Infections
Felon
General Information
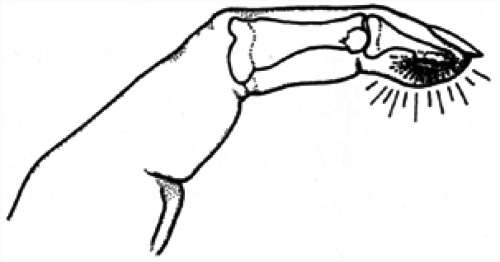
A felon is a deep infection of the finger pulp (Fig. 1), and accounts for approximately 15% of hand infections. There is usually a history of a puncture wound or an open injury to the digit. Staphylococcus aureus is the usual causative organism. The infection is trapped between the vertical septae that divide the pulp and stabilize the skin.
Diagnostic Criteria
Clinically, the patient has a throbbing pain at the tip of the digit. The pain and swelling can develop quickly. The pulp is tightly swollen, tender, and erythematous. Purulence may be present. Cultures of any purulent material should be taken. One should look for the potential complications of an untreated felon, including osteomyelitis of the distal phalanx, pyogenic arthritis of the distal interphalangeal joint, flexor tenosynovitis, and skin necrosis.
X-rays of the finger should be taken to rule out the presence of a foreign body or distal phalangeal osteomyelitis.
Treatment
Nonoperative treatment may be used in treating an early felon with mild swelling or infection that is already adequately draining. Nonoperative treatment includes the use of warm soaks, intensive local wound care, oral antibiotics, and careful follow-up.
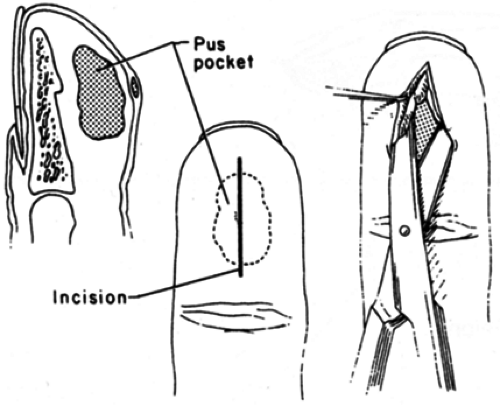
Operative treatment is used in treating a felon with moderate or severe symptoms, the presence of osteomyelitis, septic arthritis, or flexor tenosynovitis. Treatment should then include incision and drainage of the felon. A unilateral longitudinal incision is made near the nail skin margin. The incision may be extended to the tip of the digit (Fig. 2). Radial border incisions are made on the
thumb and little fingers. Ulnar border incisions are made on the index and long fingers. Either radial or ulnar border incisions can be made on the ring finger. If the abscess presents in the digital pulp, then an incision may be made in that area (Fig. 3). The vertical fibrous septae within the pulp should be fully divided to ensure that the felon is completely drained. Care should be taken not to cross the flexion creases at a right angle or violate the flexor tendon sheath. The wound should be left open and packed with a small sterile gauze wick. Flexor tenosynovitis or septic arthritis should also be adequately débrided. Any infected bone should be removed. A partial digital amputation may be needed for chronic osteomyelitis. Daily dressing changes should be performed. Warm soaks or whirlpool treatment may be needed.
thumb and little fingers. Ulnar border incisions are made on the index and long fingers. Either radial or ulnar border incisions can be made on the ring finger. If the abscess presents in the digital pulp, then an incision may be made in that area (Fig. 3). The vertical fibrous septae within the pulp should be fully divided to ensure that the felon is completely drained. Care should be taken not to cross the flexion creases at a right angle or violate the flexor tendon sheath. The wound should be left open and packed with a small sterile gauze wick. Flexor tenosynovitis or septic arthritis should also be adequately débrided. Any infected bone should be removed. A partial digital amputation may be needed for chronic osteomyelitis. Daily dressing changes should be performed. Warm soaks or whirlpool treatment may be needed.
Cultures should be taken. Antistaphylococcal antibiotics (e.g., penicillinase-resistant penicillin or cephalosporins) usually are given. Antibiotic coverage may need to be changed, depending on the lack of clinical improvement and sensitivities of the cultured bacteria. The antibiotics should be used for an adequate
enough time to allow for clinical improvement. Six weeks of intravenous antibiotics may be needed to treat osteomyelitis.
enough time to allow for clinical improvement. Six weeks of intravenous antibiotics may be needed to treat osteomyelitis.
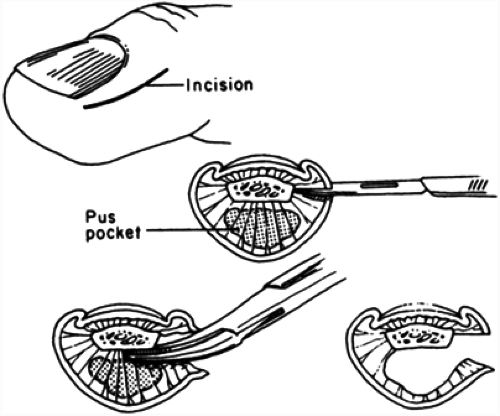 FIG. 2. Drainage of a felon using a midlateral incision. Complete division of the vertical septae should be performed. |
Paronychia
General Information
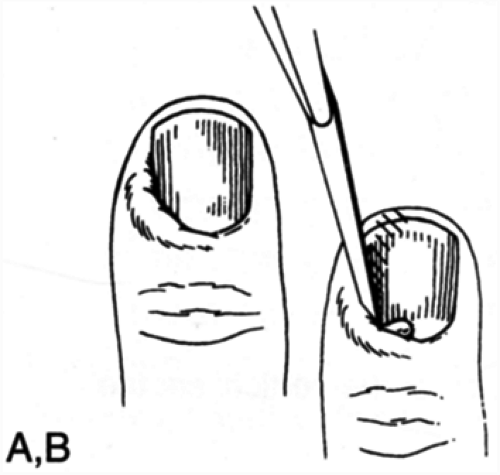
A paronychia is an infection that involves the soft tissues around the fingernail (Fig. 4). If the eponychial fold is involved, the infection is referred to as an eponychia, and if the infection invades beneath the nail as well, it is called a subungual abscess.
The usual causative organism is Staphylococcus aureus that has been introduced into the paronychial tissue by some trauma (e.g., manicure, a sharp corner of a nail, or a hangnail). In children, thumb sucking can introduce mouth flora and produce an infection. In early stages, the infection may only be superficial to the nail; it may later extend around the border of the nail into the subungual space, resulting in nail destruction; still later, it may invade bone and cause osteomyelitis.
Diagnostic Criteria
A history of precipitating trauma, increasing tenderness, erythema, swelling, and pain is usually noted. Clinically, localized swelling alongside the nail to generalized swelling of the entire distal portion of the distal phalanx in severe cases is seen. The early signs include diffuse inflammation and later abscess formation with fluctuation. Purulence may be present. Cultures of any purulent material should be taken. A herpetic whitlow (see the following), characterized by painful, clear vesicle formation, should be excluded. These infections are reported in health care workers whose hands are in contact with mouth flora (e.g., dentists and anesthesiologists).
X-rays of the finger should be taken to rule out the presence of a foreign body or distal phalangeal osteomyelitis.
Treatment
Nonoperative treatment is used in treating early paronychia with mild swelling or infection that is already adequately draining. Treatment options include trimming of a hangnail or sharp border of a nail, frequent hand washings and/or soaks, and antistaphylococcal antibiotics.
Operative treatment is used in treating paronychia with moderate or severe symptoms, a subungual abscess, felon, or osteomyelitis. Care is taken to apply the digital block proximal to the area of infection. Treatment options include incisional drainage with or without nail plate removal. Elevating the nail margin can drain the abscess (Fig. 4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree