Intussusception
Mary L. Brandt
Intussusception is the most common cause of intestinal obstruction in infants aged 3 months to 3 years. Intussusception rarely occurs in the first month of life and has a peak occurrence in infants between the ages of 5 and 9 months. The incidence of intussusception has considerable regional variation, from less than 0.5 to 4 per 1,000 live births. The highest incidences worldwide are found in northern New York, southern Quebec, and China.
PATHOPHYSIOLOGY
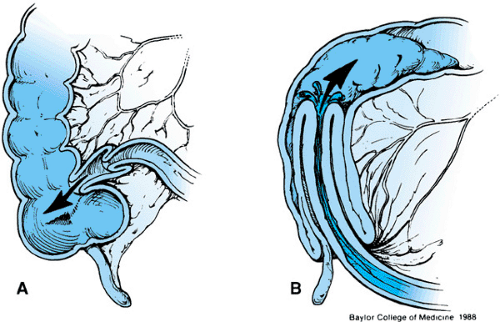
Intussusception is the result of invagination or telescoping of a portion of the bowel into the more distal bowel (Fig. 348.1). The portion of the bowel that invaginates into the more distal bowel, the intussusceptum, is pulled along with its mesentery by peristaltic waves. As the proximal bowel is pulled into the lumen of the intussuscipiens, or distal bowel, the mesentery is compressed and angled, resulting initially in lymphatic obstruction and subsequently in venous obstruction. The intussuscepted mass quickly obstructs the intestinal lumen, resulting in distention and peristaltic rushes proximal to the obstructing mass. With each peristaltic rush, the patient experiences colicky pain. As the edema from lymphatic obstruction and venous engorgement increases, the hydrostatic pressure within the intussusception increases until it equals the arterial pressure, at which time arterial inflow ceases. The intestinal mucosa becomes ischemic, with an outpouring of mucus into the intestinal lumen. Venous engorgement results in leakage of blood into the intestinal lumen, and the blood and mucus form the classic “currant jelly” stools. Although currant jelly stools are relatively diagnostic, they occur in only a small percentage of patients and are a fairly late sign of intussusception.
ETIOLOGY
Most infants who develop intussusception are healthy and well nourished. Approximately 10% of patients have a previous history of diarrhea, and many have signs and symptoms of respiratory tract infections. Approximately 65% of intussusceptions occur before the patient’s first birthday, and in almost all of these patients, no clear cause of the intussusception can be identified. Enlarged lymphoid tissue in the wall of the terminal ileum (Peyer patches) is a common finding in children with intussusception and probably acts as the lead point for the intussusception. An inexperienced surgeon may confuse this tissue with tumor and request a biopsy or resect the bowel unnecessarily. The association of intussusception with viral syndromes and the presence of this enlarged lymphoid tissue support a viral cause for the majority of the “idiopathic” intussusceptions. Adenovirus and rotavirus, in particular, have been implicated in the pathophysiology of intussusception.
Approximately 2% to 3% of older children with intussusception have a lesion such as polyps, Meckel diverticulum, ectopic pancreas, small enterogenous cysts, lymphomas, and benign tumors of the ileal wall that serves as a lead point. Localized edema or hemorrhage of the bowel wall such as that seen in patients with Henoch-Schönlein purpura, abdominal trauma, hemophilia, and leukemia also may act as a lead point. Altered intestinal motility or uncoordinated peristalsis (such as that seen after head injuries, use of anticholinergic medication, or enteritis associated with acquired immunodeficiency syndrome) also has been associated with the development of intussusception. Postoperative intussusception occurs most often after retroperitoneal dissections, particularly for tumors, and after fundoplication, presumably as a result of vagal manipulation. Nearly all intussusceptions associated with altered motility are located in the small bowel. Patients with cystic fibrosis may develop intussusception as a result of mucus-laden hypertrophied mucosal glands, which act as lead points, and as a result of the thick, tenacious fecal material associated with enzymatic insufficiency (Box 348.1). The average age for patients with cystic fibrosis who develop an intussusception is 9 years. Chronic indwelling tubes may be associated with intussusception; edema of the bowel wall caused by the tube serves as the intussuscepting point.
CLINICAL PRESENTATION
Nearly all affected infants present with vomiting and colicky pain. Because these two symptoms are nonspecific and common, infants typically are seen later in the course of illness, at which time they are more likely to have bloody stools and high fever. The classic triad of colicky abdominal pain, vomiting, and bloody stools occurs in as few as 10% of children
diagnosed with an intussusception. Early in the course of illness, because of the acute distention of the small bowel, the affected infant evacuates the distal colon and passes several partially formed stools. In fact, this finding is so universal that the presence of a large amount of stool in the rectum by examination or radiography renders the presence of an intussusception mass less likely. The same reflex is responsible for the vomiting. Initially, the vomitus is clear, but as the intestinal obstruction progresses, the vomitus becomes bile-stained and eventually fecaloid. The peristaltic rushes and colicky pain first occur at intervals of several minutes and last only a few seconds. During the intervals between peristaltic rushes, the infant appears to be in no discomfort, and the abdomen is soft and scaphoid. Children with intussusception may develop a profound lethargy, mimicking a true coma. In fact, in some children this condition may be the presenting symptom.
diagnosed with an intussusception. Early in the course of illness, because of the acute distention of the small bowel, the affected infant evacuates the distal colon and passes several partially formed stools. In fact, this finding is so universal that the presence of a large amount of stool in the rectum by examination or radiography renders the presence of an intussusception mass less likely. The same reflex is responsible for the vomiting. Initially, the vomitus is clear, but as the intestinal obstruction progresses, the vomitus becomes bile-stained and eventually fecaloid. The peristaltic rushes and colicky pain first occur at intervals of several minutes and last only a few seconds. During the intervals between peristaltic rushes, the infant appears to be in no discomfort, and the abdomen is soft and scaphoid. Children with intussusception may develop a profound lethargy, mimicking a true coma. In fact, in some children this condition may be the presenting symptom.
BOX 348.1 Examples of Lesions that Can Serve as Lead Point for Intussusception
Enlarged Peyer patches
Meckel diverticulum
Polyps
Ectopic pancreas
Enterogenous cysts
Lymphomas
Localized edema of bowel wall (may be seen in Henoch-Schönlein purpura, trauma, hemophilia, and leukemia)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree