Abstract
Osteoarthritis (OA) is a widely prevalent disease worldwide and, with an increasing ageing society, is a challenge for the field of physical and rehabilitation medicine. Technologic advances and implementation of sophisticated post-processing instruments and analytic strategies have resulted in imaging playing a more and more important role in understanding the disease process of OA. Radiography is still the most commonly used imaging modality for establishing an imaging-based diagnosis of OA. The need for an effective non-surgical OA treatment is highly desired, but despite on-going research efforts no disease-modifying OA drugs have been discovered or approved to date. MR imaging-based studies have revealed some of the limitations of radiography. The ability of MR to image all relevant joint tissues within the knee and to visualize cartilage morphology and composition has resulted in MRI playing a key role in understanding the natural history of the disease and in the search for new therapies. Our review will focus on the roles and limitations of radiography and MRI with particular attention to knee OA. The use of other modalities (e.g. ultrasound, nuclear medicine, computed tomography (CT), and CT/MR arthrography) in clinical practice and OA research will also be briefly described. Ultrasound may be useful to evaluate synovial pathology in osteoarthritis, particularly in the hand.
Knee osteoarthritis is a major public health problem that primarily affects the elderly. Almost 10% of the United States population suffers from symptomatic knee osteoarthritis by the age of 60 [S1] . In total, the health care expenditures of this condition have been estimated at US$ 186 billion annually [S2] . Despite this there are no approved interventions that ameliorate structural progression of this disorder.
The increasing importance of imaging in osteoarthritis for diagnosis, prognostication and follow-up is well recognized by both clinicians and osteoarthritis researchers. While conventional radiography is the gold standard imaging technique for the evaluation of known or suspected osteoarthritis in clinical practice and research, it has limitations that have become apparent in the course of large magnetic resonance imaging (MRI)-based knee osteoarthritis studies . Pathological changes may be evident in all structures of a joint with osteoarthritis although traditionally researchers have viewed articular cartilage as the central feature and as the primary target for intervention and measurement. Of the commonly employed imaging techniques, only MRI can assess all structures of the joint, including cartilage, meniscus, ligaments, muscle, subarticular bone marrow and synovium, and thus can show the knee as a whole organ three-dimensionally. In addition, it can directly help in the assessment of cartilage morphology and composition. The advantages and limitations of conventional radiography, MRI and other techniques such as ultrasound, nuclear medicine, computed tomography (CT) and CT arthrography in the imaging of osteoarthritis in both clinical practice and research are described in this review article.
1
Conventional radiography
Radiography is the simplest, least expensive and most commonly deployed imaging modality for OA. It enables detection of OA-associated bony features such as osteophytes, subchondral sclerosis and cysts . Radiography can also determine joint space width (JSW), which is a surrogate for cartilage thickness and meniscal integrity in knees, but direct visualization of these articular structures is not possible. Despite this limitation, slowing of radiographically detected joint space narrowing (JSN) remains the only structural end point currently approved by the U.S. Food and Drug Administration to demonstrate efficacy of disease-modifying OA drugs in phase III clinical trials. OA is radiographically defined by the presence of marginal osteophytes [S3] . Worsening of JSN is the most commonly used criterion for the assessment of structural OA progression and the total loss of JSW (“bone-on-bone” appearance) is one of the indicators for joint replacement.
We now know cartilage loss is not the only contributor to JSN but that changes in the meniscus such as meniscal extrusion and meniscal substance loss are also causative factors. The lack of sensitivity and specificity of radiography for the detection of OA-associated articular tissue damage, and its poor sensitivity to change longitudinally are other limitations of radiography. Changes in knee positioning can also be problematic in longitudinal studies and can affect the quantitative measurement of various radiographic parameters including JSW. Despite these limitations, radiography is still the gold standard for establishing an imaging-based diagnosis of OA and for assessment of structural modification in clinical trials of knee OA.
1.1
Semiquantitative assessments
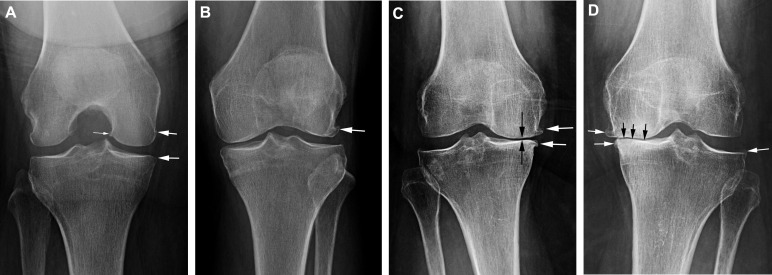
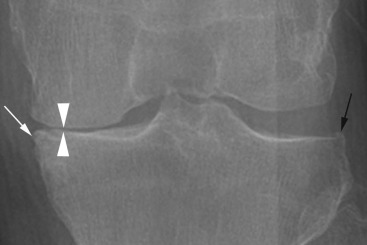
The severity of radiographic OA can be assessed with semiquantitative scoring systems. The Kellgren and Lawrence (KL) grading system is a widely accepted scheme for defining radiographic OA based on the presence of a definite osteophyte (grade 2). However, KL grading has its limitations; in particular, KL grade 3 includes all degrees of JSN, regardless of the actual extent. Fig. 1 depicts representative examples of the different KL grades as shown on the AP radiograph. Recently, the so-called atrophic phenotype of knee OA that is characterized by definite joint space narrowing without concomitant osteophyte formation has gained increasing attention as a potential risk factor for more rapid progressive OA, which may be considered a potential adverse event in so-called anti-nerve growth factor (NGF) drug trials, a class of new promising antianalgesic compounds currently under investigation . Although this phenotype is rare, it needs special attention in the research community as it potentially also is a reflection of more rapid disease progression . Fig. 2 shows an example of the atrophic phenotype of radiographic OA.
The Osteoarthritis Research Society International (OARSI) atlas provides image examples for grades for specific features of OA rather than assigning global scores according to definitions like the KL grading system. The atlas grades tibiofemoral JSW and osteophytes separately for each compartment of the knee (medial tibiofemoral, lateral tibiofemoral, and patellofemoral). A recent study using data from the OA Initiative and the OARSI atlas for semiquantitative grading of JSN demonstrated that centralized radiographic reading is important from the point of observer reliability, as even expert readers seem to apply different thresholds for JSN grading .
1.2
Quantitative assessments
JSW is the distance between the projected femoral and tibial margins on the anteroposterior radiographic image. Measurements may be performed manually or in a semi-automated fashion using computer software. Quantification using image processing software requires a digital image, whether digitized plain films or images acquired using fully digital modalities such as computed radiography and digital radiography. Minimum JSW is the standard metric, but the use of location-specific JSW has also been reported [S4] . Using software analysis of digital knee radiographic images, measures of location-specific JSW were shown to be comparable with MR imaging in detecting OA progression . Various degrees of responsiveness have been observed depending on the degree of OA severity, length of the follow-up period, and the knee positioning protocol [S4] . Measurements of JSW obtained from knee radiographs have been found to be reliable, especially when the study lasted longer than two years and when the radiographs were obtained with the knee in a standardized flexed position [S5] .
The role of malalignment in OA disease process has been described in the literature. A clinical trial showed that varus malalignment negated the slowing of structural progression of medial JSN by doxycycline [S6] . Valgus malalignment of the lower limb was shown to increase the risk of disease progression in knees with radiographic lateral knee OA . Malalignment might be a target for prevention of radiographic knee OA as determined by JSN in overweight and obese women .
2
Other radiography-based techniques
Interestingly, two older methods – tomosynthesis and bone texture analysis – have experienced a revival recently. Tomosynthesis generates an arbitrary number of cross-sectional images from a single pass of the X-ray tube. A recent study showed that tomosynthesis is more sensitive in the detection of osteophytes and subchondral cysts than radiography, using 3T MRI as the reference . Moreover, tomosynthesis was shown to offer excellent intrareader reliability regardless of the reader experience . Quantification of JSW using tomosynthesis has also been reported [S7] . Bone texture analysis extracts from conventional radiographs information on two-dimensional trabecular bone texture that relates directly to three-dimensional bone structure. It has been shown that bone texture may be a predictor of progression of tibiofemoral OA .
2
Other radiography-based techniques
Interestingly, two older methods – tomosynthesis and bone texture analysis – have experienced a revival recently. Tomosynthesis generates an arbitrary number of cross-sectional images from a single pass of the X-ray tube. A recent study showed that tomosynthesis is more sensitive in the detection of osteophytes and subchondral cysts than radiography, using 3T MRI as the reference . Moreover, tomosynthesis was shown to offer excellent intrareader reliability regardless of the reader experience . Quantification of JSW using tomosynthesis has also been reported [S7] . Bone texture analysis extracts from conventional radiographs information on two-dimensional trabecular bone texture that relates directly to three-dimensional bone structure. It has been shown that bone texture may be a predictor of progression of tibiofemoral OA .
3
MRI
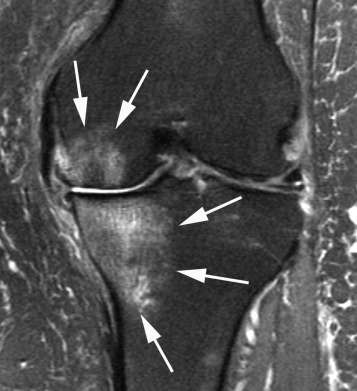
Because of the high cost, MRI is not routinely used in clinical management of OA patients. However, MRI has become a key-imaging tool for OA research thanks to its ability to assess pathology in structures not visualized by radiography i.e. articular cartilage, menisci, ligaments, synovium, capsular structures, fluid collections and bone marrow . With MRI the joint can be evaluated as a whole organ and multiple tissue changes can be monitored simultaneously; pathologic changes of pre-radiographic OA can be detected; and biochemical changes within joint tissues such as cartilage can be assessed before morphologic changes become evident. An MRI-based definition of OA is available . In addition, with MRI, OA can be classified into hypertrophic and atrophic phenotypes, according to the size of osteophytes and concomitant presence or absence of JSN . Importantly, the use of MRI has led to significant findings about the association of pain with bone marrow lesions and synovitis , with implications for future OA clinical trials. Fig. 3 shows an example of typical large bone marrow lesions that are commonly seen in conjunction with severe cartilage damage and may be responsible for pain in OA.
3.1
Technical considerations
It should be emphasized that investigators need to select appropriate MR pulse sequences for the purpose of each study. For example, focal cartilage defects and bone marrow lesions are best assessed using fluid-sensitive fast spin echo sequences (e.g. T2-weighted, proton density-weighted or intermediate-weighted) with fat suppression . Moreover, MRI may sometimes be affected by artifacts that mimic pathological findings. For example, susceptibility artifacts can be misinterpreted as cartilage loss or meniscal tear. Gradient recalled-echo sequences are known to be particularly prone to this type of artifact . To ascertain optimal assessment of MRI-derived data, trained musculoskeletal radiologists should be consulted when designing imaging-based OA studies or when interpreting data from the studies.
3.2
Semiquantitative MRI scoring systems for knee OA
A detailed review of semiquantitative MRI assessment of OA has been published . In addition to the three well-established scoring systems – the Whole Organ Magnetic Resonance Imaging Score (WORMS) , the Knee Osteoarthritis Scoring System (KOSS) [S8] , and the Boston Leeds Osteoarthritis Knee Score (BLOKS) [S9] – a new scoring system called the MR Imaging Osteoarthritis Knee Score (MOAKS) was most recently published. Of the three systems, WORMS and BLOKS have been widely disseminated and used, but these scoring systems both have strengths and weaknesses. MOAKS provides a refined scoring tool for cross-sectional and longitudinal semiquantitative MRI assessment of knee OA. It includes semiquantitative scoring of pathological features: bone marrow lesions; subchondral cysts; articular cartilage; osteophytes; Hoffa synovitis and synovitis-effusion; meniscus; tendons and ligaments; and periarticular features such as cysts and bursitides.
The use of within-grade changes for longitudinal assessment is commonly applied in OA research using semiquantitative MRI approaches . Within-grade scoring describes progression or improvement of a lesion that does not meet the criteria of a full grade change but does represent a definite visual change in comparison to the previous visit. A recent study demonstrated that within-grade changes in semiquantitative MRI assessment of cartilage and bone marrow lesions are valid and their use may increase the sensitivity of semiquantitative readings for detecting longitudinal changes in these structures .
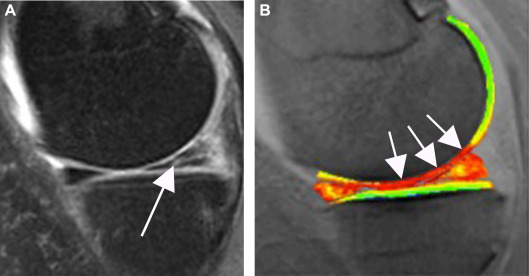
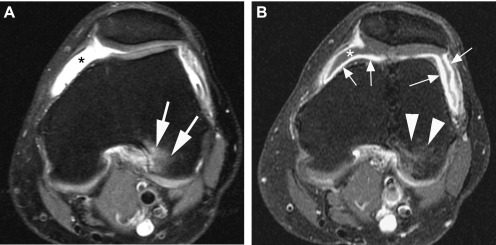
Synovitis is an important feature of OA and is associated with pain . Although synovitis can be evaluated with non-contrast-enhanced MR imaging by using the presence of signal changes in the Hoffa fat pad or joint effusion as an indirect marker of synovitis, only contrast-enhanced MR imaging can reveal the true extent of synovial inflammation . Scoring systems of synovitis based on contrast-enhanced MR imaging have been published , and these could potentially be used in clinical trials of new OA drugs that target synovitis. Fig. 4 shows a direct comparison between non-enhanced and contrast-enhanced MRI for the visualization of synovitis and joint effusion.
Other available semiquantitative MRI scoring systems related to knee OA include Cartilage Repair Osteoarthritis Knee Score (CROAKS) and Anterior Cruciate Ligament Osteoarthritis Score (ACLOAS) , which can be applied to research studies focusing on these structures. Specifically for imaging of cartilage repair tissue, MRI Observation Cartilage Repair Tissue (MOCART) scoring is available and has been applied to research studies involving cartilage repair surgery .
3.3
Semiquantitative MRI scoring system for hand OA
Radiography is still the modality of choice for assessment of hand OA in a clinical setting but the use of more sensitive imaging techniques such as ultrasound and MRI is becoming more common in OA research [S10] . A semiquantitative MRI scoring system for hand OA features called the OMERACT Hand Osteoarthritis Magnetic Resonance Scoring System (HOAMRIS) is available and offers high reliability and responsiveness [S11] . Scored pathological features include synovitis, erosions, cysts, osteophytes, JSN, malalignment and bone marrow lesions. Using these scoring systems, Haugen et al. showed that MRI could detect approximately twice as many joints with erosions and osteophytes as conventional radiography ( P < 0.001) and that moderate/severe synovitis, bone marrow lesions, erosions, attrition and osteophytes were associated with joint tenderness independently of each other . These studies demonstrated that some of the semiquantitatively assessed MRI features of hand OA may be potential targets for therapeutic interventions.
3.4
Semiquantitative MRI scoring system for hip OA
The hip joint has a spherical structure and its very thin covering of articular hyaline cartilage makes MRI assessment of the hip much more difficult than the knee. A whole organ semiquantitative multi-feature scoring system called the Hip Osteoarthritis MRI Scoring System (HOAMS) is available for use in observational studies and clinical trials of hip joints . In HOAMS, fourteen articular features are assessed: cartilage morphology, subchondral bone marrow lesions, subchondral cysts, osteophytes, acetabular labrum, synovitis (scored only when contrast-enhanced sequences are available), joint effusion, loose bodies, attrition, dysplasia, trochanteric bursitis/insertional tendonitis of the greater trochanter, labral hypertrophy, paralabral cysts and herniation pits at the supero-lateral femoral neck. HOAMS demonstrated satisfactory reliability and good agreement concerning intra- and inter-observer assessment. Recently another system was introduced that uses a similar approach . Direct comparisons of HOAMS and SHOMRI in regard to responsiveness and validity are missing to date.
3.5
Quantitative analysis of articular cartilage and other tissues
Quantitative measurement of cartilage morphology segments the cartilage image and exploits the three-dimensional nature of MRI data sets to evaluate tissue dimensions (such as thickness and volume) or signal as continuous variables. Examples of nomenclature for MRI-based cartilage measures and strategies for efficient analysis of longitudinal changes in subregional cartilage thickness were proposed by Eckstein et al. [S12] . Quantitative cartilage morphometry has been widely applied in OA studies [S13] . Quantitative measures of articular cartilage structure, such as cartilage thickness loss and denuded areas of subchondral bone have been shown to predict an important clinical outcome, i.e. knee replacement [S13] . Quantitative MRI analysis can also be applied to evaluate non-cartilage tissues in the joint including menisci [S14] , bone marrow lesions [S15] , synovitis [S16] and joint effusion [S17] . However, using segmentation approaches for ill-defined lesions such as bone marrow lesions is more challenging than segmentation of clearly delineated structures such as cartilage, menisci and effusion.
3.6
Compositional MRI
Compositional MRI allows visualization of the biochemical properties of different joint tissues. It may be sensitive to early, pre-morphologic changes that cannot be visualized on conventional MRI. Compositional MRI has been mostly applied for ultrastructural assessment of catilage, although the technique can also be used to assess other tissues such as the menisci or ligaments. Detailed reviews on this topic have been published recently . Compositional MRI of cartilage matrix changes can be performed using advanced MRI techniques such as delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), T1 rho, and T2 mapping [S18] . Of these, the first two take advantage of the concentration of highly negatively charged glycosaminoglycans (GAGs) in healthy hyaline cartilage; loss of these GAGs in focal areas affected by possible early disease can be visualized. Both dGEMRIC and T1 rho focus on charge density in cartilage. In contrast, T2 concentrations are affected by a complex combination of collagen orientation and hydration of cartilage.
Compositional MRI techniques are currently not routinely used in clinical practice and remain research tools that are available only at a limited number of institutions. Nevertheless, they have been applied in clinical trials and observational studies. A recent placebo-controlled double-blind pilot study of collagen hydrolysate for mild knee OA demonstrated that the dGEMRIC score increased (meaning higher GAG content and better cartilage status) in tibial cartilage regions of interest in patients receiving collagen hydrolysate, and decreased in the placebo group, with a significant difference being observed at 24 weeks . Crema et al. showed that a decrease in dGEMRIC indices was associated with an increase in cartilage thickness in the medial compartment of the knee, suggesting that an increase in cartilage thickness may also be related to a decrease in proteoglycan concentration . Souza et al. demonstrated that acute loading of the knee joint resulted in a significant decrease in T1 rho and T2 relaxation times of the medial tibiofemoral compartment and especially in cartilage regions with small focal defects, suggesting that changes of T1 rho values under mechanical loading may be related to the biomechanical and structural properties of cartilage. Hovis et al. reported that light exercise was associated with low cartilage T2 values but moderate and strenuous exercise was associated with high T2 values in women, suggesting that activity levels can affect cartilage composition . In an interventional study assessing the effect of weight loss on articular cartilage, Anandacoomarasamy et al. reported that improved articular cartilage quality was reflected as an increase in the dGEMRIC index over one year for the medial but not the lateral compartment , highlighting the role of weight loss in possible clinical and structural improvement. Fig. 5 shows an example of a knee with a prevalent meniscal tear and corresponding decrease in GAG content in the central aspect of the cartilage of the central medial femoral condyle.