations in the foot and ankle and details the primary directions of motion. The gait cycle for walking is divided into a swing phase, when the limb is elevated off the ground, and a stance phase, during which the limb is in contact with the ground. The stance phase is further subdivided into heel strike, foot flat (or midstance), heel rise, and toe-off. The process of advancing from heel strike through toe-off requires motion of the foot and ankle complex in the sagittal plane to decrease the impact loading to the rest of the lower extremity. The inversion-eversion motion of the hindfoot and supination-pronation of the forefoot allow the foot to accommodate to uneven ground. It is considerably more difficult to walk on uneven ground, such as pebbles or grass, if the joints providing these functions (subtalar joint, transverse tarsal joint) are impaired by OA.
Effect of Osteoarthritis on Biomechanics
OA can have a primary effect on both the motion and the load-bearing functions of the joints of the foot and ankle. With the development of secondary osteophytes about any given articulation, the range of motion of the joint can be significantly compromised. This can cause significant pain from impingement of the osteophytes on surrounding bone and soft tissues (Fig. 21C-2). Pain can also result from a transfer of load from the affected joint to the surrounding joints, leading to pain in the overloaded secondary joints, which can result in a confusing clinical presentation.
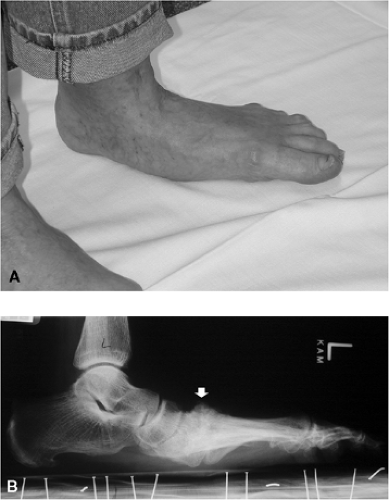
The load-bearing function of a joint can obviously be primarily affected by OA. This will result in pain with weight bearing, frequently accompanied by a functional decrease in range of motion despite an absence of osteophytes. The load-bearing pain can also result in an apparent loss of motor control and instability due to the reflex inhibition of the controlling muscles when loading of the joint causes significant pain. In addition, as OA progresses, significant deformity and malalignment of the joints of the foot and ankle complex may develop (Fig. 21C-3).
TABLE 21C-1 THE RELATIONSHIP OF FOOT AND ANKLE LOADING AND MOTION TO THE PHASES OF GAIT | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differential Diagnosis of Osteoarthritis of the Foot and Ankle
The differential diagnosis of OA of the foot and ankle essentially includes everything else that can possibly occur to these structures. In many instances, the key to determining a diagnosis is based on localizing the source of pain and its temporal pattern. Pain that is not related to weight bearing is unlikely to be OA but is more probably due to neuritis, infection, or inflammatory diseases. Weight-bearing pain that is worse initially and then gets better with further activity is also unlikely to be OA but may be related to tendinitis or inflammatory arthritis. In contrast, typical osteoarthritic pain gradually increases with progressive weight bearing. A complete absence of pain by history and on physical examination of the suspected joints makes OA unlikely, although it can be seen in individuals exhibiting pure complaints of instability. The distinction between a low-grade infection and OA can be difficult clinically. Hematogenous spread of infection to bones of the foot and ankle in the nonpediatric age group is extremely unusual. Consequently, infection in the absence of a local source would not be likely. Pain related to weight bearing in the context of acute trauma should, of course, raise the suspicion of a fracture. One final possible etiology of weight-bearing-associated pain is that of avascular necrosis. This is most common in the talus and presents in three forms: osteochondritis dissecans (involving a small part of the talar dome), post-traumatic (especially after a talar neck fracture), and idiopathic (most commonly associated with steroid use, diabetes, or alcoholism).
Diagnostic Assessment
In most cases, the diagnosis of OA can be made on the basis of the history of symptoms. As noted earlier, pain that is weight bearing in nature and has a monotonically increasing severity with continued weight bearing is classic for OA and serves to differentiate it from tendinitis, neuritis, and inflammatory conditions. The pain should be localized to a joint and should not have radiation of significance either proximally or distally. This can be a bit complicated in long-standing cases of OA in which there may be fairly generalized pain. A change in visible foot shape should also be directly queried because it may be the first clue to conditions such as Lisfranc OA causing midfoot collapse (Fig. 21C-4). Finally, a specific question should be asked about the existence of similar symptoms in the contralateral foot. Although bilateral symptoms can occur in primary OA, they raise the possibility of an underlying inflammatory diathesis.
The physical examination should include observations of the patient standing barefoot, walking barefoot, and sitting. The standing examination allows assessment of symmetry as well as of any weight-bearing deformity or malalignment that would not otherwise be appreciated. The patient should also be asked to do both a heel rise (single- and double-limbed) and forefoot rise to test the strength of the posterior and anterior musculature, respectively. Pain elicited with either of these maneuvers can pinpoint the joint or joints affected by OA. Observing the gait provides insight into limping from either pain (antalgic gait) or weakness. It may also reveal a tendency for the patient to protect one part of the foot by shifting weight elsewhere on the foot. When this occurs, the patient can be specifically asked to bear weight more normally to elicit symptoms.
For the last part of the examination, the patient is sitting with the legs dangling. The passive range of motion of the ankles, subtalar joints, midfoot articulations, and toes should be assessed and recorded. A motor examination of the posterior, tibialis anterior, peroneal, and Achilles tendons is also performed. This is to elicit tenderness in the tendons more than to assess strength. A gross sensory examination should include testing to light touch in the distributions of the deep peroneal (first web space dorsally), superficial peroneal (medial hallux and dorsal lateral midfoot), sural (lateral foot), medial plantar (plantar
medial midfoot and forefoot), and lateral plantar (plantar lateral midfoot and forefoot) nerves. The L5 nerve root is tested by sensation on the medial forefoot and strength of the extensor hallucis longus; the S1 nerve root is tested by sensation on the lateral border of the foot and the Achilles reflex. A systematic palpation examination of each joint of the ankle and foot should then be undertaken to determine the presence of tenderness. The entire physical examination takes between 3 and 4 minutes. The establishment of a personal routine of the complete examination of the foot and ankle will effectively guard against missing significant pathologic processes in this region.
medial midfoot and forefoot), and lateral plantar (plantar lateral midfoot and forefoot) nerves. The L5 nerve root is tested by sensation on the medial forefoot and strength of the extensor hallucis longus; the S1 nerve root is tested by sensation on the lateral border of the foot and the Achilles reflex. A systematic palpation examination of each joint of the ankle and foot should then be undertaken to determine the presence of tenderness. The entire physical examination takes between 3 and 4 minutes. The establishment of a personal routine of the complete examination of the foot and ankle will effectively guard against missing significant pathologic processes in this region.
Imaging of the Foot and Ankle
The most useful imaging modality for foot and ankle problems is the plain radiograph. Because most of the symptoms are related to weight bearing, such films should be obtained with the patient standing. Significant shifts in the articulations can occur with weight bearing, making non-weight-bearing films particularly unhelpful in OA.1 For the foot, the films are obtained in anteroposterior, oblique, and lateral views. For the ankle, anteroposterior, mortise, and lateral views are standard.
Computed tomography (CT) is not a sensitive, specific, or cost-effective way to screen for foot and ankle problems. On the other hand, it is the best method to define bone and joint anatomy in the presence of subtle intra-articular malalignments that can cause OA. The two joints most commonly assessed by CT are the Lisfranc and subtalar joints, both of which are nonlinear, multiplanar, complex articulations. As with CT, screening with MRI is exceedingly unhelpful given the wide variation of normal findings. MRI can be helpful in delineating soft tissue disease, such as posterior tibial tendon ruptures, but it does not add to the clinical assessment of OA. Bone scans typically show abnormalities in osteoarthritic joints, but this does not add any information that cannot be easily obtained by less expensive means, such as by a physical examination.
Principles of Nonoperative Treatment of Osteoarthritis of the Ankle and Foot
Recognition of the Sources of Pain
There are three primary sources of pain on patient presentation. The most common in OA is pain directly related to axial loading of a joint compromised by degenerative changes within the articular surfaces (Fig. 21C-5). In this instance, mere weight bearing frequently elicits the symptoms. The second major source, which may coexist with the first, is pain related to mechanical limitation of motion. This is a consequence of osteophytic change in the periarticular region, which mechanically interferes with a normal range of motion (Fig. 21C-6). These patients primarily have complaints related to ambulation, which requires a functional range of motion that exceeds the limits of the involved articulations. It is important to distinguish these two sources of pain because the surgical treatment of osteophytic change is frequently much less destructive than that of degenerative change. Last, pain may be a consequence of the architectural loss of integrity accompanying OA. This results in clinical instability, such as the midfoot collapse seen in the Lisfranc arthritis, which can be a source of great pain (Fig. 21C-3, Fig. 21C-4).
Biomechanical Rationale of Nonoperative Treatment (With Specific Examples)
The nonoperative treatment of OA of the foot and ankle can be divided into mechanical and biologic regimens. In those patients for whom loading of a compromised arthritic joint is causing pain, the treatment goal is to shunt the forces away from the defective joint to decrease painful loading. For the ankle, this is exemplified by the use of a patella tendon-bearing brace in which the axial loads are supported by the brace and the surrounding soft tissues. Loading across the midfoot joints can be diminished by the use of a stiff-soled rocker-bottom shoe that decreases the bending of the midfoot. External support, such as a cane in the opposite hand or crutches, is also effective in decreasing loading by transferring the load to an upper extremity.
Joints with motion limited by osteoarthritic changes can be made less symptomatic by similar means. A rigid ankle-foot orthosis serves to limit motion in the ankle joint, thereby decreasing painful anterior impingement from osteophytes. Such braces can frequently be obtained off the shelf and used with normal shoes. Hallux rigidus is a prototypical example of how a mechanically limited joint can cause a great deal of pain during normal gait (Fig. 21C-2). The use of a steel shank shoe protects the first metatarsophalangeal joint from dorsiflexion forces, thereby alleviating many of the symptoms of this condition. An interesting example of how shoe wear can provide accommodation to a limited range of motion is the use of a rocker-bottom shoe in patients with anterior ankle osteophytes. The rocker bottom allows the foot to roll off the floor as one progresses from midstance to toe-off without forcing the ankle into a dorsiflexed position. The overall pattern of gait is therefore preserved while the range of motion necessary at the ankle is minimized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree