 Longitudinal Approach to the Proximal Interphalangeal Joint of the Second to Fifth Toes for Hammer Toe
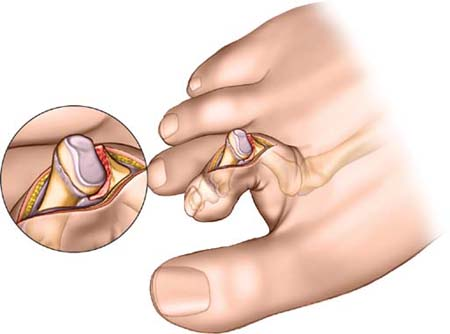
Longitudinal Approach to the Proximal Interphalangeal Joint of the Second to Fifth Toes for Hammer ToeThe longitudinal approach to the proximal interphalangeal joint of the second to fifth toes is used for the treatment of hammer toe deformities. The most common procedure that utilizes this approach is proximal interphalangeal joint fusion.
The longitudinal midline incision gives excellent access to the extensor tendon and the underlying proximal interphalangeal joint.
The advantage of the longitudinal incision is that it allows both proximal and distal extensions if other procedures are to be carried out. The disadvantage of the longitudinal approach is that following correction of the fixed flexion deformity there is often some redundant skin; wound closure thus must be done carefully to avoid creating a space under the skin that could be the site of troublesome postoperative hematoma.
The skin over the dorsal aspect of the interphalangeal joint of a toe with a hammer toe deformity is often red and thinned. In extreme cases, frank ulceration with associated infection may occur. The presence of ulceration is a contraindication to surgery. The skin lesion should be treated before surgery is considered.
As with all procedures of the distal end foot, careful vascular assessment of the patent is indicated, especially in high-risk cases such as diabetes mellitus.
Position of the Patient
Place the patient supine on the operating table. The foot normally lies in a degree of external rotation. If the procedure is to be carried out on the lateral digits, place a sandbag under the buttock of the affected side to correct the external rotation and bring the toes more easily into the plane of the surgical field.
After exsanguination, place a tourniquet on the middle of the thigh. Alternatively, use a soft rubber bandage to exsanguinate the foot, then wrap the leg tightly just above the ankle (see Fig. 1-1). The use of a rubber tourniquet around the toe does restrict access to a minor degree, but has the advantage that it can be used in conjunction with a ring block local anesthesia.
Landmarks and Incision
Palpate the dorsal aspect of the proximal interphalangeal joint of the digit. Passively flexing and extending the joint while palpating its dorsal surface can confirm the exact position of the joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


