Linked Arthroplasty
Bernard F. Morrey
INTRODUCTION
There has been increased interest in the design and use of elbow replacement in the last several years with a number of new devices appearing on the market. This chapter focuses on what is known and documented. It thus serves to complement the description of other implants, especially the newer designs, by distinguishing what is established from what is hypothesized. Today, rather than characterizing devices as resurfacing or hinge, constrained or unconstrained, the most appropriate terminology is that of a linked (coupled) or unlinked (uncoupled) device. The reason for this is that some devices can be very highly constrained because of the configuration of the articular surface, yet they are not mechanically linked. Other devices can be mechanically linked but provide significant play, laxity, or less constraint of the linked articulation. Further, the amount of bone removed for unlinked implants may be considerable and thus not accurately described as resurfacing or conservative.
The potential advantages of an unlinked implant are stated in chapter 22. In general, the perceived value includes an opportunity for a greater amount of polyethylene at the articulation, allows for the option or requirement to replace the radial head, and is more anatomic in concept and thus might theoretically provide a more functional joint. The unproven value of the radial head is a potential disadvantage in some cases. The implications of increased technical difficulty and potential complications associated with the greater demands placed on the accuracy of insertion are other concerns regarding the new devices. At this time, the absence of outcome data requires the use of these implants to be based on theoretic advantages. Finally, prior designs for which data do exist have all suffered from an instability rate of around 5%, a concern that must be addressed by technique or design of the uncoupled device.
ADVANTAGES
The advantage of a linked device is that the joint is rendered immediately stable. This means a broad spectrum of pathology may be addressed. It also implies the potential for a relatively simple procedure of insertion. Hence, in our view there are a significant number of advantages to such a design. These features imply that a rather broad spectrum of conditions can be treated by a relatively large and expanding number of surgeons.
DISADVANTAGES
Depending on the design, the amount of polyethylene at the articulation may be limited with the linked implant, giving rise to the potential for wear and osteolysis. Some linked implants may require more bone to be removed than the unlinked designs, causing difficulty at revision. If the condyles are sacrificed, resection arthroplasty, as a salvage procedure, is unpredictable. Because the forces across the joint are transmitted to the implant/bone interface, linked or unlinked designs that are more constrained have the potential for increased humeral component loosening.
INDICATIONS
The indications for the linked implant are identical to those of unlinked devices and are consistent with the indications for other joint replacements. Specifically, elbow dysfunction that is considered a major limiting factor in the patient’s day-to-day existence justifies consideration of linked implant replacement. This dysfunction typically is the result of pain, but at the elbow the dysfunction can also be attributed to instability or even stiffness. The Mayo experience with the use of a single design since 1982 in more than 1,000 patients reveals the most common indication for total elbow arthroplasty is rheumatoid arthritis (Table 21-1). As noted, the patient with rheumatoid arthritis represents less than 40% of the 1,021 procedures that have been performed at the Mayo Clinic. This is in contrast to most reports regarding elbow replacement in which the patient with rheumatoid arthritis accounts for 80% or more of these procedures. The reason for this is that the linked implants do not require osseous or ligamentous integrity, whereas the unlinked devices do require these anatomic features to be present for implant stability. The indications for a linked implant are thus rather broad and include those with ligamentous deficiency and those with traumatic conditions, which include acute fractures, established posttraumatic arthrosis, distal humeral nonunion, posttraumatic ankylosis, and posttraumatic instability. This spectrum of potential candidates reduces the relative frequency of replacement for rheumatoid arthritis. Finally, revision of a failed total elbow arthroplasty is most reliably managed by a linked device because bone and ligaments are almost always compromised in this setting. The optimum design goal is that of a reliable “off the shelf” implant capable of addressing all these pathologic presentations.
The contraindications for a linked arthroplasty are those for any total elbow—that is, the presence of infection or the lack of adequate motors to gain the anticipated efficacy of the implantation. There are no unique contraindications to the linked implant compared to the unlinked one.
OVERALL OUTCOME
The literature reflects experience with limited semiconstrained/linked devices to be increasing in the last few years. One in-depth experience is that of the GSBIII design (Fig. 21-1). Gschwend and colleagues (1) report 59 procedures, of which 51 were for rheumatoid arthritis. Of the 36 elbows available for long-term assessment at a mean of 13.5 years, 88% of these implants were still in situ. The
authors report a 9% incidence of infection and a similar 9% incidence of loosening of one or more components.
authors report a 9% incidence of infection and a similar 9% incidence of loosening of one or more components.
TABLE 21-1 DIAGNOSIS AMONG 1,021 COONRAD-MORREY ELBOW REPLACEMENT PROCEDURES PERFORMED AT THE MAYO CLINIC FROM 1982 TO 2002 | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
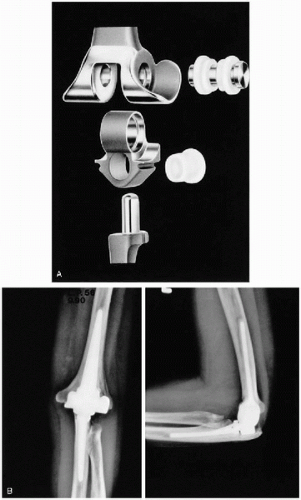 Figure 21-1 A: The GSB III linked, semi-constrained implant. B: It requires intact condyles for humeral fixation. |
 Figure 21-2 Typical outcome of rheumatoid total elbow arthroplasty at 12 years using Coonrad-Morrey implant preoperatively and postoperatively. |
A French experience with 20 GSBIII implants for rheumatoid arthritis (2) reports subjective satisfaction in 19 of 20 elbows (95%) a mean of 3 years after surgery. This experience is in contrast to that of Schneeberger and colleagues, which documented that 9 of 14 patients with a mean 5.8 years after surgery had rheumatoid arthritis, but only 7 of 14 procedures were considered satisfactory (3). Loosening was the major problem occurring in 29% of these patients.
THE COONRAD/MORREY IMPLANT: MAYO EXPERIENCE
In general, and especially in Mayo’s experience, the results of the linked implant have been satisfactory not just for the patient with rheumatoid arthritis but also for the posttraumatic conditions and even in revision settings (4, 5, 6, 7, 8, 9, 10, 11, 12). The overall success is approximately 90% at 5 years.
Rheumatoid Arthritis
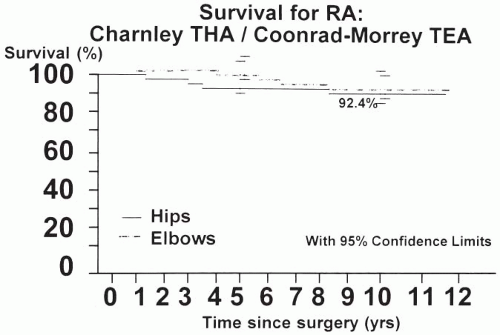
Mayo’s experience with 78 procedures assessed after 10 to 15 (mean 12.5) years for the patient with rheumatoid arthritis reveals a 92.4% rate of survival free of revision (Figs. 21-2 and 21-3). The Mayo Elbow Performance Score (MEPS) in this sample was satisfactory in 86% at 12.5 years. All patients were stable, and 97% had no or minimal pain. The mean flexion arc was 28 to 131 degrees; forearm rotation averaged 68 degrees pronation and 62 degrees supination. (6)
Conner and colleagues also studied the effectiveness of this implant in 18 elbows afflicted with juvenile rheumatoid arthritis. Of patients, 96% were pain-free and satisfied with the procedure an average of 7.4 years after surgery. However, motion was less in this patient population (5).
Acute Fracture
The outcome for acute fracture managed by elbow replacement was originally described in 22 procedures (13). This experience has been updated in a review of 42 patients followed for a mean of 6.5 years. (14) The most recent report reveals an overall objective satisfactory result of 88% using the MEPS. Subjectively, 92% reported a satisfactory outcome. Today the mean time in the hospital is 3.5 days. The complication rate in these patients was 6%, and one (3%) required reoperation for fractured ulnar component subsequent to a fall.
Traumatic Arthritis
The subjective satisfactory results of 41 patients with established arthrosis treated at the Mayo Clinic by total elbow arthroplasty is reported to be 91% (12) The mean age of this group was 74 years, and the mean arc of flexion after surgery was 27 to 131 degrees. A complication rate of 27% was recorded, and 22% required a subsequent procedure, most commonly for ulnar component fracture resulting from excessive usage.
Nonunion
The experience with 39% distal humeral nonunions followed a mean of 4.5 years has been reviewed (10). The surgical technique for these patients includes complete excision of the nonunited fracture fragment, and often the triceps is left attached to the ulna because there is no distal humerus. The objective MEPS was the best of any diagnostic category, averaging 88% objective and 92% subjective satisfaction with a follow-up averaging 4.5 years (Fig. 21-4).
Gross Instability
The outcome of the treatment of 19 patients with gross instability by the use of the Coonrad-Morrey implant has been reported by Ramsey and colleagues (11). At 6 years all were stable, and 16 of 19 were without pain. Final arc of motion averaged 25 to 128 degrees. The MEPS was 44 before and 86 after surgery. One implant became loose.
Ankylosis
Posttraumatic stiffness is a particularly difficult problem usually following severe trauma and has been assessed by Mansat and associates (8). Of 13 patients with less than 30 degrees motion before surgery, 9 were fused. At 6 years, 8 of 13 patients (62%) recorded an objective satisfactory result, whereas 10 of 13 (82%) reported subjective satisfaction. The main factor accounting for this low performance score is the lack of attainment of the functional 100 degrees of flexion arc. The mean arc improved in this group from 7 to 67 degrees.
 Figure 21-4 A: Distal humeral nonunion. B: Typical 5-year outcome with Coonrad-Morrey linked prosthesis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|