Latarjet Procedure for Instability with Bone Loss
Patrick J. Denard
Stephen S. Burkhart
DEFINITION
Recognizing and properly addressing bone defects is crucial to achieving good surgical outcomes in shoulder instability.
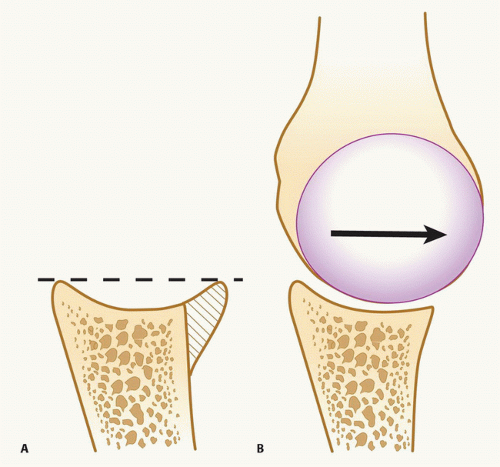
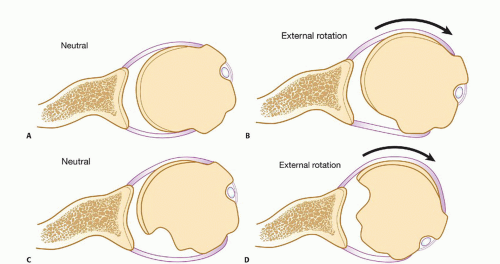
One of the most important requirements for glenohumeral stability is a long congruent articular arc in which the humerus and glenoid remain in contact throughout motion. Loss of this congruent arc can occur from glenoid bone loss or defects in the posterior humeral head (ie, Hill-Sachs lesions) (FIGS 1 and 2).
We define glenoid bone loss requiring Latarjet as glenoid bone loss 25% or greater of the inferior glenoid diameter.
In the Latarjet procedure, the coracoid is transferred to the inferior glenoid and secured with two screws.
As noted by Patte, the success of the Latarjet procedure can be attributed to the triple effect, which is composed of the following:
Lengthening of the articular arc by the bone graft
The sling effect of the conjoined tendon
Tensioning of the lower subscapularis by means of the conjoined tendon in its new position (draped over the lower subscapularis)
ANATOMY
In 1954, Latarjet14 described his technique for a coracoid bone graft to prevent anterior dislocation.
He detached the pectoralis minor from the coracoid, incised the coracoacromial ligament, left a stump of the coracoacromial ligament attached to the coracoid, then completed the osteotomy at the base of the coracoid so that it could be placed as a bone graft against the anterior glenoid neck.
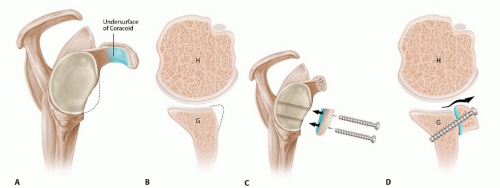
The coracoid was passed through a split in the subscapularis and positioned so that its inferior surface was in contact with the anterior glenoid neck where it was secured with two screws (FIG 3). In doing so, the posterolateral surface of the coracoid was placed adjacent to the glenoid joint surface.
We call our surgical technique the congruent arc technique. This technique was first reported by Burkhart and DeBeer5 in 2000 and incorporated two important modifications:
The coracoid graft was rotated 90 degrees around its long axis so that the concave inferior surface of the coracoid became the extension to the glenoid concavity, providing
a much more anatomic articular arc to the reconstructed glenoid surface11 (FIG 4).
The capsule was reattached to the native glenoid by means of suture anchors so that the coracoid graft was extra-articular, thereby preventing abrasion of the humeral articular surface against the coracoid graft.
Use of the congruent arc technique, or the inferior aspect of the coracoid extending the glenoid, more closely restores normal glenohumeral contact forces compared to the posterolateral position described by Latarjet.11
PATHOGENESIS
Bone lesions are present in up to 95% of patients with recurrent shoulder instability.10
Examining the glenoid alone, Sugaya et al19 reported that 90% of patients with recurrent instability have glenoid bone
abnormalities (including bone loss or abnormal contour). Glenoid bone loss (distinct from abnormal contour alone) was seen in 50% of cases in over half of which the defect was greater than 5% of the glenoid width.
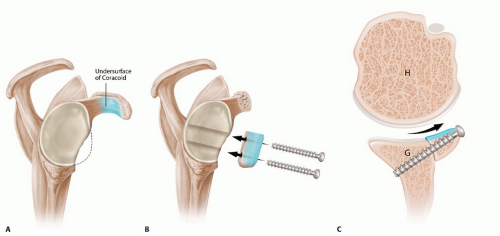
FIG 4 • Schematic of the Burkhart-DeBeer modification of the Latarjet reconstruction. A. Sagittal view demonstrates glenoid bone loss. The undersurface of the coracoid is shaded in blue. B. Following coracoid osteotomy, the graft is rotated 90 degrees so the undersurface of the coracoid is flush with the glenoid and forms a continuation of the concave glenoid articular arc. The graft is secured with two screws. C. Axial view demonstrates how the orientation change (compared to the original French technique [FIG 3]) provides a contour that more closely matches the native glenoid concavity and also provides greater length extension of the articular arc. G, glenoid; H, humerus. (Reproduced with permission from Burkhart SS, Lo IK, Brady PC, et al. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott Williams & Wilkins, 2012.)
Yamamoto et al20 introduced the concept of the “glenoid track” to describe the interaction between glenoid bone loss and Hill-Sachs lesions.
When the arm is raised, the glenoid contact area shifts from the inferomedial to the superolateral portion of the posterior articular surface of the humeral head, creating a zone of contact (glenoid track) between the glenoid and the humeral head. An intact glenoid track results in bony stability.
In cases with 25% or greater glenoid bone loss, bony stability is always compromised and bony augmentation is required.
In cases with less than 25% glenoid bone loss, the “glenoid track” can be used to define the Hill-Sachs lesion as “on track” or “off track” and therefore determine the need for remplissage in addition to arthroscopic Bankart repair.
NATURAL HISTORY
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history is essential and should elicit the mechanism of injury and prior treatments received.
Previous operative reports should be obtained and reviewed; they often yield valuable information about areas of bone deficiency, tissue quality, and fixation devices used.
Essential components of the history include age, mechanism of dislocations, number of dislocations, position of shoulder during dislocation, reduction efforts (self- or physician reduced), hand dominance, sport and work requirements, prior treatments, and patient’s goals.
The physical examination determines the position and direction of instability as well as identifies or eliminates factors that contribute to instability:
Muscle tone or wasting
Range of motion, active and passive
Strength assessment (rule out concomitant rotator cuf tear)
Position of apprehension
Relocation relief
Direction of instability (load and shift test)
Generalized ligamentous laxity
Neurovascular examination
IMAGING AND OTHER DIAGNOSTIC STUDIES
Our evaluation for bone loss is based on preoperative and intraoperative assessments. We routinely obtain anteroposterior (AP), transscapular lateral, and axillary radiographs of the glenohumeral joint. Radiographs are evaluated on all patients for the presence of glenoid bone loss or a Hill-Sachs lesion.
Although plain radiographs can grossly demonstrate bone defects, the severity is often underestimated. We therefore obtain a computed tomography (CT) scan with three-dimensional (3-D) reconstructions on all individuals with suspected bone loss. Additionally, we have a low threshold
for obtaining a CT in patients without plain radiographic evidence of bone loss but otherwise have risk factors for recurrence (eg, young patients, multiple dislocations). To estimate glenoid bone loss, bilateral 3-D CTs are obtained.
Assuming a normal contralateral shoulder, the percentage of bone loss is easily estimated by comparing the width of the glenoid on the affected side to the width of the glenoid on the normal shoulder in the en face view. In 96% of cases, this technique accurately stratifies glenoid bone loss as less than or greater than 25% of glenoid width.9
DIFFERENTIAL DIAGNOSIS
Multidirectional instability
Seizure disorders
NONOPERATIVE MANAGEMENT
There are few indications for nonoperative management of glenoid bone loss 25% or greater.
However, uncontrolled seizure disorders must be recognized and may be contraindication to Latarjet reconstruction based on the high failure rate with this condition.18
In addition, infection and voluntary instability are contraindications to Latarjet reconstruction.
SURGICAL MANAGEMENT
Our main indications for performing an open Latarjet procedure are the following:
Glenoid bone loss of 25% or greater of the inferior glenoid diameter (inverted pear glenoid)
Deep Hill-Sachs lesion that engages in a position of 90-degree abduction plus 90-degree external rotation (position of athletic function)
In general, we have found that a large engaging Hill-Sachs lesion usually occurs in combination with an inverted pear glenoid, so such a case satisfies both indications. Also, when there is a large Hill-Sachs lesion, the coracoid bone graft in the Latarjet procedure will lengthen the articular arc to such an extent that the Hill-Sachs lesion will not be able to engage the glenoid rim. In this way, the Latarjet procedure effectively addresses the Hill-Sachs lesion without the need for an additional bone graft to the humeral defect.
One relative indication for the Latarjet reconstruction is in the patient with severe soft tissue loss involving the anterior labroligamentous complex.
Such soft tissue deficiency can occur due to thermal capsular necrosis or due to multiple failed soft tissue procedures for instability. Although some authors have recommended soft tissue allografts, we have preferentially done the Latarjet reconstruction without soft tissue augmentation.
Alternatively, we have noted that there are occasional cases with partial loss of the capsule (thermal capsular necrosis; multiple failed surgeries) without any significant bone loss. We have found that such cases may be amenable to arthroscopic repair using a flap of the deep surface of the subscapularis to augment or to substitute for the anterior capsule.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree