Abstract
Innovative technologies for sensorimotor rehabilitation after stroke have dramatically increased these past 20 years. Based on a review of the literature on “Medline” and “Web of Science” between 1990 and 2013, we offer an overview of available tools and their current level of validation. Neuromuscular electric stimulation and/or functional electric stimulation are widely used and highly suspected of being effective in upper or lower limb stroke rehabilitation. Robotic rehabilitation has yielded various results in the literature. It seems to have some effect on functional capacities when used for the upper limb. Its effectiveness in gait training is more controversial. Virtual reality is widely used in the rehabilitation of cognitive and motor impairments, as well as posture, with admitted benefits. Non-invasive brain stimulation (rTMS and TDCS) are promising in this indication but clinical evidence of their effectiveness is still lacking. In the same manner, these past five years, neurofeedback techniques based on brain signal recordings have emerged with a special focus on their therapeutic relevance in rehabilitation. Technological devices applied to rehabilitation are revolutionizing our clinical practices. Most of them are based on advances in neurosciences allowing us to better understand the phenomenon of brain plasticity, which underlies the effectiveness of rehabilitation. The acceptation and “real use” of those devices is still an issue since most of them are not easily available in current practice.
Résumé
Les technologies innovantes appliquées à la rééducation sensori-motrice dans les suites d’un accident vasculaire cérébral se sont multipliées ces 20 dernières années. À partir d’une revue de la littérature sur « Medline » et « Web of Science » entre 1990 et 2013, nous proposons une synthèse des outils disponibles et de leur niveau de validation actuel. La stimulation électrique neuromusculaire et/ou fonctionnelle a une efficacité admise dans cette indication. La robotique de rééducation a été diversement appréciée dans la littérature. Il semble qu’elle ait une certaine efficacité sur les capacités fonctionnelles lorsqu’elle est utilisée pour le membre supérieur. Son efficacité dans la rééducation à la marche est plus controversée. La réalité virtuelle est utilisée par de nombreuses équipes dans la rééducation de la motricité ou de la posture, avec un bénéfice maintenant admis. Les techniques de stimulations cérébrales non invasives (rTMS et TDCS) sont encore exploratoires dans cette indication, de la même façon que les techniques de neuro-feedback visant à utiliser l’enregistrement du signal cérébral pour agir sur la plasticité cérébrale. L’avènement de ces technologies appliquées à la rééducation est en train de révolutionner nos pratiques. Elles reposent sur les progrès des neurosciences qui nous permettent de mieux comprendre les phénomènes de plasticité neurale qui sous-tendent l’efficacité de la rééducation. L’appropriation de ces outils par les patients et les thérapeutes est une nécessité. Ces dispositifs doivent se mettre au service de la relation entre le patient et son rééducateur mais ne peuvent se substituer à ce dernier.
1
English version
1.1
Introduction
The rehabilitation of hemiplegic patients has greatly improved these past 30 years . New organization models have been proposed, from the creation of specialized units , to the concepts of “early supported discharge” , “telerehabilitation” and “self-rehabilitation” .
Alongside these organizational evolutions, the methods and means available for the rehabilitation of these patients have varied in a considerable manner, with a greater importance allocated to technological devices . This evolution was made possible by the advances in neurosciences that enabled the better understanding of brain plasticity mechanisms underlying the phenomena of sensorimotor and cognitive recovery as well as the better integration of learning theories in our rehabilitation programs. These progresses have completely altered the principles driving our rehabilitation practices with the emergence of new ideas such as the notion of task-oriented rehabilitation training, the new focus on the importance of intensity and repetition of exercises, as well as challenging the commonly admitted duration of our rehabilitation programs. This evolution has been widely influenced by the emergence of new technologies that found in this pathology an increasingly larger field of potential applications. Finally, this evolution of concepts and practices was associated to important progresses in rehabilitation-related professions and the healthcare organizations managing these patients.
The objective of this work was to propose a non-exhaustive synthesis of the main technologies involved in the rehabilitation of hemiplegic patients based on a review of the literature conducted on “Medline” and “Web of Science” for the period going from 1990 to 2013.
1.2
Rehabilitation technological devices
1.2.1
Neuromuscular or functional electrical stimulation (FES)
Motor-stimulating currents were proposed more than 30 years ago for the rehabilitation of hemiplegic patients. The simple use of these currents was quickly enriched by more elaborated functions such as devices coupling detection and stimulation to let the patient’s own motor functions express themselves during a voluntary task ( Fig. 1 ), before motor-stimulating currents take over . This technique has showed its effectiveness for the upper limbs, especially in hemiparetic patients . These devices can easily be integrated into “task-oriented” rehabilitation programs; in fact electrical stimulation is dedicated to the patient’s movements rendering them possible and easier to complete (FES). Thus, FES can be used for gait (e.g. Walkaid ® system) or grasping (e.g. Handmaster ® system) tasks. It is interesting to note that these particular devices, initially designed for orthotic purposes, seem to have a therapeutic relevance by improving the motor functions in the stimulated muscles .

1.2.2
Rehabilitation robotics
Rehabilitation robots are interactive motorized devices allowing the mobilization of a limb for sensorimotor rehabilitation but also potentially, for cognitive rehabilitation. Rehabilitation robotics, whether they concern the upper or lower limbs, are generally divided into two categories: automated exoskeleton that move the limbs by controlling the displacement of each segment, and devices that enable the mobilization of a limb from a distal application point ( Fig. 2 ), without the control of the various joints . Depending on their design, these robots work in two or three dimensions. They are designed with different working modes: simple passive mobilization, robot-assisted mobilization that interacts more or less with the subject, and resistance training. Most robots enable the interaction with a virtual environment. The technological sophistication of these different systems is quite uneven, reflecting the yet not completely mature nature of these technologies .

The oldest rehabilitation robots are in fact isokinetic dynamometers; they are dedicated to instrumental muscle strength training and completely fit the definition of rehabilitation robotics. In hemiplegic patients, their relevance in lower limb rehabilitation has been validated whereas their effectiveness in upper limb rehabilitation is still being debated .
The effectiveness of upper limb robot-assisted rehabilitation on stroke patients is strongly suspected. The latest meta-analyses suggest a superiority of robot-assisted rehabilitation when embedded in a complete rehabilitation program, compared to conventional methods on motor recovery of the upper limb, with a transfer of the acquired skills into the patient’s daily life . The mechanisms explaining this effectiveness remain uncertain; it is possible that the intensity and repetition of the exercises might be largely at the origin of the effectiveness for this type of rehabilitation. The individual effects of robotics remain unknown and are still being debated today. The refinement of these devices might probably promote a better effectiveness . Non-automated electromechanical devices, like Armeo ® , are often classified as rehabilitation robots even though their functioning mode does not fit the definition of robots. The effectiveness of robot-assisted rehabilitation for the lower limbs is still being argued in the literature . Some studies reported that the “dose” effect was greater for robot-assisted gait rehabilitation than for robot-assisted upper limb rehabilitation. Paradoxically, these devices offer functions that are often less advanced than devices used for the upper limb: the interaction with the patient is mostly limited to applying forces to impose a “normal” gait pattern to the subject, with parameters set by the therapists. There are very few devices equipped with self-adapting functions where the machine can adapt to the patient’s performances. . The association with virtual reality is rare on these robots .
Generally, very few rehabilitation robots are available on the market, and their diffusion is greatly limited by the yet immature nature of the technology, the price of the devices, as well as the reluctance of therapists and patients to use them . These reluctances are fed by the fear of seeing these rehabilitation robots replace human help; yet most studies have shown that the effectiveness of robot-assisted rehabilitation was based on its integration within a global program where the place of rehabilitation therapists is essential.
1.2.3
Virtual reality
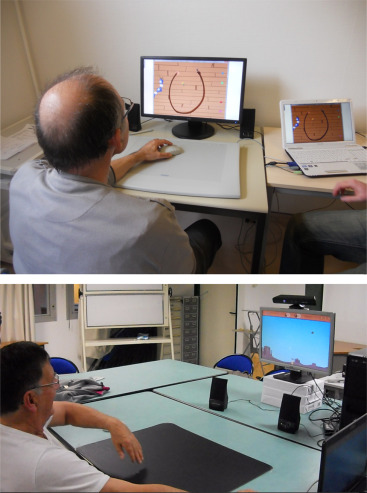
Virtual reality has strongly invaded the field of rehabilitation . Video games for the general public have been tested on neurological patients in several clinical studies, and have shown their effectiveness especially in upper limb rehabilitation but also for posture rehabilitation. Encouraged by these first publications, several teams have started working on video games dedicated to the rehabilitation of hemiplegic patients and thus designed with the help of therapists based on their knowledge of motor and cognitive specificities required for these patients ( Fig. 3 ). The superiority of “dedicated” games has not yet been validated, but in this case also it is probably due to the immaturity of these technologies. These games are progressively enriched with promising new functions, not yet fully validated: intelligent components allowing the automatic adaptation of the game to the patient’s own achievements , command interface enabling the therapist to adapt online the game’s characteristics to the patient’s needs, multiplayer systems to play outside of the institution via a web-service platform.
Besides its rehabilitation relevance, virtual reality opens essential perspectives in terms of patient follow-up and individualization of care. In fact, thanks to the automatic recording of the movements performed by the subject, we will be able to conduct a refined analysis of the quality and quantity of motor function progression, and also to better understand this progression timeline. The collected data should help us decipher the learning and recovery mechanisms, in order to better analyze how we could act on them. Furthermore, this data acquisition will facilitate the modeling of post-stroke recovery and improve our ability to individualize in a very precise manner these rehabilitation programs .
1.2.4
Modulation of sensory afferents
We find under this term techniques using sensory afferents to impact on the recovery of functional motor abilities. All sensory feedback techniques, visual or auditory and biofeedback techniques can fit into this category; voluntarily we will only review them briefly . These techniques are old and technological advances have enabled the sophistication of their application as well as providing a better understanding of their action mode. These sensory afferent modulation techniques also concern transcutaneous stimulation devices, like TENS, sometimes proposed as adjuvant methods to other sensorimotor rehabilitation devices .
The three most advanced techniques for sensory afferent modulation are mirror therapy, robot-assisted rehabilitation and postural rehabilitation devices. Mirror therapy exploits the theory of mirror neurons, where the observation or even mind representation of the movement facilitates the activation of brain areas involved in the performance of motor tasks . The use of mirror therapy has been generalized and rationalized, especially for the upper limb, with highly suspected results on motor and functional recovery.
Virtual reality rehabilitation robotics is a technique proposing visual, auditory and haptic feedback of the performed task to patients. Computer and robotic technologies allow the manipulation of this feedback (increased errors for example) in order to manage the post-therapy effect and promote learnings . Finally dynamic and static postural evaluation devices are typically included in the definition of technology for sensory afferent modulation. Their relevance in postural rehabilitation, which implies the recovery of several other motor functions, has increasingly been validated.
1.2.5
Neurofeedback rehabilitation
Recent advances in terms of brain signal collection and treatment permit a refined analysis of brain activation areas during the completion of a motor or cognitive task. These recordings are available through functional magnetic resonance imaging (fMRI), near-infrared spectroscopy (NIRS) or electroencephalography (EEG) techniques. However, fMRI, in spite of its excellent spatial and temporal resolution, cannot be mounted onto a device to record brain activity in functional situations. NIRS and EEG, especially when coupled, can record brain activity during motor tasks in daily life or at least in rehabilitation settings.
The collected brain signal can be used for therapeutic objectives :
- •
brain interface coupled to an auditory or visual feedback system (e.g. displacement of a target) can help patients to visualize the effects of brain representation exercises and facilitate the learning of recruiting brain activation ;
- •
brain interface, when associated with a passive or active mobilization of the limb through an external device, either robot-assisted or via FES, can help patients become aware of the recruitment of relevant brain areas and thus influence brain plasticity by facilitating learning. Brain interface coupled with robotic or SEF technologies might also contribute to “closing the sensorimotor loop” and thus promoting the shaping and maybe the emergence of voluntary motor functions;
- •
finally, very recent studies have suggested associating the decoding of this brain signal with brain stimulation techniques, during voluntary tasks. The coupling of these two techniques could help reinforce the mechanisms of adaptive brain plasticity and inhibit maladaptive mechanisms (e.g. inhibition of contralesional activations when they exist).
1.2.6
Brain stimulation
Brain stimulation techniques can be ranked among innovative rehabilitation technologies. They are based on the use of a local magnetic field or galvanic current to stimulate or inhibit certain brain areas, to promote the emergence of motor functions . Repetitive transcranial stimulation (rTMS) or transcranial direct current stimulation (TDCS) can be used in a stimulating or an inhibiting mode according to the characteristics of the generated magnetic field or currents. The spatial resolution in rTMS is better than in TDCS and its application can be associated with neuro-navigation techniques to increase its precision. TDCS bears the advantage of being easy to use and requiring less costly materials.
The effectiveness of these methods is still being debated , even if there are an increasing number of studies in the literature showing some relevance in motor recovery . The most recent studies promote the use of these techniques as a “facilitation” method for other rehabilitation techniques: for example the patient follows an intensive rehabilitation session preceded and facilitated by a TDCS session. In a similar manner, coupling these brain stimulation methods to brain signal recording methods during voluntary movements opens perspectives for new paradigms where the stimulation site will be guided by the management of individual brain map recordings specific to each patient.
1.3
Perspectives
The advent of these technologies applied to rehabilitation is revolutionizing our practices. Brain signal recording techniques associated with the infinite possibilities of behavioral recordings of motor functions or cognitive processes, promote the refined understanding of the mechanisms involved during recovery. This increased knowledge on neural plasticity phenomena, underlying the learning process post lesion, will allow us to individualize very precisely our rehabilitation programs, refine the indications for this or that technique, and, through recovery modeling, define rational therapeutic strategies for a more effective care management. Eventually these technologies will become real “assistants” for rehabilitation professionals. The future probably resides in associating these different techniques to one another. Using these technological tools to help the patient-therapist relationship is a preview of what the rehabilitation of tomorrow will be: a personalized and rationalized training program, greater possibilities of increasing the quantity of rehabilitation training at home without increasing the physiotherapists’ time, appropriation by the patients and their family of some of these tools under the supervision of rehabilitation professionals acting at a distance via web-service platforms. Our goal is to remain vigilant in anticipating these positive and ineluctable advances while preserving the quality of care where direct human interaction remains essential.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
La rééducation du patient hémiplégique a beaucoup évolué ces 30 dernières années . En particulier, de nouveaux modèles organisationnels ont été proposés, allant de la création d’unités spécialisées , au concept d’ early supported discharge , à la « télé-rééducation » , ou au concept d’« auto-rééducation » .
En parallèle à ces évolutions organisationnelles, les méthodes et les moyens mis à la disposition de la rééducation de ces patients se sont considérablement diversifiés, avec une importance de plus en plus grande donnée aux dispositifs technologiques . Cette évolution s’est faite à la faveur des progrès des neurosciences qui nous permettent de mieux comprendre les mécanismes de plasticité cérébrale qui sous-tendent les phénomènes de récupération sensori-motrice et cognitive et à la faveur d’une meilleure intégration des théories de l’apprentissage dans nos programmes de rééducation. Ces progrès ont totalement modifié les principes qui basent nos pratiques rééducatives avec l’avènement d’idées nouvelles comme la notion de rééducation orientée vers la tâche, le regard nouveau que nous portons sur l’importance de l’intensité et de la répétition des exercices, et la remise en question des durées classiquement admises de nos programmes de rééducation. Cette évolution a été très largement influencée par l’émergence des technologies nouvelles qui ont trouvé dans cette pathologie un champ d’application de plus en plus étendu. Enfin, cette évolution des concepts et des pratiques s’est accompagnée d’une évolution très importante des métiers de la rééducation et des organisations sanitaires de prise en charge de ces patients.
Nous nous proposons de réaliser une synthèse non exhaustive des principales technologies appliquées à la rééducation du sujet hémiplégique, à partir d’une revue de la littérature effectuée sur « Medline » et « Web of Science » entre 1990 et 2013.
2.2
Dispositifs technologiques de rééducation
2.2.1
La stimulation électrique neuromusculaire ou fonctionnelle (SEF)
Les courants excito-moteurs ont été proposés il y a plus de 30 ans dans la rééducation du patient hémiplégique. L’utilisation simple de ces courants a rapidement été enrichie de fonctionnalités plus élaborées avec des appareils couplant détection et stimulation qui laissent la motricité propre du patient s’exprimer lors d’une tâche volontaire ( Fig. 1 ), avant de prendre le relais par des courants excito-moteurs . Cette technique a montré une efficacité lorsqu’elle est appliquée au membre supérieur, en particulier chez le patient hémiparétique . Ces dispositifs peuvent parfaitement s’intégrer dans des rééducations dites « orientées vers la tâche », la stimulation électrique étant asservie aux mouvements du patient et les rendant ainsi possibles ou plus faciles à réaliser (SEF). Ainsi la SEF peut être utilisée lors de tâches de marche (système Walkaid ® par exemple) ou lors de tâches de préhension (système Handmaster ® par exemple). Il est intéressant de noter que ce type d’appareils, qui avaient été initialement conçus dans une indication orthétique, semblent avoir un intérêt thérapeutique en améliorant la motricité des muscles stimulés .









