Hip resurfacing arthroplasty has reemerged as a valid reconstruction option for the osteoarthritic hip. Patient selection is critical for excellent surgical outcomes, especially when compared with total hip arthroplasty. However, concerns regarding surgical technique and postsurgical complications persist. The authors review the evidence for surgical technique, outcomes, and complications related to modern metal-on-metal hip resurfacing arthroplasty.
Many patients seek hip arthroplasty earlier in life to remain physically active rather than accept the limitations of their hip arthritis. This younger patient demographic will likely require additional hip surgery because the life expectancy of patients in their 40s and 50s will most likely exceed 30 more years. As a result, the lack of established longevity for standard bearing (metal-on-polyethylene) total hip arthroplasty (THA) and the need for future revision of THA in this younger patient population has prompted the use of alternative bearing surfaces and fueled the resurgence of hip resurfacing arthroplasty.
The first hip resurfacing procedures (large metal head articulating with high-molecular-weight polyethylene) performed in the 1970s resulted in an unacceptably high wear rate resulting in failure secondary to osteolysis (ie, aseptic loosening or inflammatory bone resorption). Despite this initial failure, efforts have been made to improve surgical technique, instrumentation, and implant design.At present, there are several hip resurfacing implant systems available; however, only the Cormet (Corin, England) and Birmingham hip resurfacing systems (Smith and Nephew, Memphis, TN, USA) are approved by the Food and Drug Administration for use in the United States.
Modern implant design
Current hip resurfacing implants use a metal-on-metal bearing surface, with implants forged or cast from high-carbon cobalt-chromium-molybdenum alloy. If the femoral and acetabular implants are well-manufactured and well-positioned, large-diameter metal-on-metal bearing surfaces are predicted by lubrication theory to produce very low levels of volumetric wear compared with the metal-on-polyethylene surfaces used in the past.
Hybrid fixation (press-fit acetabular and cemented femoral components) is most commonly used. A cementless acetabular cup is typically press fit into the under-reamed acetabulum. The acetabular cup has a surface modification of cobalt-chromium beads or plasma-sprayed titanium with or without hydroxyapatite coating for bone in-growth and fixation. The femoral component is traditionally cemented into place on the femoral neck. There are, however, cementless designs being used because of the potential for thermal bone necrosis during the cement curing process, contributing to early implant failure.
Surgical technique
There is no ideal surgical approach for hip resurfacing arthroplasty. There is a balance between the risks of surgical dissection and necessary exposure and visualization. Femoral head oxygen concentration is compromised in both the anterolateral and posterior approaches. However, during the anterolateral approach and not the posterior approach, femoral oxygen concentration recovers after implantation with hip relocation ( Table 1 ), suggesting compromise of the ascending branch of the medial circumflex femoral artery during release of the short external rotators during the posterior approach. However, a posterior approach used in surgical dislocation that protects the tendon of the obturator externus and consequently the ascending branch of the medial circumflex femoral artery has no risk of femoral head osteonecrosis (see Table 1 ). Retrieval studies demonstrated osteonecrosis of the remaining femoral head in 10 of 14 failed hip resurfacing arthroplasties using the posterior approach; 9 underwent revision for femoral neck fracture, and 1 underwent revision for femoral component loosening.
| Technical Considerations | Evidence | Citations |
|---|---|---|
| The anterolateral approach preserves the blood supply to the femoral head | Level III, B | |
| The extended posterior approach compromises the blood supply to the femoral head | Level IV, B | |
| An obturator externus tendon sparing posterior approach does not compromise the blood supply to the femoral head | Level IV, B | |
| Reaming of the femoral head decreases blood supply to the femoral head | Level IV, B | |
| Femoral neck notching decreases blood supply to the femoral head and is associated with femoral implant loosening | Level IV, B | |
| A cement mantle more than 3 mm is associated with femoral implant loosening | Level IV, B | |
| Filling of bone cysts greater than 1 cm 3 is associated with femoral implant loosening | Level IV, B | |
| Lesser trochanteric suction cannula can control femoral temperatures during cementing | Level III, B | |
| A varus stem-shaft angle less than 130° correlates with adverse outcome | Level III, B | |
| Hip resurfacing arthroplasty cannot dramatically affect limb length or horizontal femoral offset | Level III, B | |
| Biomechanical reconstruction of the hip is comparable to THA with hip resurfacing arthroplasty if minimal initial deformity is present | Level I, A | |
| Acetabular bone loss is similar to that of THA | Level I, A | |
| Acetabular component abduction angle of greater than 55° can increase wear | Level IV, B | |
| Femoral bone stock is preserved and may be converted to THA | Level II, B |
Preparation of the femoral head by reaming is enough to decrease blood flow to the femoral head by 70% in 9 of 10 hips. This is likely a result of disruption of the nutrient retinacular vessels of the femoral head because 80% of these vessels penetrate bone in the anterosuperior and posterosuperior quadrants of the femoral neck. Valgus positioning during reaming results in notching of the femoral neck and a reduction of blood flow by 50% in 10 of 14 hips by laser Doppler flowmetry (see Table 1 ). Notching is associated with an increase in femoral component loosening, from 6.8% to 28.6%, during radiographic follow-up of 72 hip resurfacing arthroplasties (see Table 1 ). Removal of up to 30% of the anterolateral femoral neck does not alter the load-bearing capacity of the proximal femur, suggesting that there is minimal mechanical weakness attributed to femoral neck notching and that there is a vascular component to femoral neck notching that contributes to loosening as opposed to fracture.
The heat produced by polymerization of the cement that is used to fix the femoral component may result in thermal bone necrosis. Retrieval studies of 96 failed hip resurfacing arthroplasties demonstrate that femoral implants that failed secondary to femoral loosening had an average cement mantle of 2.9 mm, whereas nonfemoral failures had an average cement mantel of 2.3 mm. In addition, the bone-cement interface of the loose femoral components were thick, fibrous, and associated with bone resorption, and the interface of those isolated for femoral neck fracture were ischemic. Cement-filled bone cysts were more prevalent in hip resurfacing arthroplasties that failed secondary to femoral loosening. Finite element modeling supports the concept that deep cement penetration or filling of a bone cyst larger than 1 cm 3 results in temperatures that are consistent with thermal bone necrosis (see Table 1 ). Another retrieval study that evaluated 55 failed hip resurfacings supports these conclusions. Use of a 3-mm suction cannula inserted into a hole drilled in the lesser trochanter, penetrating 3 cm into the intramedullary canal for femoral preparation and cementing, resulted in a decrease in the maximal femoral temperature from 68°C to 36°C, well below the level required for thermal bone necrosis (see Table 1 ).
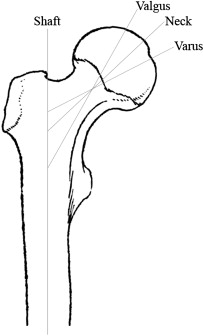
The positioning of the femoral component is critical. Evaluation of 94 hip resurfacing arthroplasties showed that a varus stem-shaft angle, less than 133°, correlated with adverse outcomes (see Table 1 ). Finite element analysis supports placement of the femoral implant in a relative valgus position as a result of decreased predicted peak stress levels more similar to those of a normally loaded femur ( Fig. 1 ). Valgus positioning by 10° increased load to fracture by 28%. However, radiographic studies demonstrate that placement of the femoral component in 5° to 10° of relative valgus position slightly decreases mean femoral offset by 4.5 to 8 mm and results in mean limb length discrepancy of −2.2 to 0.3 mm (see Table 1 ). Hence, hip resurfacing arthroplasty can only minimally alter hip biomechanics to correct deformity. Despite this limitation, a randomized clinical trial of 120 patients comparing THA to hip resurfacing arthroplasty confirmed a mean limb shortening of 1.9 mm and a mean reduction in horizontal offset by 3.3 mm in the hip resurfacing arthroplasty limb of the study (see Table 1 ).
Despite issues with exposure, reaming, and cementing, the modern metal-on-metal hybrid hip resurfacing implants provide the bone stock conservation required for the implant to be viable in a younger patient population (see Table 1 ). Many acetabular components require the removal of less than 5 mm of acetabular bone stock, similar to the amount of acetabular bone stock removed during a THA. A randomized trial of 230 hips demonstrated no difference in the size of the acetabular component in hip resurfacing arthroplasty or THA. Positioning of the acetabular component is also important because an abduction angle (ie, lateral opening angle) of greater than 55° has been shown to increase wear in simulation and retrieval studies.
The conservation of bone stock on the femoral side is intuitive because a hip resurfacing arthroplasty can easily be converted to a THA in the case of complication or need for revision. There is no demonstrated loss of bone mineral density secondary to stress shielding during hip resurfacing arthroplasty in comparative studies. However, there is a 70% incidence of femoral neck narrowing seen during retrospective review of 163 hip resurfacing arthoplasties. The consequence of this finding is unknown.
Surgical technique
There is no ideal surgical approach for hip resurfacing arthroplasty. There is a balance between the risks of surgical dissection and necessary exposure and visualization. Femoral head oxygen concentration is compromised in both the anterolateral and posterior approaches. However, during the anterolateral approach and not the posterior approach, femoral oxygen concentration recovers after implantation with hip relocation ( Table 1 ), suggesting compromise of the ascending branch of the medial circumflex femoral artery during release of the short external rotators during the posterior approach. However, a posterior approach used in surgical dislocation that protects the tendon of the obturator externus and consequently the ascending branch of the medial circumflex femoral artery has no risk of femoral head osteonecrosis (see Table 1 ). Retrieval studies demonstrated osteonecrosis of the remaining femoral head in 10 of 14 failed hip resurfacing arthroplasties using the posterior approach; 9 underwent revision for femoral neck fracture, and 1 underwent revision for femoral component loosening.
| Technical Considerations | Evidence | Citations |
|---|---|---|
| The anterolateral approach preserves the blood supply to the femoral head | Level III, B | |
| The extended posterior approach compromises the blood supply to the femoral head | Level IV, B | |
| An obturator externus tendon sparing posterior approach does not compromise the blood supply to the femoral head | Level IV, B | |
| Reaming of the femoral head decreases blood supply to the femoral head | Level IV, B | |
| Femoral neck notching decreases blood supply to the femoral head and is associated with femoral implant loosening | Level IV, B | |
| A cement mantle more than 3 mm is associated with femoral implant loosening | Level IV, B | |
| Filling of bone cysts greater than 1 cm 3 is associated with femoral implant loosening | Level IV, B | |
| Lesser trochanteric suction cannula can control femoral temperatures during cementing | Level III, B | |
| A varus stem-shaft angle less than 130° correlates with adverse outcome | Level III, B | |
| Hip resurfacing arthroplasty cannot dramatically affect limb length or horizontal femoral offset | Level III, B | |
| Biomechanical reconstruction of the hip is comparable to THA with hip resurfacing arthroplasty if minimal initial deformity is present | Level I, A | |
| Acetabular bone loss is similar to that of THA | Level I, A | |
| Acetabular component abduction angle of greater than 55° can increase wear | Level IV, B | |
| Femoral bone stock is preserved and may be converted to THA | Level II, B |
Preparation of the femoral head by reaming is enough to decrease blood flow to the femoral head by 70% in 9 of 10 hips. This is likely a result of disruption of the nutrient retinacular vessels of the femoral head because 80% of these vessels penetrate bone in the anterosuperior and posterosuperior quadrants of the femoral neck. Valgus positioning during reaming results in notching of the femoral neck and a reduction of blood flow by 50% in 10 of 14 hips by laser Doppler flowmetry (see Table 1 ). Notching is associated with an increase in femoral component loosening, from 6.8% to 28.6%, during radiographic follow-up of 72 hip resurfacing arthroplasties (see Table 1 ). Removal of up to 30% of the anterolateral femoral neck does not alter the load-bearing capacity of the proximal femur, suggesting that there is minimal mechanical weakness attributed to femoral neck notching and that there is a vascular component to femoral neck notching that contributes to loosening as opposed to fracture.
The heat produced by polymerization of the cement that is used to fix the femoral component may result in thermal bone necrosis. Retrieval studies of 96 failed hip resurfacing arthroplasties demonstrate that femoral implants that failed secondary to femoral loosening had an average cement mantle of 2.9 mm, whereas nonfemoral failures had an average cement mantel of 2.3 mm. In addition, the bone-cement interface of the loose femoral components were thick, fibrous, and associated with bone resorption, and the interface of those isolated for femoral neck fracture were ischemic. Cement-filled bone cysts were more prevalent in hip resurfacing arthroplasties that failed secondary to femoral loosening. Finite element modeling supports the concept that deep cement penetration or filling of a bone cyst larger than 1 cm 3 results in temperatures that are consistent with thermal bone necrosis (see Table 1 ). Another retrieval study that evaluated 55 failed hip resurfacings supports these conclusions. Use of a 3-mm suction cannula inserted into a hole drilled in the lesser trochanter, penetrating 3 cm into the intramedullary canal for femoral preparation and cementing, resulted in a decrease in the maximal femoral temperature from 68°C to 36°C, well below the level required for thermal bone necrosis (see Table 1 ).
The positioning of the femoral component is critical. Evaluation of 94 hip resurfacing arthroplasties showed that a varus stem-shaft angle, less than 133°, correlated with adverse outcomes (see Table 1 ). Finite element analysis supports placement of the femoral implant in a relative valgus position as a result of decreased predicted peak stress levels more similar to those of a normally loaded femur ( Fig. 1 ). Valgus positioning by 10° increased load to fracture by 28%. However, radiographic studies demonstrate that placement of the femoral component in 5° to 10° of relative valgus position slightly decreases mean femoral offset by 4.5 to 8 mm and results in mean limb length discrepancy of −2.2 to 0.3 mm (see Table 1 ). Hence, hip resurfacing arthroplasty can only minimally alter hip biomechanics to correct deformity. Despite this limitation, a randomized clinical trial of 120 patients comparing THA to hip resurfacing arthroplasty confirmed a mean limb shortening of 1.9 mm and a mean reduction in horizontal offset by 3.3 mm in the hip resurfacing arthroplasty limb of the study (see Table 1 ).
Despite issues with exposure, reaming, and cementing, the modern metal-on-metal hybrid hip resurfacing implants provide the bone stock conservation required for the implant to be viable in a younger patient population (see Table 1 ). Many acetabular components require the removal of less than 5 mm of acetabular bone stock, similar to the amount of acetabular bone stock removed during a THA. A randomized trial of 230 hips demonstrated no difference in the size of the acetabular component in hip resurfacing arthroplasty or THA. Positioning of the acetabular component is also important because an abduction angle (ie, lateral opening angle) of greater than 55° has been shown to increase wear in simulation and retrieval studies.
The conservation of bone stock on the femoral side is intuitive because a hip resurfacing arthroplasty can easily be converted to a THA in the case of complication or need for revision. There is no demonstrated loss of bone mineral density secondary to stress shielding during hip resurfacing arthroplasty in comparative studies. However, there is a 70% incidence of femoral neck narrowing seen during retrospective review of 163 hip resurfacing arthoplasties. The consequence of this finding is unknown.
Modern hip resurfacing arthroplasty outcomes
Hip resurfacing arthroplasty has been shown to be equivalent to THA in short- to medium-term retrospective studies ( Table 2 ). Comparison of 52 hip resurfacing arthroplasties with 93 cementless THAs after a mean follow-up of 3 years revealed similar revision rates of 3.5% and 4.3%, respectively. In addition, the complication rate and improvements in function, range of motion, and pain were also similar. The 5-year mean follow-up data on age, gender, body mass index, and activity level were also similar between hip resurfacing arthroplasty and hybrid THA, with 6% and 8% revision rates, respectively, and with similarly excellent quality of life and functional scores. The Australian Orthopaedic Association National Joint Replacement Registry supports these findings. Men younger than 65 years with hip resurfacing arthroplasty have a similar revision rate to those with THA. The revision rate of hip resurfacing arthroplasty is 2% at 5 years. Harris Hip Scores are equivalent at 2 years in retrospective comparison of 337 hip resurfacing arthroplasties and 266 THAs. Gait is also shown to be similar between patients who underwent hip resurfacing arthroplasty and those who underwent THA, with the former group walking at almost a normal speed of 1.26 m/s. A prospective, randomized, controlled trial comparing 48 patients demonstrated no difference in gait speed or postural balance. In fact, both groups had reached normal parameters at 3 months post surgery. There are several unpublished reports and trials showing that range of motion after hip resurfacing arthroplasty is full in all planes of motion, but retrospective data show an almost 20° increase in hip flexion after surgery to greater than 110°. A retrospective study supports the concept that early hip resurfacing arthroplasty results in an improved functional outcome (see Table 2 ). Hips with fewer changes secondary to osteoarthritis (ie, bone density, femoral neck shape, hip biomechanics, and focal bone defects) correlated with improved postoperative hip pain, range of motion, and biomechanics and fewer acetabular radiolucencies.
| Patient Selection and Outcome | Evidence | Citations |
|---|---|---|
| Hip resurfacing arthroplasty survivorship at 3 and 5 years is equivalent to THA | Level II, B | |
| 0.02% revision rate in men younger than 55 years with osteoarthritis | Level IV, B | |
| 3% revision rate if SARI a ≤3; 11% revision rate if SARI>3 | Level IV, B | |
| Patients return to a high level of function, including sports, after hip resurfacing arthroplasty | Level I, A | |
| Gait speed and postural balance are similar to THA and normal at 3 months postsurgery | Level I, A | |
| Hip flexion increases by 20° after hip resurfacing arthroplasty | Level IV, B | |
| Early intervention favors a good functional outcome | Level II, B | |
| Patients with osteonecrosis of the femoral head have an increased revision rate of 7% | Level II, B |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



