All patients presenting with signs and symptoms of lumbar radiculopathy must undergo a thorough history taking and physical examination. Often, however, the diagnosis remains unclear; it is accurate anatomically, but the underlying cause of the lesion is not confirmed, or the symptoms are so severe that more information on the anatomy is required. Therefore, the next step in the diagnostic process is imaging studies. This article discusses imaging modalities, including plain radiographs, magnetic resonance imaging, computed tomography (CT), CT myelogram, selective nerve root block, and bone scan.
All patients presenting with signs and symptoms of lumbar radiculopathy must undergo a thorough history taking and physical examination. After reviewing the dermatomal and myotomal patterns of the condition, astute clinicians often think that they are able to make the diagnosis. Often however, the diagnosis remains unclear; it is accurate anatomically, but the underlying cause of the lesion is not confirmed or the symptoms are so severe that more information on the anatomy is required. Finally, the patient may present with red flags that suggest that the cause of their condition is not benign. Therefore, often, the next step in the diagnostic process is to order imaging studies to attempt to confirm the suspected diagnosis or rule out more serious pathologic condition.
There are several imaging examinations that are used as an extension of history taking and physical examination, including plain radiographs, magnetic resonance imaging (MRI), computed tomography (CT), CT myelogram, selective nerve root block, and bone scan.
Plain radiographs
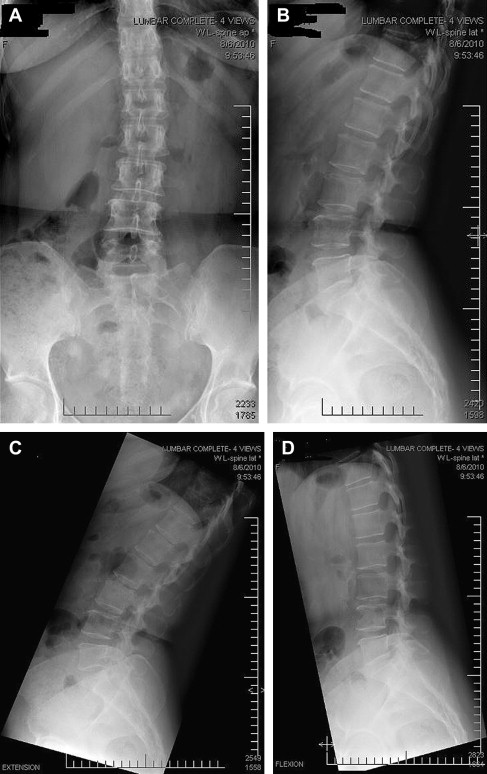
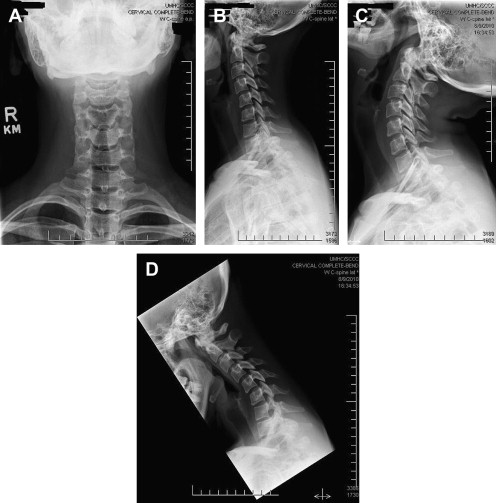
Plain radiographs of the spine usually consist of anteroposterior and lateral views. Specialized circumstances, such as the suspicion of spondylolysis, require oblique views. Inquires into alignment and instability requires dynamic flexion/extension motion views ( Figs. 1 and 2 ). Spine radiographs can also investigate whether the primary source of the spinal pain is related to malignancies, infections, instability, inflammatory spondyloarthropathies, and fractures (osteoporotic or pathologic) but with a lesser sensitivity than other imaging studies. Osteophyte formation from zygapophyseal joints or severe spondylolisthesis may raise concern about nerve root impingement, but this must be confirmed by more detailed imaging, such as CT scan or MRI.
Although many clinicians most often recommend radiographs as the first-line imaging study to investigate spinal pain, a lot has been written about the lack of effectiveness of radiographs to make relevant diagnoses. In 1987, the Quebec Task Force in proposed a classification to emphasize simple clinical criteria based on history taking (eg, location of symptoms, duration, and work status), physical examination findings, radiological test results, and response to treatment. This task force classified activity-related spinal disorders into 11 categories and subdivided these categories according to the working status during evaluation along with the duration of symptoms. For patients with radicular symptoms, the Quebec Task Force classification was highly associated with the severity of symptoms and the probability of subsequent surgical treatment. Nonsurgically treated patients in the Quebec Task Force classification categories reflecting nerve root compression had greater improvement than those with pain symptoms alone. Among surgical patients, the Quebec Task Force classification was not associated with outcome.
The most obvious shortcoming of radiograph is the lack of ability to see soft tissue structures such as spinal disks, nerves, muscles, or ligaments. Radiographs also lack fine detail of bony structures such as small osteophytes, canal size, lateral recess diameter, and end plate irregularities, which are seen better by CT or MRI. Finally, radiographs lack specificity when it comes to the abnormalities found as published studies have revealed that many asymptomatic volunteers had the same abnormities as patients with symptoms of spinal pain.
Despite the drawbacks, the routine of performing screening radiographs at the time of initial presentation or injury remains. Typically, more advanced imaging such as MRI, CT, or bone scan is not performed on initial presentation unless a red flag is identified for the severity of symptoms requiring such an inquiry. However, because many patients with spinal pain and radiculopathy do not respond with conservative management even after weeks of medical and rehabilitation treatments, more detailed imaging becomes necessary. MRI or CT is recommended earlier in patients with severe or progressive neurologic deficits or with serious underlying conditions, such as vertebral infection, cauda equina syndrome, or cancer with spinal cord compression.
MRI
MRI has become the most popular imaging modality for the investigation of spinal radiculopathy. Highly sensitive for disk, bone, and nerve abnormalities and lacking the radiation exposure of CT, MRI presents the most accurate information on the spine anatomy. MRI is the most sensitive imaging modality available to identify disk and soft tissue abnormalities in the spine. No imaging study can offer the visualization of the soft tissues in the spine such as disks, spinal nerves, and fat-related structures in as much detail ( Fig. 3 ). Sheehan indicates that the possible uses of MRI for low-back pain include predictive diagnostic assessment of severity, prognostic assessment of recovery, management planning, therapeutic planning, and occupational planning. Other studies, however, find the use of MRI to predict severity of symptoms or clinical outcomes to be unreliable because of the high sensitivity and low specificity of degenerative findings. For this reason, many national guidelines discourage the use of MRI in nonspecific low-back pain, although they do support its use to investigate for progressive neurologic symptoms to
- 1.
Exclude serious pathologic conditions, such as tumors or infections
- 2.
Correlate the level of abnormality to clinical symptoms of radiculopathy
- 3.
Plan surgical management of spinal stenosis and radiculopathy.
Adding gadolinium contrast can increase the sensitivity to identify malignant causes of spinal pain, such as infection, abscess, or malignant tumor. Fat suppression imaging can increase the sensitivity for identifying stress and insufficiency fractures and hyperintense signal within the spinal cord or plexus.
Both T1- and T2-weighted pulse sequences used together comprising sagittal and axial slices of the affected area of the spine offer the greatest view of the anatomy of the spine and associated neurologic structures to include or exclude abnormality. T1-weighted images, both in the sagittal and axial planes, are useful to evaluate epidural foraminal fat, whereas T2-weighted images are useful to evaluate neural structures, disk morphology, and facet joints. When clinically indicated, gadolinium-enhanced T1 sequences obtained both in the axial and sagittal planes are useful to differentiate between disk material (herniation of the nucleus pulposus) and granulation tissue of a previous surgery or surgeries.
The high sensitivity of MRI is not only its greatest achievement and advantage but also its greatest limitation. Jensen and colleagues found that on MRI examination of the lumbar spine, asymptomatic individuals without low-back pain can have disk bulges and protrusions. Jarvik and Deyo noted that extrusions are rare in asymptomatic patients. Therefore, it was concluded in the study that bulges and protrusions found on MRI in people with low-back pain or even radiculopathy may be coincidental. In summary, a patient’s clinical situation must be carefully evaluated in conjunction with the results of MRI ( Figs. 4–6 ). Other investigators have found similar findings of degenerative disks and annular tears in many asymptomatic individuals, reducing the specificity of these findings.
For the more advanced abnormalities, other investigators find a better specificity. Thornbury and colleagues demonstrated a sensitivity of MRI for small herniated disks of 89% to 100% but a specificity of only 43% to 57%. In a meta-analysis, Kent and colleagues demonstrated that the sensitivity of MRI for diagnosing high-grade stenosis ( Figs. 7 and 8 ) was 81% to 97% and the specificity ranged from 72% to 100%. When stricter criteria for false-positive findings were used, the specificity was 93% to 100%. In addition, other investigators have found a higher specificity for larger herniated disks, extruded disks, and sequestered disks, which are less often seen in asymptomatic patients.
MRI increases the nonspinal incidental findings, including renal cysts, liver cysts, thyroid nodules, and lymph node enlargement. All these conditions have the potential to be malignant, so they often require follow-up testing. But malignancy is extremely rare with these findings, thus the burden of cost and care is increased. Recently, higher-resolution scanners with 3.0 tesla and even stronger magnets have been introduced. It remains to be seen if this introduction results in a greater ability to find abnormality or an increase in incidental findings and reduced specificity ( Figs. 9–13 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





