Acute chest trauma to the rib cage can result in rib fractures. Because in children the bones of the rib are less likely to fracture, complete fractures may be rare. The ribs in general are exposed with very little soft tissue covering. Contact sports place the young athlete at greater risk. Also, sports with missiles and sticks have potential to cause rib fractures.
In younger children, the ribs contain more cartilage and less bone. This places children at relatively increased risk of cartilage and soft tissue injury than fractures. Acute fractures of the lower ribs can result from direct blunt trauma to the chest wall in contact sports like football, hockey, and rugby. High-impact trauma such as automobile, motorcycle, or bicycle accidents result in multiple rib fractures. Chronic repetitive stress of upper body muscles, as in weightlifting, throwing, rowing, and serving sports can result in stress fractures. Forceful contraction against resistance can cause avulsion fractures of the ribs. Traction of the external oblique muscles used in throwing and batting can cause avulsion fractures of the floating ribs.1 Because children have relatively more elasticity, chest wall injuries are less common than their adult counterparts.2 First rib fractures can occur as a result of a fall on an outstretched hand (Figure 37-1). Isolated fractures of the upper four ribs are rare since they are protected by the shoulder complex.
The athlete may report feeling of a “pop” or “the wind is being knocked” of him or her. Fractured ribs cause pain with deep inspiration, coughing and sneezing. The deformity of the fractured rib may be palpable, associated with localized tenderness and crepitus. There may be localized swelling and ecchymosis. Because significant energy is required to fracture ribs, this intense energy can result in associated deep organ injury. If the upper ribs are involved, the physician should carefully examine for lung, heart, esophagus, or great vessel injury. If lower ribs are involved, the athlete’s abdomen, back, and flank should be examined for associated liver, spleen, gastrointestinal, or kidney injury.2
Chest x-ray may not only identify rib fractures, but also show the presence of hemothorax or pneumothorax. Rib films should be requested if multiple fractures are suspected. Because the ribs are often difficult to fully evaluate on plain films, a CT scan may show rib fractures more clearly than plain x-ray. The CT scan will be even more beneficial in evaluating underlying organ injury in case of multiple rib fractures or when associated complications are suspected.
Most rib fractures generally heal well without any need for specific treatment. Pain control is important to allow the athlete to take full breaths and prevent atelectasis. A binder may give some relief of pain. Nonunion of these fractures are rare. Multiple rib fractures with associated flail chest may require open reduction internal fixation (ORIF) to stabilize the chest. The athlete can return to conditioning as soon as the pain is tolerable. Contact sports should be limited for 3 weeks. Some have recommended contact sports be limited up to 3 months.
Pneumothorax occurs as air collects between the plural membrane and chest wall. Pneumothorax is a rare occurrence in sports. Most cases reported in the literature are the result of trauma related to participation in football with a peak age of onset at 16 to 24 years, and young children rarely experience these injuries.2
In athletes, pneumothorax can result from direct chest trauma or spontaneously from rupture of the apical blebs. Activities such as weightlifting can result in increased pressure in the chest which can lead to rupture of a bleb.3 Rib fractures can be associated with this injury.
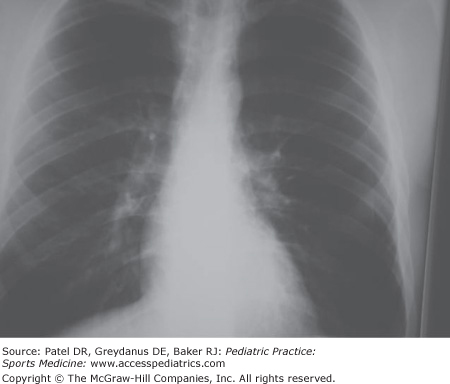
The athlete experiences chest pain on deep inspiration, shortness of breath, and tachycardia. Breath sounds are diminished over the affected area. The pneumothorax may be stable or may be expanding or “tension” pneumothorax (Figure 37-2). The tension pneumothorax is a medical emergency and should be identified clinically when there is rapidly deteriorating shortness of breath (Figure 37-3). Trachea may be deviated to the uninvolved side. A rattling sound or sensation in the anterior chest is known as Hagemen’s sign and indicates pneumomediastinum.
If clinical signs suggest tension pneumothorax in an unstable patient, treatment should be started rather than delayed while awaiting an x-ray. For the stable patient with pneumothorax, the x-ray should be obtained to confirm the diagnosis and treatment based on percent of lung collapse.
The tension pneumothorax can be aspirated immediately with 14 gauge needle inserted in the second intercostal space. Placement of a chest tube or catheter will allow the lung to re-expand. Percentage of lung collapse is estimated on the chest film. Stable pneumothorax less than 20% can be observed and managed conservatively. Pneumothorax greater than 20% should be re-expanded with placement of chest tube. Oxygen administration is indicated and will help with dyspnea. In cases of recurrent pneumothorax, surgical pleurodesis will be required. Return to sports should not be attempted prior to 2 weeks following complete resolution with gradual return to unrestricted sports participation over the subsequent 8 to 12 weeks.
Direct trauma to the anterior chest wall can result in concussion of the heart. Should this concussion occur during the repolarizing cycle of the heart, arrythmias can occur.4 This leads to ventricular fibrillation and sudden cardiac death. Commotio cordis, as this is sometimes called, has resulted in deaths in young children.
Direct trauma to the anterior chest can lead to the accumulation of fluid in the pericardial sac or pericardial tamponade. As fluid accumulates, the cardiac function is compromised. The ventricles cannot fill, cardiac output decreases, and cardiogenic shock results. The classic findings on examination are jugular vein distention, hypotension, and muffled heart sounds. The ECG may show sinus tachycardia with electrical alternans and PR segment depression.4 Immediate decompression under ultrasound guidance is the treatment. Full recovery is expected with early intervention and the athlete can return to sports following recovery.
Any young athlete participating in contact sports should use the appropriate protective equipment. In football and hockey, shoulder pads that are appropriately fitted and in good repair will protect the upper ribs. Protective rib pads, which cover the lower ribs, are available for contact sports as well. For baseball players, catchers should use appropriate chest protectors.
Direct trauma following a collision with opposing player, projectile, or stick to the chest or breast area may result in a contusion, hematoma, abrasion, and/or laceration of the breast. With the exception of horse bite in equestrian sports, chest and breast injuries are rarely reported in the literature. This may because of less severity of injury, rare occurrence, and or gender differences in the incidence of such injuries. Accident-prone sports such as biking, road racing, mountain biking, skiing, and rodeo may have a higher risk for these injuries. Though most collision sports such as hockey, football, baseball, and field hockey provide some chest protection for at-risk players, trauma can occur.5
Velocity of the unsupported breast can be significant, so large breasted women (i.e. C & D cup) are at an increased risk. Poor fitting of protective equipment will put the athlete at risk especially in collision sports. Hard or metal bra parts such as straps, metal hooks, clips, and underwire can cause breast injury in athletes.
Athletes presenting with local pain following trauma may be associated with bruising, swelling, or laceration of the breast tissue. Nipples can become irritated and painful because of chaffing. Males with gynecomastia are at an increased risk by virtue of added breast tissue. On examination swelling, mass, bruising, and hematoma can be identified. Masses should be localized and characterized in terms of density, consistency, movement, and pulsation. Axillary lymphadenopathy should be also noted.
Rarely, hematomas may become secondarily infected. Trauma of the chest and breast may lead to Mondor’s disease or thrombophlebitis of superficial breast veins. Occasionally, breast trauma and pain will uncover tumors and masses. Complications following trauma include fat necrosis, induration, mastitis, scarring, and calcification.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree