Intramedullary Fixation of Proximal Humerus Fractures
Mark Morrey
Pascal Boileau
J. Dean Cole
Thomas d’Ollonne
DEFINITION
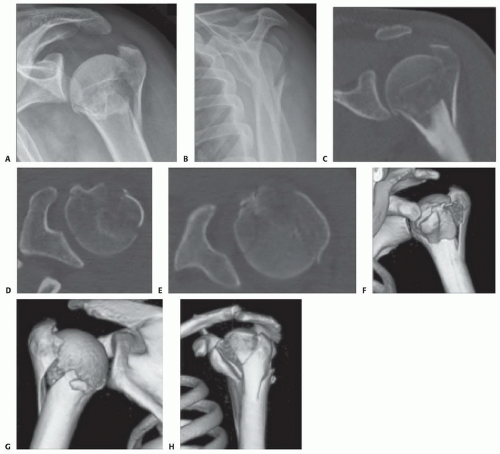
Fractures of the proximal humerus can be two, three, or four part according to the Neer classification (FIG 1).
Fifty percent to 80% of proximal humerus fractures are nondisplaced or minimally displaced and stable.A short period of immobilization in neutral rotation to avoid fracture malunion followed by early mobilization is usually sufficient to treat fractures and can result in satisfactory outcomes.
Twenty percent to 50% of patients with displaced, unstable two-, three-, four-part proximal humerus fractures with a vascularized, attached head fragment may benefit from operative management with reduction and internal fixation.
Extensive dissection and inadequate biomechanical fixation in the context of the severe soft tissue injury, osteopenia, and devascularization associated with these complex fracture types are the commonly cited reasons for failure of internal fixation devices.
Encouraging reports have been made on the use of intramedullary nails for two-,three-, and even select four-part fractures. Newer designs of intramedullary nails that permit stable fixation of the head to the shaft of the humerus while maximizing biomechanical fixation of the tuberosities using a minimally invasive rotator cuff-splitting approach are ideal.
Techniques in this chapter use the Aequalis intramedullary nail (Tornier, Inc., Bloomington, MN). This is an intramedullary stabilization device for proximal humeral fractures, designed specifically to optimize tuberosity fragment fixation and provide stable support for the humeral head, improving proximal humeral reconstruction and fixation in osteopenic bone.
ANATOMY
Osteology
The proximal humerus includes the humeral head, the lesser tuberosity (LT), the greater tuberosity (GT), and the proximal humeral metaphysis.
The position of the head is higher than the tuberosities, and changes in this relationship will cause poor biomechanical function. The humeral head is slightly medial (3 mm) and posterior (7 mm) in relation to the humeral shaft (FIG 2).
The humeral head is retroverted approximately 30 degrees (range 20 to 60 degrees).
The bicipital groove separates the lesser and greater tuberosities. The hardest bone in the proximal humerus is located within the bicipital groove and most fractures of the GT occur posterior to the groove.
Vascular Supply of the Proximal Humerus
The anterior and posterior humeral circumflex arteries are branches of the axillary artery.
The arcuate artery, the terminal vessel of the ascending branch of the anterior humeral circumflex artery, supplies most of the humeral head.
Avascularity of the humeral head can occur if this vessel is disrupted during a fracture of the anatomic neck.
The posterior circumflex artery becomes important in patients with proximal humerus fractures.
It may be the primary source of blood supply to the fractured head, so care should be taken to prevent additional devascularization.
Traumatic and iatrogenic vascular insult may lead to devascularization of the fracture fragments, resulting in delayed union, nonunion, and avascular necrosis. Traumatic injury cannot be prevented; well-planned minimally invasive procedures should reduce the risk of further damage, however.
Innervation
The brachial plexus is at risk in patients with upper extremity injury, and thorough neurologic evaluation is mandatory.
The axillary nerve courses through the quadrilateral space, where it is at risk during fracture dislocation.
The lateral entry site for locking screw fixation (4 to 5 cm distal to the tip of the acromion) places the axillary nerve at risk.
PATHOGENESIS
A blow to the anterior, lateral, or posterolateral aspect of the humerus typically is the cause.
Axial load transmitted to the humerus may cause impacted fracture in osteoporotic bone.
Violent muscle contractures, as in grand mal seizures and electric shock, are associated with posterior dislocation- and impaction-type fractures due to overpowering internal rotators and adductors.
Pathologic causes include tumor, multiple myeloma, and metastatic or metabolic disorders.
Osteoporosis is associated with fractures of the proximal humerus (more than any other fracture).
Minor losses in the humeral length between the head and the deltoid insertion can alter the deltoid length-tension ratio.
In unstable three- and four-part fractures, displacement occurs because of the pull of the rotator cuff muscles on their attached tuberosities in the transverse plane, widening the gap created by the fracture plane posterior to the bicipital groove. The GT is pulled posteromedially by the
infraspinatus and teres minor muscles, whereas the LT is pulled anteromedially by the subscapularis muscle (FIG 3).
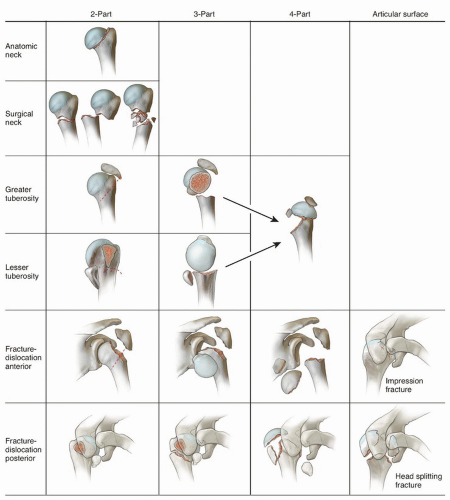
FIG 1 • Classification of shoulder fractures according to Neer. Fracture patterns that are shaded in blue are amenable to humeral nailing.
In four-part proximal humerus fractures, it has been demonstrated that the main vertical fracture plane separating the tuberosities is located posterior to the bicipital groove and that the principal displacement of such fractures occurs in the transverse (horizontal) plane (FIG 4).
In fractures involving the loss of reduction and fixation of the GT leads to definitive retraction and atrophy of the two single external rotator muscles of the shoulder (infraspinatus and teres minor).
Results in definitive pseudoparalyzed and stiff shoulder for which surgical options are limited.
By contrast, posttraumatic humeral head necrosis is well tolerated if the GT has healed in an anatomic position and there is no screw penetration or glenoid erosion. Thus, all efforts of the surgeon should not be directed toward the humeral head but to the GT fixation and reduction.
The humeral head becomes stable when both tuberosities are reduced and fixed.
Modern intramedullary nails have been designed specifically to optimize tuberosity fragment fixation and provide stable support for the humeral head, improving proximal humerus reconstruction and fixation in osteopenic bone. The design of these nails and these specific techniques have been created to avoid the common complications
and problems related to previous intramedullary nailing of proximal humeral fractures.
NATURAL HISTORY
Epidemiology
Four percent to 5% of all fractures
Increased incidence in osteoporosis, older middle-aged and elderly persons (third most common fracture in elderly)
In persons older than 50 years of age, the female-to-male ratio is 4:1 (osteoporosis). Minor falls and trauma may cause comminuted fracture.
In patients younger than 50 years of age, violent trauma, contact sports, and falls from heights are responsible for fractures.
Surgical neck fracture is common.
Consequences of Injury
Nondisplaced fractures may heal without major consequences.
Acute, recurrent, or chronic dislocation
Rotator cuff tears
Neurovascular injury: axillary nerve, brachial plexus
Avascular necrosis of the humeral head can result from disruption of the arcuate artery. The axillary artery also may be damaged but less commonly.
Malunion
Malunion of the tuberosities causes poor shoulder function due to altered biomechanics.
Shortening may cause poor shoulder function due to changes in the length tension relationship of the deltoid.
Posttraumatic arthrosis
Adhesive capsulitis
Biceps tendinopathy
Chronic pain
PATIENT HISTORY AND PHYSICAL FINDINGS
Associated injuries
Rotator cuff tears
Dislocation
Forearm fractures
Brachial plexus, axillary, and radial and ulnar nerve injuries (5% to 30% of complex proximal humerus fractures)
Biceps tendon injury/entrapment
IMAGING AND OTHER DIAGNOSTIC STUDIES
Trauma series
Scapular anteroposterior (glenoid view)
Trans-scapular
Axillary
Rotational views
Computed tomography (CT) scan is very helpful to characterize the fracture fragments and aid in surgical planning.
SURGICAL MANAGEMENT
Indications
Displaced or unstable two-, three- and certain four-part proximal humerus fractures.
Prerequisites
Shoulder table, image intensification, and experienced radiology technician
Be aware of the learning curve (do not attempt nailing of a four-part fracture before acquiring adequate experience with two- and three-part fractures).
When treating patients with complex fractures, obtain the patient’s consent for a hemiarthroplasty and/or reverse shoulder arthroplasty if these treatments are determined to be the best treatment and have the implant available in case it is found to be necessary.
Contraindication: head-splitting, comminuted displaced humeral head fragment devoid of soft tissue attachments
Preoperative Planning
Successful intramedullary nailing of the proximal humerus fracture depends on consistent integration between image intensification and the surgical steps.
Patient positioning on a radiolucent table will allow the surgeon to use a minimally invasive approach.
Errors in the nail entry site will cause inevitable problems with the rest of the procedure.
It is crucial that the surgeon follow the surgical technique precisely.
Positioning
Positioning on the table must allow orthogonal and overhead axillary views.
The patient is placed supine in the beach-chair position with the elbow flexed 90 degrees on a radiolucent table tilted at 60 to 70 degrees. The C-arm should be positioned to allow the surgeon easy access to the proximal humerus (FIG 5).
A bolster may be used to elevate the shoulder from the table and to allow shoulder extension. Extension of the shoulder aids in exposure to the entry site in the humeral head.
Approach
Each type of proximal humerus fracture (two-, three-, four-part) has its own pathophysiology and complications. The surgical technique must therefore vary accordingly. Three-dimensional CT scan images reveal the exact fracture geometry and allow accurate preoperative planning.
Three surgical approaches are possible depending on the fracture type and the surgeon’s preference:
The percutaneous approach, in which the deltoid muscle and supraspinatus are bluntly split through a superior, 1-cm incision, is used most frequently for two-part fractures not requiring tuberosity fixation.
The superior transdeltoid approach, in which the anterior head of the deltoid is detached from the anterior acromion with the tip of the acromion to expose the rotator cuff, is used most often if the GT is involved.
The deltopectoral approach, in which the anterior deltoid muscle is retracted to expose the rotator cuff, can be used in three-part fractures involving the LT.
This chapter will describe the superior transdeltoid approach to fix a valgus impacted four-part fracture and the percutaneous approach for a two-part fracture. The technique is easily adapted for three-part fractures involving only one of the tuberosities.
For all approaches, the straight nail must be inserted medially either through the supraspinatus muscle fibers or through the rotator interval. The entry portal of the nail is created with an awl and enlarged with a reamer under fluoroscopic control. If the bicipital groove is fractured, the long head of the biceps should be tenodesed to avoid postoperative pain and stiffness.
TECHNIQUES
▪ Four-Part Valgus-Impacted Fracture with a Superior Transdeltoid Approach
A saber incision in line with Langer lines is planned and created to expose the division of the anterior and middle deltoid (TECH FIG 1A). This division is found just lateral to the anterior edge of the acromion.
A split is made between the anterior and middle deltoid fibers with a cautery with the arm in slight abduction to help relax the deltoid. The saw is used to create an osteotomy of the anterior acromion, which will allow exposure for nail entry and facilitate later repair. The osteotomy is completed with an osteotome. The deltoid is split no more than 4 cm from the acromion to avoid injury to the axillary nerve. The saber incision helps to avoid splitting the deltoid distally to prevent this from happening. Gelpi self-retaining retractors help to facilitate the exposure (TECH FIG 1B).
A Hohmann retractor is placed over the coracoid to help gain exposure for bursal resection. The bursa is excised to expose the GT, LT, and head fracture fragments. Great care is taken to stay below the deltoid fascia to avoid injury to any branches of the axillary nerve (TECH FIG 1C).
The fracture is identified and then the fibers of the rotator cuff can be incised longitudinally to expose the head fragment if needed (TECH FIG 1D).
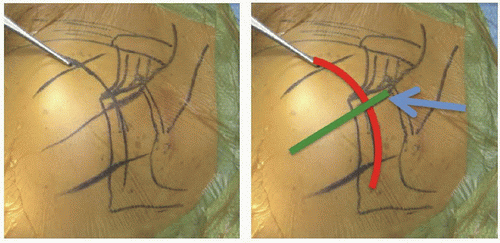
TECH FIG 1A • Landmarks and skin incision for a superior transdeltoid approach have been drawn out. A saber incision in line with Langer lines is made (red arc). It is centered over the division between the anterior and middle deltoid (green line). The blue arrow is the site of the acromial osteotomy, which facilitates the deltoid repair at the end of the case.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access