Conventional radiography is the primary imaging modality to evaluate the condition of hip resurfacing implants and the preferred method of assessing implant stability over time. Radiographs assess the angle of inclination of the femoral and acetabular components, implant stability, and femoral neck narrowing. Ultrasonography detects solid or soft tissue masses adjacent to the implant. Magnetic resonance imaging (MRI) detects osteolysis and complications in the periprosthetic soft tissues such as wear-induced synovitis, periprosthetic collections, neurovascular compression, and quality of the muscle and tendons of the rotator cuff of the hip. For pain after hip resurfacing, early use of optimized MRI is recommended.
Imaging of the painful surface replacement requires correlation between imaging and clinical data, including a comprehensive physical examination and careful patient history. The first mainstay of imaging evaluation is an appropriately performed radiograph to assess for radiographic findings that obviate more advanced imaging. In the setting of radiographs with equivocal or negative results, more advanced imaging may be necessary, and both magnetic resonance imaging (MRI) and ultrasonography have shown to be effective in the evaluation of these joints. Ultrasonography is helpful in detecting periprosthetic fluid collections, which may then undergo ultrasound-guided percutaneous aspiration. Computed tomography (CT) can detect osseous complications such as osteolysis and allow more accurate assessment of component alignment. Optimized MRI can not only identify fluid collections but also assess for any adverse synovial response that may indicate wear-induced synovitis or infection as well as identify periprosthetic osteolysis. Further modification of pulse sequences relevant to MRI is currently underway, resulting in marked improvement in the degree of artifacts generated by metal-on-metal (MOM) prostheses, allowing for superior characterization of the type of synovial reaction.
Radiographic assessment
Because of its widespread availability, conventional radiography continues to be the primary imaging modality to evaluate the condition of hip resurfacing implants. With the ability to visualize a large field of view, conventional radiographs are able to assess implant position relative to the native anatomy of the hip, thus allowing the measurement of femoral stem-shaft and cup abduction angles. Sequential radiographs remain the preferred method of assessing implant stability over time, such as loosening. With proper radiographic technique, one can assess a hip resurfacing implant for position, heterotopic bone formation, periprosthetic lucency, impingement, osteolysis, migration, and neck narrowing.
Technique
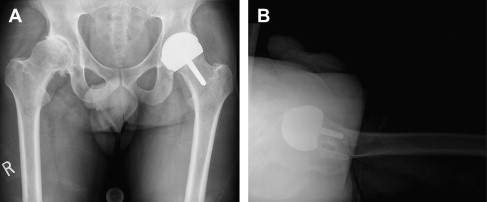
Conventional radiographs should be taken in 2 planes to allow for biplanar evaluation of the implant and surrounding bone. Most commonly, an anteroposterior view of the pelvis is taken in the frontal plane; visualization of both hips allows for a side-to-side comparison of the biomechanical axes of the hips. In the lateral plane, there is a wide variation in the preferred technique. At the authors’ institution, the preferred view is the cross-table (shoot-through or Johnson ) lateral view. This radiograph is taken with the patient supine and the nonoperated hip flexed to 90° so that it does not obstruct the field of view. The beam is aimed from the midline, and the cassette is positioned lateral to the hip. This type of imaging allows visualization of the lateral plane of the cup position and assessment of the amount of anteversion and the presence of anterior cup overhang. Studies have debated the accuracy of the cross-table lateral view with regard to anteversion because of the variability in native pelvic tilt, but this view still allows one to see the anterior aspect of the native acetabulum relative to the prosthetic edge ( Fig. 1 ) .
Interpretation
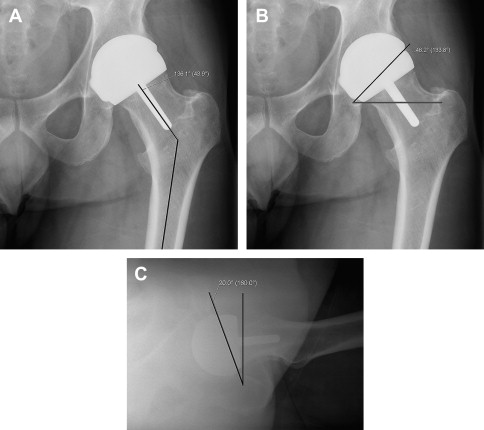
Femoral implant position
Conventional radiographs should be inspected for implant position. Commonly, the femoral stem-femoral shaft angle in both planes is of interest. This angle is assessed by measuring the angle created by a line drawn along the femoral stem and a line drawn down the femoral shaft ( Fig. 2 A). In the frontal plane, this angle typically approximates the native femoral neck-shaft angle of 135°, but several surgeons have advocated a more valgus orientation (higher stem-shaft angle) in order to improve the biomechanical forces on the neck. In the lateral plane, the angle created by the femoral stem and femoral shaft should approximate the native version of the femoral neck; however, the angle may be directed from more posterior to anterior to improve bone contact with the implant. Thus, there may be relative retroversion of the implant relative to the native femoral neck.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





