Abstract
Compression therapy has precise technical characteristics but in vivo pressures exerted by bandages are still poorly understood.
Objective
To perform in vivo pressure measurements of different compression bandages bearing different technical characteristics with different application methods.
Method
Interface pressure was measured on the lower limb of 20 healthy women at 3 different points (B1, C and F) using 6 compression techniques (stockings, non-elastic bandage, elastic bandages with 2 technical characteristics and 3 application methods), and in 3 positions.
Results
All elastic compression bandages respected the principle of graduated pressure along the length of the limb ( P < 0.0001), but not the non-elastic bandage. The pressures increase significantly ( P < 0.0001) between the supine position and the sitting or standing position, especially with the non-elastic compression bandage. There is a marked variation in pressures between subjects for some bandages (non-elastic and elastic applied using the figure-of-eight technique). The pressure increases significantly with the number of bandage overlaps ( P < 0.01).
Conclusion
Elastic and non-elastic bandages behave differently from one another, and non-elastic bandages not appearing to comply with medical recommendations concerning graduated pressure. There is a high level of variability between subjects for some compression bandages (non-elastic and figure-of-eight methods).
Résumé
Un traitement compressif répond à des caractéristiques techniques précises mais les pressions in vivo exercées par les bandes restent mal connues.
Objectif
Mesurer in vivo la pression de différentes bandes ayant des caractéristiques techniques différentes et selon différentes techniques de pose et positions du sujet.
Méthode
Les pressions ont été mesurées sur la jambe droite de 20 sujets sains féminins à 3 niveaux différents (B1, C et F) selon 6 modes de compression (bas, bande non élastique, bandes élastiques avec 2 caractéristiques techniques et 3 techniques de pose différentes), et dans 3 positions.
Résultats
Les bandes élastiques respectent le principe de dégressivité des pressions le long du membre ( p < 0,0001) mais pas la bande non élastique. Les pressions de chacune des bandes testées augmentent significativement ( p < 0,0001) de la station allongée à assise ou debout, en particulier avec la bande non élastique. Il existe une forte variation inter-sujets des pressions pour certaines bandes (non élastique et élastique posée en épis). La pression augmente significativement avec le nombre de recouvrements ( p < 0,01).
Conclusion
Les bandes élastiques et non élastiques ont des comportements différents, les bandes non élastiques ne semblant pas respecter les recommandations médicales de dégressivité. Il existe une grande variabilité inter-sujets sur certaines bandes (non élastique et élastique posée en épis).
1
English version
1.1
Introduction
Elastic stockings and elastic compression bandages are the cornerstone of chronic venous disease therapy, particularly in chronic venous and lymphatic insufficiency. These medical devices are designed to exert pressure on the skin surface in order to prevent (or control) the symptoms or detrimental effects of certain pathologies (edema, lipodermatosclerosis, leg ulcers, etc.). It has been very widely demonstrated that the use of compression bandages induces a variety of complex physiological and biochemical effects on the venous, arterial and lymphatic systems . If the applied pressure, application technique and device used are perfectly adapted to the pathology treated, this compression therapy can help reduce the edema, restore valve function, limit swelling of the lower limbs when standing and relieve pain while also promoting the healing of leg ulcers caused by venous insufficiency .
A variety of different medical devices exist, including compression stockings, elastic and non-elastic bandages, multi-layer kits, etc. . Various technical and pressure recommendations have been made on the use of these compression devices . In contrast, the classification of bandages remains unclear. Sometimes they are categorized based on their stretching ability (short, medium or long) and sometimes their behavior (rigid, non-elastic or elastic) . The pressure exerted by bandages depends on the application method, bandage tension and on the radius of curvature of the area covered. The spiral and figure-of-eight techniques (spica method) are classic application methods, yet several unanswered questions remain, such as the ideal pressure to be exerted as well as the pressure variability between the different techniques. .
The level of pressure exerted from a medical device answers to the Laplace equation stating that the pressure (P in hPa) of a compression applied to the skin surface is proportional to the tension (T in cN/cm) of the compression material and inversely proportional to the radius of curvature (R in cm) of limb surface to which it is applied, i.e. P = T/R. To measure this level of pressure, several methods exist. Interface pressure is the pressure exerted by the device (i.e. stockings or bandages), which in clinical practice is the skin of the limb under the compression device .
For compression stockings, various standards exist for in vitro measurements of the pressure exerted, depending on the size of the compression stockings (AFNOR standards). These standards make it possible to identify the pressure exerted by the stockings and define its class. Nowadays, this measurement procedure only applies to stockings. Compression bandages bear very precise technical characteristics: structure, stretching ability upon application, tension under the stretched bandage as well as elastic or non-elastic ability. Standards exist for classifying bandages. Some can be used to accurately measure the force and stretch characteristics (AFNOR standards) while others define bandages on the basis of parameters entirely unrelated to these notions of force (DIN standards). Anyway, no standard can estimate, as it is the case with compression stockings, the in vitro pressure exerted by compression bandages.
More recently, the problem of in vivo assessment has been raised, i.e. the pressure applied by the compression device on the surface of the skin. Various in vivo measurement systems have been proposed: pneumatic and pneumatic-electric; piezoelectric; resistant-based or with a tension and capacity gauge, with a high level of variability for the measurement methods . Partsch et al. carried-out measurement procedures in various positions and compared in vitro and in vivo methods. They observed an acceptable correlation between these two measurement methods, and thus it helped promote in vivo methods. However, real in vivo pressures exerted on the skin by a bandage are still poorly understood. Furthermore, the pressure actually exerted is operator-dependent, i.e. pressures obtained vary from one operator to the next and even for the same operator, from one application to the next .
In vivo pressure measurement devices now appear essential. They offer new avenues and are strongly recommended by certain authors because they are easy to use and offer the possibilities of direct sub-bandage measurement. In this context, this study was designed to measure in vivo the interface pressure of compression bandages produced by a manufacturer whose compression therapy products make up most compression bandages distributed in France, with different technical characteristics (e.g. elastic and non-elastic, tension under the stretched bandage) and applied using different methods. The objective was to benchmark these devices against one another and evaluate the pressures really applied according to the different characteristics. The influence of the subject’s position was also be evaluated according to the type of bandages used.
The French compression classification was chosen as the reference. Hence there are 4 different compression classes according to French regulatory standards (AFNOR G30 102, 1986): class 1: pressure of 10 to 15 mmHg; class 2: pressure of 15.1 to 20 mmHg; class 3: pressure of 20.1 to 36 mmHg; class 4: pressure greater than 36 mmHg.
1.2
Methods
1.2.1
Subjects
Twenty healthy female subjects agreed to take part in this study ( Table 1 ). All subjects underwent a prior physical examination in the Department of Physical Medicine and Rehabilitation within the Saint-Étienne University Hospital in order to verify that they met the following inclusion criteria: healthy females, having never been pregnant, aged between 18 and 30 years, volunteers for the study, with a normal body mass index (BMI) (between 18.5 and 25 kg/m 2 ); free of any functional vascular symptoms in the lower limbs; absence of neurological, rheumatologic, cardiovascular, respiratory or metabolic affection that could have an impact on the vascular functions of the lower limbs or mobility; absence of traumatic lesion or history of surgery of the lower limbs or pelvis; absence of functional impairments affecting gait abilities or the ability to switch freely between supine, sitting and standing positions.
| Age (years) | Height (cm) | Weight (kg) | BMI | Perimeter | Total leg length (cm) | Lower leg length (cm) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B (cm) | B1 (cm) | C (cm) | Knee (cm) | F (cm) | |||||||
| Mean | 20.7 | 1.6 | 55.7 | 20.7 | 20.8 | 25 | 34.4 | 35.8 | 50.4 | 88.5 | 40.4 |
| SD | 2.8 | 0.05 | 5.7 | 1.8 | 1.1 | 1.5 | 2.6 | 2.2 | 4.6 | 4.5 | 2.8 |
| Min | 18 | 1.5 | 45 | 18.4 | 18 | 22 | 28 | 31 | 40 | 78 | 34 |
| Max | 30 | 1.7 | 68 | 25.9 | 23 | 27 | 40 | 41 | 61 | 94 | 47 |
All subjects had a morphology corresponding to a size 1, length N of the compression stockings proposed in this study.
All subjects agreed to sign the informed consent form.
The study was approved by the Loire Ethics Committee (2010-A00362-37).
1.2.2
Study protocol
One pair of stockings, three compression bandages and different application methods, amounting to a total of 6 different compression methods, were applied to the right leg of the 20 subjects. In vivo interface pressures were measured in the supine, sitting and standing positions.
Subjects were placed in the supine position on an examination table, with the heel resting on a platform to prevent any contact between the calf and the table. Three sensors were positioned inside the right leg and fixed to the skin with adhesive tape, at three different points as recommended by Partsch et al. : on the ankle at point B1: above the medial malleolus, below the medial gastrocnemius muscle in front of the Achilles tendon and at the back of the tibia (“area where the Achilles heel becomes a muscle, approximately 10 to 15 cm from the internal malleolus”); on the calf, at point C: located on the medial side of the leg, at the calf’s greatest circumference; on the thigh, at point F, on the medial surface, midway between the kneecap and the groin ( Fig. 1 ).

Following the application of the sensors, the 6 compression methods studied were successively tested, the order of application was randomly determined. Bandages were applied starting at the toes, going under the heel and then right up the leg to the top of the thigh.
Throughout the study, the same qualified operator, who had received practical training on the application of compression bandages, was in charge of all applications.
1.2.3
Materials
Four compression systems were used, based on their routine use in France:
- •
Venoflex Kokoon ® compression stockings for women (Thuasne, Levallois-Perret, France), class 2 (graduated pressure of 15.1 to 20 mmHg from the ankle to the top of the thigh at point B, according to the French classification and AFNOR standards NF G30 102B. Composition: polyamide: 60%; elastane: 40%. Stockings size was adapted to the morphology of each subject on the basis of: ankle circumference, thigh circumference and leg length (floor-groin height);
- •
an elastic Biflex ® 16 compression bandage (Thuasne, Levallois-Perret, France) with a maximum stretch capacity greater than 100%, calibrated, 7 m × 10 cm. Composition: viscose: 58%; polyamide: 19%; cotton: 16.5%; elastane: 6.5%. For this bandage, three application methods were used: bandage applied with a 50% overlap (i.e. 2 layers) and an elastic bandage stretch of 30% (the calibrated rectangle becomes a square); bandage applied with a 75% overlap (i.e. 3 layers) and an elastic bandage stretch of 30% (the calibrated rectangle becomes a square); bandage applied using the figure-of-eight technique (spica method), without stretching the bandage, with a space between overlap layers of 1.5 cm (approximately one finger width);
- •
an elastic Biflex ® 17 compression bandage (Thuasne, Levallois-Perret, France) with a maximum stretch capacity greater than 100%, calibrated, 5 m × 10 cm. Composition: viscose: 61%; polyamide: 18%; cotton: 10.5%; elastane: 10.5%. For this bandage, only one application method was used: bandage applied with a 50% overlap and a 30% elastic stretch of the bandage (the calibrated rectangle becomes a square);
- •
a non-elastic Biflexideal ® compression bandage (Thuasne, Levallois-Perret, France) with a maximum stretch capacity inferior to 100%, 5 m × 10 cm. Composition: viscose: 36%; polyamide: 46%; cotton: 17.5% elastane: 0.5%. For this bandage, only one application method was used: bandage applied with a 50% overlap and bandaged stretched to 80% of its maximum stretching capacity.
Therefore, the study evaluated a total of 6 compression devices and/or application methods. These 6 conditions were justified by the fact that we wanted to assess: 1) the influence of bandage tension on the pressure exerted (difference in tension between Biflex ® 16 and 17); 2) the influence of elastic versus non-elastic behavior on the pressure exerted; 3) the influence of two traditional application techniques (spiral or figure-of-eight) and number of overlaps applied (Biflex ® 16 with 2 or 3 overlaps) on the pressure exerted.
The technical characteristics of the compression bandages are described in Table 2 .
| Bandage | Weight (in g/m 2 ) | Maximum stretch (in %) | Stretch upon application (in %) | Tensile strength when stretched upon application (in N/m) | Stiffness (in N/m.mm) |
|---|---|---|---|---|---|
| Biflex ® 16 | 475 | 153 | 30 | 50.9 | 1.05 |
| Biflex ® 17 | 525 | 122 | 30 | 112.2 | 1.57 |
| Biflexideal ® | 261 | 70 | 56 | 178.8 | 12.3 |
Each sensor was connected to a PicoPress ® interface pressure measurement system (MicroLab Elettronica, Ponte S. Nicolo, Italy) with an acquisition frequency of 4 Hz and a flexible sensor with a diameter of 5 cm, enabling interface pressure measurements.
Hence three independent systems simultaneously recorded measurements from the three sensors positioned at the three reference points described above.
The PicoPress ® system is a portable digital gauge specially designed to measure the pressure exerted by a bandage, its reliability and reproducibility have already been demonstrated and it is know as one of the best systems for measuring interface pressure . The ultra-slim circular sensors, into which a known amount of air was introduced, were placed between the limb and the bandage. The pressure detected by the sensor was measured using a digital microprocessor gauge and visualized via an alphanumeric display. The system incorporates a micro-pump that is manually activated to insufflate a pre-determined volume of air.
1.2.4
Measurements
Interface pressure measurements were taken on the right leg for each of the bandages and in 3 successive positions:
- •
supine position, arms alongside the body, heel slightly raised so that the calves are not in contact with the table surface;
- •
sitting position, legs still, at a 90 degree angle, arms alongside the body;
- •
standing position, feet apart at pelvis width, standing still, arms alongside the body.
A 2 min rest period without moving was mandatory before each measurement. The pressure recorded was the highest pressure noted on the screen.
In order to test the reproducibility of bandage applications, for each of the subjects, each bandage was removed and applied again at the end of each measurement. This way, three measurements were successively taken for the same subject and the same bandage, at the three reference points, and in each position.
Inter-subjects pressure variations were also evaluated.
1.2.5
Statistical analysis
We used a repeated-measures analysis of variance (ANOVA) to determine: the effects of the bandage type and application method (“bandage” effect) on interface pressure for each of the three measurement points and according to the subject’s position; the effects of the three measurement points (“gradient” effect) for each bandage and in each position; the effects of the subject’s three positions (“position” effect) for each bandage and at each measurement point; and, finally, the reproducibility of bandage applications.
The individual effects were analyzed by a Fisher post-hoc test.
The dispersion of the recorded pressures within the study population (dispersion between subjects) was assessed by the coefficient of variation.
Correlations between the pressures exerted by the Biflex ® 16 bandage applied using a spiral technique with two overlaps and the Biflex ® 17 bandage applied using a spiral technique with two overlaps were evaluated with a correlation Z test.
The significance threshold was set at P < 0.05.
1.3
Results
We measured in vivo the interface pressures exerted by the stockings as well as different types of medical compression bandages and according to the different application methods and subject’s position ( Table 3 ).
| Supine | Sitting | Standing | Moving from supine to sitting position | Moving from supine to standing position | |
|---|---|---|---|---|---|
| Venoflex Kokoon ® class 2 stockings | |||||
| B1 | 12.9 ± 0.2 | 14.8 ± 0.2 | 14.5 ± 0.3 | + 1.9 mmHg | + 1.6 mmHg |
| C | 10.5 ± 0.3 | 13.0 ± 0.4 | 12.7 ± 0.4 | + 2.5 mmHg | + 2.2 mmHg |
| F | 7.4 ± 0.2 | 6.5 ± 0.2 | 7.4 ± 0.3 | − 1.0 mmHg | 0.0 mmHg |
| Biflex ® 16 – 2 overlaps | |||||
| B1 | 33.8 ** ± 0.8 | 36.8 ± 0.8 | 36.0 ± 0.9 | + 3.0 mmHg | + 2.2 mmHg |
| C | 28.1 ** ± 0.9 | 30.8 ± 0.9 | 30.3 ± 0.9 | + 2.7 mmHg | + 2.2 mmHg |
| F | 19.0 ± 0.5 | 17.5 ± 0.4 | 19.8 ± 0.9 | − 1.5 mmHg | + 0.8 mmHg |
| Biflex ® 16 – 3 overlaps | |||||
| B1 | 62.6 ** ± 0.9 | 68.0 ± 1.2 | 65.6 ± 1.2 | + 5.3 mmHg | + 3.0 mmHg |
| C | 51.4 ** ± 1.5 | 58.5 ± 186 | 54.5 ± 1.5 | + 7.1 mmHg | + 3.1 mmHg |
| F | 32.6 ± 0.9 | 30.6 ± 0.9 | 31.6 ± 0.9 | − 2.0 mmHg | − 1.0 mmHg |
| Biflex ® 16 – figure-of-eight | |||||
| B1 | 33.1 ** ± 1.2 | 42.0 ± 1.3 | 44.2 ± 1.3 | + 8.9 mmHg * | + 11.1 mmHg * |
| C | 21.7 ** ± 0.7 | 30.5 ± 0.9 | 31.4 ± 0.9 | + 8.8 mmHg * | + 9.7 mmHg * |
| Biflex ® 17 – 2 overlaps | |||||
| B1 | 64.4 ** ± 1.4 | 68.4 ± 1.4 | 66.8 ± 1.5 | + 4.0 mmHg | + 2.4 mmHg |
| C | 52.3 ** ± 1.5 | 56.8 ± 1.8 | 55.4 ± 1.8 | + 4.5 mmHg | + 3.0 mmHg |
| F | 35.3 ± 1.2 | 34.1 ± 1.2 | 34.7 ± 1.2 | − 1.2 mmHg | − 0.6 mmHg |
| Biflexideal ® | |||||
| B1 | 44.1 ** ± 1.5 | 52.5 ± 2.0 | 53.8 ± 1.8 | + 8.4 mmHg * | + 9.7 mmHg * |
| C | 43.9 ** ± 1.8 | 55.6 ± 1.9 | 54.2 ± 1.9 | + 11.7 mmHg * | + 9.3 mmHg * |
| F | 27.1 ± 1.0 | 25.2 ± 1.2 | 28.2 ± 1.1 | − 1.9 mmHg | + 1,1 mmHg |
1.3.1
“Pressure gradient” effect
The results showed that, regardless of application methods (spiral or figure-of-eight techniques), the elastic compression bandages (Biflex ® 16 or Biflex ® 17) respect the principle of pressure gradient along the length of the limb ( Fig. 2 ). The pressures measured decreased significantly ( P < 0.0001) from the ankle (point B1) to the top of the thigh (point F). This result is similar to the one reported for compression stockings ( Table 3 ).
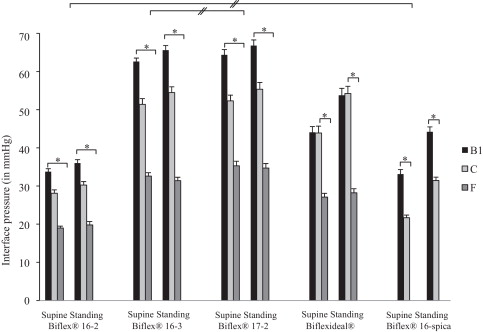
Conversely, for the Biflexideal ® non-elastic bandage, no pressure difference was observed between the ankle and calf (between point B1 and C, P > 0.05).
1.3.2
“Subject position” effect on interface pressures
The results underlined that, regardless of the application method (spiral or figure-of-eight techniques), interface pressures significantly increased ( P < 0.0001) from the supine position to the sitting or standing position at points B1 and C, i.e. at the ankle and calf ( Table 3 and Fig. 2 ). No difference was observed at the thigh at point F ( P > 0.05). Similarly, no significant differences in pressures were observed between the sitting and standing positions ( P > 0.05).
Repeated ANOVA unveiled that, when switching from the supine to the sitting or standing position ( Table 3 ), the increase in interface pressure at B1 or C was significantly higher with the Biflexideal ® and Biflex ® 16 bandages applied using the figure-of-eight technique compared to other bandage types or application methods ( P < 0.01).
1.3.3
“Bandage and techniques” effects on interface pressures
Stockings yielded a significantly lower pressure ( P < 0.001) than bandages for all measurement points and in all positions ( Table 3 and Fig. 2 ).
There was no pressure difference between the Biflex ® 16 elastic bandages, applied using a spiral technique with 3 overlaps, and Biflex ® 17, applied using a spiral technique with 2 overlaps ( P > 0.05), at points B1 and C, and for all positions. Average pressures obtained for these two bandages were respectively 62.6 mmHg and 64.4 mmHg (at point B1 in the supine position) or 65.6 mmHg and 66.8 mmHg (point B1 in the standing position).
There was no significant pressure difference with the Biflex ® 16 elastic bandage using the figure-of-eight t vs. the spiral technique, with 2 overlaps, at point B1 (supine) and at point C (sitting and standing) ( P > 0.05).
1.3.4
Inter-operator reproducibility of application
A repeated-measures ANOVA showed no significant difference for the pressures recorded during the 3 successive applications for each bandage ( P > 0.1).
1.3.5
Inter-subject reproducibility of application
Within the studied population, the coefficients of variation in the supine position ranged from 6 to 18%. In fact, for stockings they were respectively 8%, 12%, 14%, at points B1, C and F; for the Biflex ® 16 elastic bandage, applied using the spiral technique, with 2 overlaps: they were respectively 10%, 14%, 11%; for the Biflex ® 16 elastic bandage, applied using the spiral technique, with 3 overlaps: they were respectively 6%, 13%, 12%; for the Biflex ® 16 elastic bandage, applied using the figure-of-eight technique: 16% and 15%; for the Biflex ® 17 elastic bandage, applied using the spiral technique, with 2 overlaps: they were respectively 10%, 13%, 16% and finally for the Biflexideal ® non-elastic bandage the coefficients of variation were respectively 16%, 18%, 16%.
1.3.6
Correlation between the pressures of the Biflex ® 16 and Biflex ® 17 elastic bandages
Correlations between the pressures exerted by the Biflex ® 16 elastic bandage applied with two overlaps and the Biflex ® 17 elastic bandage applied with two overlaps were significant for all the measurement points and in all positions ( P < 0.01, Table 4 ).
| Correlation coefficient. Biflex ® 16-2 vs Biflex ® 17-2 | ||
|---|---|---|
| B1 | C | |
| Supine | r = 0.69 P < 0.0005 | r = 0.69 P < 0.0004 |
| Sitting | r = 0.71 P < 0.0003 | r = 0.56 P < 0.008 |
| Standing | r = 0.73 P < 0.0001 | r = 0.54 P < 0.01 |
1.4
Discussion
1.4.1
Pressure variation exerted when switching position
Results showed that the interface pressure exerted by the different types of bandages was significantly lower in the supine position than in the sitting or standing position, and it was almost identical between the latter two positions.
The lowest pressure was obtained with the Biflex ® 16 bandage, applied using the spiral technique with two overlaps or using the figure-of-eight technique. In both these cases, a class 3 pressure was obtained at point B1 in the supine position. For the other bandages or application methods, the pressure exerted was class 4. After moving from the supine to the standing position, the interface pressure at point B1 increased by more than 9 mmHg for the Biflexideal ® bandage or the Biflex ® 16 bandage applied using the figure-of-eight technique. When the Biflex ® 16 and 17 bandages were applied using the spiral technique with 2 or 3 overlaps, the pressure did not increase over 3 mmHg. Similar results were observed at point C.
Upon switching from the supine to the standing position, there was a marked increase in hydrostatic pressure , and hence an increase in leg volume. This increase will not have the same impact under the effects of elastic vs. non-elastic compression. The choice of elastic or non-elastic devices, stockings or bandage, is based on the level of compression required. Biflex ® 16 and 17 elastic bandages exhibit a low stiffness (less than 2 N/m.mm, Table 2 ). Thus, a low variation in bandage stretch leads to a low variation in bandage tension and therefore in interface pressure. Conversely, the Biflexideal ® bandage exhibits a high stiffness (12.3 N/m.mm, Table 2 ). In this case, a low variation in bandage stretch leads to a marked variation in bandage tension and therefore in interface pressure. For the Biflex ® 16 bandage, applied using the spica method, it is the application technique that triggers this result.
The difference between elastic and non-elastic compression bandages has been studied on numerous occasions . Callam et al. demonstrated that elastic bandages maintained their pressure for a longer period and over time. However, non-elastic bandages appeared to exert a strong intermittent pressure, which was relatively low at rest, and therefore well tolerated, and high during muscle exercise . These results were obtained in the static position. They cannot be extrapolated to the interface pressures exerted while walking. When walking, the leg volume will decrease compared to the standing position . Therefore it is probable that pressure variations observed while walking are lower than those measured when switching from a supine to a standing position. It would be worth conducting further studies to validate this hypothesis.
1.4.2
Application reproducibility
If the operator is well trained and carefully follows the application recommendations noted in the instructions for use, the intra-operator reproducibility is good and does not yield any significant difference in pressures between the different tests. However, in order to use the Gold Standard, i.e. the intra-class correlation (ICC), we would have needed more subjects to test this reproducibility. In addition, further studies would be relevant to assess inter-operator reproducibility.
Although the reproducibility study did not show any significant pressure differences between the different applications, results nonetheless showed a relatively high disparity in pressure measurements between subjects, especially for the Biflex 16 ® bandage applied using the figure-of-eight technique and the Biflexideal ® non-elastic bandage. In fact, for the former, in the supine position for example and at point B1, the pressure measured could vary from 24 to 42 mmHg between 2 different subjects; and from 35 to 59 mmHg for the latter. For the Biflexideal ® non-elastic bandage, this could be explained by the fact that the bandage was applied at a stretching level very close to its maximum stretch capacity. In this area, a small stretch variation upon application leads to a marked variation in bandage tension and hence in the pressure exerted. This is what the stiffness reflects, as shown in Table 2 . In addition, because of its non-elastic nature, the bandage tension – and thus the pressure – falls rapidly once this bandage is stretched. For the Biflex ® 16 bandage applied using the figure-of-eight technique; the results could be explained by the application method. This method is indeed more difficult to control than the spiral technique. For Coull et al. , the spiral technique was a safe and comfortable method of bandage application. The figure-of-eight method also provided graduated compression but with some areas exhibiting high pressure, notably over the Achilles tendon.
Moreover, as demonstrated by Hafner et al. and Keller et al. , experience and regular training are required to ensure the reliability of bandage application and the reproducibility of the pressure exerted by the bandage.
1.4.3
Graduation of pressures along the length of the leg
Our study confirms that elastic and non-elastic bandages behave differently . Our results reveal that elastic bandages fully comply with the graduation of pressures, regardless of application methods. Conversely, the non-elastic Biflexideal ® bandage demonstrates more marked pressure variations and does not appear to respect medical recommendations for pressure graduation along the length of the leg.
According to the literature, non-elastic bandages have a significant effect on venous hemodynamics and help improve the efficacy of the calf’s muscle pump, by generating a higher pressure in the calf, particularly while walking . Its effects have been demonstrated in the treatment of lymphatic diseases, particularly in terms of reducing the volume of the limb affected by lymphedema .
Compression stockings and elastic compression bandages behave similarly, as long as the application method and bandage stretch upon application are mastered.
1.4.4
Relationship between application method and interface pressure
According to the literature , the higher the number of overlaps, the higher the interface pressure becomes. Our study demonstrates that the Biflex 16 ® elastic bandage exerts identical pressures on the lower limb, regardless of whether it is applied using a spiral method with 2 overlaps, or a figure-of-eight technique, in the supine position. These pressures then differ when the subjects are in sitting or standing positions. When the bandage is applied using a spiral method with 3 overlaps, pressure values are almost twice as high compared to those obtained with 2 overlaps (in the supine position: + 85% at point B1, + 83% at point C, + 72% at point F). Indeed, for Thomas et al. , an overlap of 50% corresponds to two layers of bandage, and a 66% overlap corresponds to three layers of bandage.
In addition, in our study pressure values are almost identical between the spiral technique with 2 overlaps and the figure-of-eight technique, even though Barbenel et al. revealed that a figure-of-eight technique applies 1.5 times the pressure of a spiral technique.
1.4.5
Relationship between bandage tension and interface pressure
The main technical difference between the Biflex ® 16 and the Biflex ® 17 elastic bandages is the tension when stretched upon application ( Table 2 ). Correlations between pressures exerted by the Biflex ® 16 bandage applied with two overlaps and the Biflex ® 17 bandage applied with two overlaps are significant for all measurement points and in all positions ( P < 0.01, Table 3 , Fig. 2 ). All other things being equal, these results validate that the interface pressure is indeed related to bandage tension when stretched upon application. The greater the tension, the higher the interface pressure will be.
1.4.6
Study limits
Most compression bandages used in France are elastic bandages. We thus chose to use Biflex ® bandages, which are the most prescribed. Conversely, non-elastic bandages are seldom prescribed and used and the bandage chosen is one of the bandages available on the market, but we chose to keep the same manufacturer. The results of the present study are therefore valid for the products tested, but can also be extrapolated to other compression devices available on the market with identical mechanical characteristics.
In addition, as with the majority of descriptive studies in the literature, this study evaluated healthy volunteers. The results could be different in pathological situations. Additional studies would be useful to compare these results with those obtained in a pathologic population (venous or lymphatic edema, etc.).
1.4.7
Recommendations
If we refer to recent recommendations concerning venous disease in terms of the level of pressure to be exerted, we can therefore conclude that as long as its technical characteristics are fully controlled and the operator strictly follows the instructions recommended by the manufacturer, an elastic compression bandage can be used in the following conditions: stages C2, C3, C4 and C5 of venous disease for elastic compression bandages with a force when stretched upon application of around 50 N/m, applied using a spiral method with two overlaps; stage C6 of venous disease for elastic compression bandages with a force when stretched for application of 112 N/m applied using a spiral method with two overlaps, or 50 N/m applied using a spiral method with three overlaps. In addition, these studies underlined that it is preferable to use elastic bandages in order to guarantee graduated pressures along the length of the limb.
1.5
Conclusion
Although in vivo pressures are increasingly used, few studies have evaluated the relationship between interface pressures, the technical characteristics of the bandages and the application method used. This study demonstrated that the interface pressure exerted depends on the application method and characteristics of the bandage (tension when stretched upon application and elastic or non-elastic behavior according to AFNOR standards NF S97-115).
Two different types of compression bandages can be differentiated. First, elastic compression bandages, with a reproducible application, it provides graduated pressure from the ankle to the top of the thigh which not varies much when switching from the supine to the standing position. Second, non-elastic compression bandages, where application reproducibility is not controlled as well, the pressure is not graduated along the length of the leg, and varies significantly when the subject moves from the supine to the standing position. These results were obtained in a static position. It would be relevant to study interface pressures obtained while walking.
In order to guarantee patients a pressure that complies with current recommendations for the treatment of their disease, not only must the technical characteristics of the bandages be fully controlled, but the application method to be used should also be clearly indicated. The efficient use of the bandage depends on these two conditions.
Disclosure of interest
The authors declare that the manufacturer Thuasne SA participated in this study from a material, human and financial point of view. R. Convert, Director of the Research and Development Department at Thuasne SA participated in the production of this article.
Financing: the authors declare that the manufacturer Thuasne SA funded this study.
2
Version française
2.1
Introduction
La contention et la compression élastique sont la clé de voûte des traitements des affections veineuses chroniques et en particulier de l’insuffisance veineuse chronique et lymphatique. Ces dispositifs médicaux sont destinés à exercer, sur la surface cutanée, une pression visant à empêcher (ou à maîtriser) les symptômes ou les effets néfastes induits par certaines pathologies (œdèmes, hypodermites scléreuses, ulcères, etc.). En effet il a été très largement prouvé que l’utilisation de bandes de compression entraîne divers effets physiologiques et biochimiques complexes concernant les systèmes veineux, artériel et lymphatique . Si la pression appliquée, la technique de pose et le matériel sont parfaitement adaptés à la pathologie traitée, cette compression permet de réduire l’œdème, restaurer la fonction valvulaire, limiter le gonflement des membres inférieurs à l’orthostatisme, soulager la douleur tout en favorisant la cicatrisation des ulcères dus à l’insuffisance veineuse .
Beaucoup de dispositifs médicaux existent, parmi lesquels les bas de contention, les bandes élastiques ou non élastiques, les kits multicouches etc. . Différentes recommandations ont été faites sur l’utilisation de ces dispositifs de compression . A contrario, la classification des bandes est beaucoup plus floue. On les classe tantôt selon leur allongement (court, moyen ou long), tantôt selon leur comportement (rigides, non élastiques ou élastiques) . La pression exercée par les bandes est fonction de la technique de pose, de la tension de la bande, ainsi que du rayon de courbure de la zone qu’elles couvrent. Les techniques de pose dites « en spirale » ou « en épis » constituent des méthodes traditionnelles d’application des bandes, mais il reste beaucoup de questions sans réponse, en particulier sur la pression idéale à exercer, la variation de pression entre les différentes techniques etc. .
Le niveau de pression exercée par un dispositif médical obéit à la loi de Laplace énonçant que la pression (P en hPa) d’une compression exercée sur la surface cutanée, est proportionnelle à la tension (T en cN/cm) du moyen de contention et inversement proportionnelle au rayon de courbure (R en cm) de la surface comprimée, soit P = T/R. Pour mesurer ce niveau de pression, plusieurs méthodes existent. La pression d’interface est la pression exercée par le dispositif (en l’occurrence le bas ou la bande) sur son support, en pratique clinique sur la peau du membre recouvert .
Pour les bas de compression, différentes normes existent afin de mesurer la pression exercée in vitro, en fonction de la taille du bas de compression (normes Afnor). Elles permettent d’identifier la pression exercée par le bas et de situer sa classe. Cette procédure de mesure de pression ne s’applique actuellement que pour les bas. Une bande de compression, quant à elle, répond à des caractéristiques techniques précises : sa structure, son allongement à la pose, sa tension sous cet allongement à la pose, ainsi que son comportement élastique ou non élastique. Des normes existent pour caractériser les bandes. Certaines permettent de mesurer avec précision les caractéristiques de force et d’allongement (normes Afnor) alors que d’autres définissent les bandes selon des paramètres n’ayant aucun lien avec ces notions de forces (normes DIN). Dans tous les cas, aucune norme ne permet d’estimer, comme pour les bas, la pression in vitro exercée par une bande.
Plus récemment a donc été posé le problème d’une évaluation in vivo, c’est-à-dire de la pression appliquée par le dispositif compressif sur la surface cutanée. Différents dispositifs de mesures in vivo ont été proposés : pneumatique et pneumatique-électrique ; piézoélectrique ; résistif ou à jauge de tension et capacitif avec une grande variabilité des techniques de mesure . Partsch et al. ont réalisé des mesures dans différentes positions et ont comparé une méthode in vitro et in vivo. Ils ont alors observé qu’il existait une corrélation correcte entre ces deux modes de mesure, d’où l’encouragement des techniques in vivo. Cependant, les pressions réelles in vivo exercées sur la peau par un bandage restent encore mal connues. De plus, la pression réellement exercée est opérateur-dépendante, c’est-à-dire que les pressions obtenues varient d’un opérateur à l’autre et, chez le même opérateur, d’une pose à l’autre .
Les dispositifs in vivo paraissent maintenant incontournables. Ils offrent de nouvelles perspectives et sont fortement encouragés par certains auteurs du fait de leur facilité d’utilisation et de leurs possibilités de mesure directe entre la peau et un article de compression. Dans ce contexte, cette étude a pour but de mesurer in vivo la pression d’interface de bandes de compression issues d’un fabricant dont les produits de compression représentent la très grande majorité des bandes élastiques délivrées en France, ayant des caractéristiques techniques différentes (élastique et non élastique, tension sous allongement à la pose, etc.), et selon différentes techniques de pose. L’objectif étant de les comparer entre elles et de vérifier les pressions réellement appliquées en fonction de ces différentes caractéristiques. L’influence de la position du sujet sera également évaluée en fonction des types de bandes utilisées.
La définition française des classes de compression a été choisie comme référence. On distingue ainsi 4 classes de compression d’après la norme réglementaire française (Afnor G30 102, 1986) : classe 1 : pression de 10 à 15 mmHg ; classe 2 : pression de 15,1 à 20 mmHg ; classe 3 : pression de 20,1 à 36 mmHg ; classe 4 : pression supérieure à 36 mmHg.
2.2
Méthodes
2.2.1
Sujets
Vingt sujets sains de sexe féminin ont accepté de participer à cette étude ( Tableau 1 ). Tous les sujets ont été soumis à un examen clinique préalable au sein du service de médecine physique et de réadaptation du CHU de Saint-Étienne, en vue de répondre aux critères d’inclusion suivants : sujet sain, de sexe féminin, nulligeste, âgé de 18 à 30 ans, volontaire, ayant un indice de masse corporel (IMC) normal (entre 18,5 et 25 kg/m 2 ) ; indemne de toute symptomatologie fonctionnelle vasculaire des membres inférieurs ; de toute affection neurologique, rhumatologique, cardio-vasculaire, respiratoire ou métabolique pouvant avoir une incidence sur le système vasculaire des membres inférieurs ou la mobilité ; de toute lésion traumatique ou de chirurgie des membres inférieurs ou de bassin ; de toute limitation fonctionnelle de déambulation et de possibilités de transfert couché-assis-debout.









