Humeral Resurfacing: Indications, Technique, and Results
Kirk Jensen
OVERVIEW
Humeral articular cartilage can be damaged in a variety of ways: global loss secondary to inflammatory, infectious, osteoarthritic, posttraumatic, or iatrogenic causes and focal loss such as localized avascular necrosis (AVN), traumatic, or postsurgical defects. These cartilage injuries occur in a spectrum of patients, all with their own clinical presentation, from an older osteoporotic sedentary patient to the younger, active patient with excellent bone quality. Humeral head resurfacing arthroplasty has evolved from a fringe treatment option into a reliable method of shoulder arthroplasty designed to restore the natural anatomy of an arthritic or damaged articular humeral surface.22
Recent implant changes have improved the ability of the surface replacement implants to recreate the humeral head surface and improve the initial implant fixation. Resurfacing implants now have surface extensions for rotator cuff deficiencies and increased size options. The development of a smaller resurfacing implant now allows for the partial resurfacing of smaller asymmetric focal cartilage lesions of the humeral head.21,24 Instrument changes have improved the ability to place the implant in the anatomic position that recreates an individual’s humeral articular surface posterior offset, neck-shaft angle, and version. These implant and instrument changes have led to more refined surgical technique that avoid the complications associated with the use of stemmed implants. Minimal bone resection occurs in shoulder resurfacing arthroplasty; therefore, preserving bone stock is important in active or young patients with shoulder arthritis. Cementless surface replacements have been shown to provide results that are comparable to those of stemmed implants with similar diagnosis and follow-up.1,7,14,15 and 16,23 The following text outlines the current rationale and indications for the usage of resurfacing arthroplasty implants; the surgical techniques are also presented, along with a review of the results of proximal humerus resurfacing arthroplasty. The natural progression from resurfacing arthroplasty to the development of new “stemless” humeral head arthroplasty will also be reviewed.
HUMERAL HEAD RESURFACING ARTHROPLASTY
The concept of resurfacing arthroplasty as a treatment for painful humeral head articular cartilage conditions evolved from its application in arthritic hip joints. The first-generation humeral resurfacing arthroplasty implants were based upon the extensive historic experience with hip resurfacing arthroplasty, were made from stainless steel, and lacked a central stem, relying on methylmethacrylate for fixation.
Copeland has contributed greatly to the development of future implant resurfacing designs. In 1986, he developed the Mark I prosthesis, a cementless resurfacing component with a smooth central round stem and a screw that engaged the lateral cortex of the proximal humerus for immediate fixation and to control rotation. The screw was felt to be unnecessary
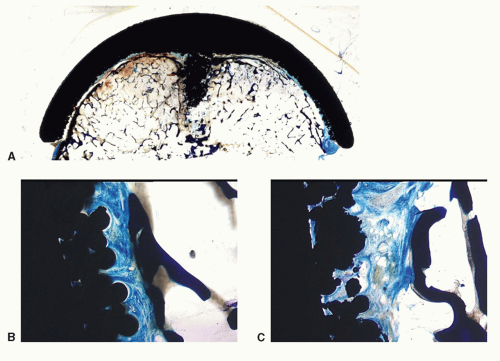
and the Mark II design was implanted from 1990 to 1993. The Mark III resurfacing design that began clinical implantation in 1993 added an application of hydroxyapatite coating to the entire undersurface and central stem to improve immediate and long-term component fixation.12 Third-generation implants have been designed since 2002, with anatomic head sizing based upon the observation that the humeral head height correlates with the humeral head diameter.4,11 An increase in the sizing options and radius of circumference changes in the available resurfacing implants implies greater anatomic options for the patients. The third-generation implants also achieve improved theoretical fixation at the time of implantation with unique undersurface designs and stem designs that provide immediate rotational stability. Theoretically, long-term fixation of the third-generation implants have been improved by the addition of hydroxyapatite or alternative finishes, such as porous coating (Fig. 15-1) or grit blasting on the undersurface of the head and the proximal portion of the stem, as well as the presence of apical flat surfaces on the undersurface that provides an area of increased contact (Fig. 15-1A).
and the Mark II design was implanted from 1990 to 1993. The Mark III resurfacing design that began clinical implantation in 1993 added an application of hydroxyapatite coating to the entire undersurface and central stem to improve immediate and long-term component fixation.12 Third-generation implants have been designed since 2002, with anatomic head sizing based upon the observation that the humeral head height correlates with the humeral head diameter.4,11 An increase in the sizing options and radius of circumference changes in the available resurfacing implants implies greater anatomic options for the patients. The third-generation implants also achieve improved theoretical fixation at the time of implantation with unique undersurface designs and stem designs that provide immediate rotational stability. Theoretically, long-term fixation of the third-generation implants have been improved by the addition of hydroxyapatite or alternative finishes, such as porous coating (Fig. 15-1) or grit blasting on the undersurface of the head and the proximal portion of the stem, as well as the presence of apical flat surfaces on the undersurface that provides an area of increased contact (Fig. 15-1A).
The rationale for the use of humeral resurfacing arthroplasty includes the preservation of humeral bone stock and a decrease in intraoperative occurrences such as humeral peri-prosthetic fracture and excessive blood loss. In the case of implant failure or the development of glenoid arthrosis and the need for revision, a humeral resurfacing arthroplasty does not require removal of a cemented or ingrowth stem, and therefore, avoids humeral shaft fracture and catastrophic loss of humeral bone. Also, the conversion to standard stemmed arthroplasty and the placement of a glenoid component does not require specialized equipment or technique.15 Arthrodesis as a salvage procedure may also be performed due to preserved metaphyseal bone.
Accurate intraoperative articular surface positioning is also reliably obtained due to the absence of an intramedullary-based system. Systematic anatomic investigation of proximal humerus anatomy has revealed that normal anatomy values, such as retroversion, head shaft angle, center of rotation, are variable from individual to individual.3,4,11,20 These individual variations are difficult for an intramedullary-based system to encompass, and the biomechanical studies of several intramedullary-based humeral head replacement systems have shown that the replication of the normal articular surface cannot be achieved with these systems and that they displace the center of rotation superiorly and laterally potentially causing late complications.3,19 However, neck-shaft angle and retroversion can be easily managed by a resurfacing arthroplasty by identifying the humeral anatomic neck and center of the humeral head at the time of surgery. Therefore, resurfacing arthroplasty of the humeral head provides a reliable technique to anatomically recreate a stable articulating surface regardless of individual pathologic anatomy.22
INDICATIONS
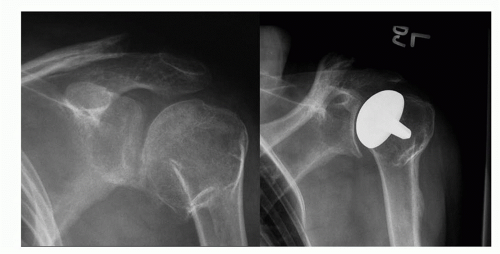
Historically, humeral resurfacing arthroplasty was indicated for younger, active patients with osteoarthritis and a concentric glenoid and for patients with metaphyseal dysplasia, rheumatoid arthritis, or those with AVN who had adequate supportive bone (Fig. 15-2). Currently, these indications have been expanded to include instability arthritis with a concentric glenoid or resurfaced glenoid, arthroscopy arthropathy, posttraumatic arthritis or arthritis associated with a proximal humerus malunion (Figs. 15-3 and 15-4), cuff tear arthropathy with stable kinematics, and dialysis arthropathy. Numeric patient age is not relevant; however, the quality of proximal humerus is a significant factor and the subchondral surface should support at least 60% of the resurfacing implant.14,15 and 16 A humeral resurfacing arthroplasty requires anterior glenoid-implant stability provided by the function of an intact subscapularis tendon or pectoralis major transfer. A resurfacing arthroplasty may be performed in the presence of large rotator cuff tears if stable kinematics are present.7 The resurfacing arthroplasty functions as a hemiarthroplasty and therefore a congruent glenoid surface is also a requirement. Glenoid surface abnormalities such as
eccentric wear, cystic bone changes, or rim deficiencies should be managed appropriately to produce a stable congruent surface for the resurfacing implant to articulate against. However, glenoid resurfacing with an implant may be problematic due to limited exposure in a stiff shoulder joint and should be a consideration in any preoperative decision-making.
eccentric wear, cystic bone changes, or rim deficiencies should be managed appropriately to produce a stable congruent surface for the resurfacing implant to articulate against. However, glenoid resurfacing with an implant may be problematic due to limited exposure in a stiff shoulder joint and should be a consideration in any preoperative decision-making.
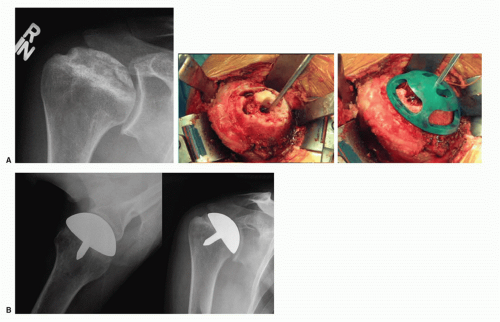 FIGURE 15-2. (A, B) A 55-year-old male with AVN from use of oral steroid treated with a CAP hemiarthroplasty. (Courtesy of Joseph Iannotti, MD, PhD.) |
SURGICAL TECHNIQUE
Preoperative templating of a 30-degree external rotation anteroposterior (AP) radiograph allows the surgeon to estimate the implant size that will be needed during surgery. Both the head diameter and the height can be estimated at this time, as well as identifying the presence of degenerative anatomic humeral head changes that may influence intraoperative implant positioning or sizing. The head size will be verified intraoperatively by measuring the humeral head after peripheral osteophyte removal. An axillary lateral radiograph or a CT scan is also required preoperatively to identify nonconcentric glenoid wear.
We prefer proximal humerus resurfacing to be performed with the patient anesthetized with both general anesthesia and regional anesthesia. The patient should receive preoperative intravenous antibiotics ½ hour prior to induction of anesthesia. The patient should be placed in a supine beach chair position with the head elevated 30 degrees and lateral enough to allow the surgical arm to be fully extended. Two different approaches are commonly utilized depending on the surgeon’s preference, a superior approach (MacKenzie approach)18 or a deltopectoral approach. The Mackenzie approach utilizes a smaller incision, direct access to the glenoid through the rotator interval, and excellent exposure to the superior and posterior rotator cuff for reconstruction. The major disadvantage of the approach is the detachment of the anterior deltoid origin and inherent potential issues with reattachment. The deltopectoral approach has been well described and has the advantage of preserving the deltoid origin, is extensile, and facilitates subscapularis lengthening.17 The method of subscapularis release and repair is dependent on the degree of external rotation loss and may consist of an intratendinous incision and anatomic repair, a release of the subscapularis from the lesser tuberosity with a subperiosteal incision, a z-lengthening of the subscapularis and anterior capsule, or a lesser tuberosity osteotomy. It is recommended that the anterior-inferior capsule be excised medial to its
lateral confluence with the subscapularis tendon. To achieve this safely, the axillary nerve must be identified and protected.
lateral confluence with the subscapularis tendon. To achieve this safely, the axillary nerve must be identified and protected.
 FIGURE 15-4. A 56-year-old male with posttraumatic arthritis and malunion treated with a CAP hemiarthroplasty. (Courtesy of Joseph Iannotti, MD, PhD.) |
After the subscapularis and anterior-inferior capsule have been released, the humeral head is delivered out of the wound using simultaneous adduction, external rotation, and extension of the arm. This requires a complete inferior capsular release from the humeral neck to its posterior inferior attachment. With the humeral head delivered out of the wound, remove all humeral osteophytes. This is a particularly important step, since the anatomic neck must be visualized to guide humeral preparation and to determine the neck-shaft angle of the patient. Place a curved Crego or reverse Hohmann retractor along the anatomic neck superiorly to protect and retract the long head of the biceps and posterosuperior rotator cuff. The biceps tendon may be tenodesed at this time distally at its natural resting length. Identify and mark the anatomic neck with electrocautery or marking pen.
Head sizing is performed preoperatively with templating and confirmed intraoperatively using the humeral head sizer or humeral head gauge. Place the preoperatively determined sizer over the humeral articular surface such that its superior rim is parallel to the superior articular cartilage line and the plane of the head sizer rim is parallel to the plane of the anatomic neck of the native humerus (Fig. 15-5). The appropriate head sizer is determined by identifying the articular margin of the humerus in relation to the inferior edge of the sizer, as the inferior edge of the sizer represents the outermost diameter of the definitive implant. A common problem with humeral resurfacing is incomplete reaming and placement of the correct sized component in medialized position resulting in lateralization of the center of rotation of the humeral head (Fig. 15-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree