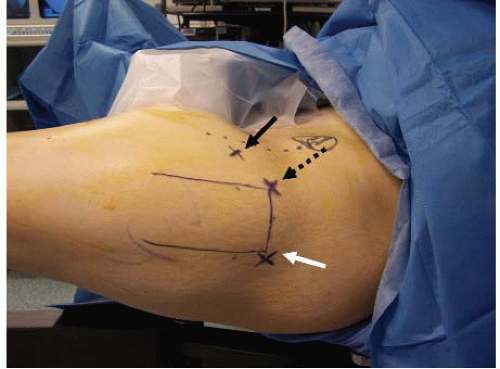
improvements assessed at the completion of the procedure. The patient is then moved distally on the table until contact is made between the medial thigh of the operative leg and the perineal post. The peroneal post should be adequately padded to decrease the risk for local neural and cutaneous injuries. The feet are placed in a well-padded boot or wrapped in cast padding after applying an ABD pad to the dorsomedial aspect of the forefoot. Padding protects the foot from skin and nerve pressure injuries as the feet need to be secure to avoid inadvertent slippage and loss of traction during the case. The feet are placed in the traction boots and further secured with cloth tape. The nonoperative leg is then maximally abducted and externally rotated with the knee in extension. The operative leg is positioned in neutral abduction, neutral to 15° of hip flexion, maximal internal rotation, and full knee extension. The pelvis is leveled by rotating the bed (typically toward the operative side) until the anterior superior iliac spines (ASIS) are at the same height and parallel to the floor/ceiling. A mayo stand is brought in from the contralateral side of the patient and placed over the upper torso and head. This acts as a working platform where instruments are easily accessed by the surgeon or assistant while allowing a working space under the surgical drape for the anesthesiologist. Finally, the video monitor is placed at the patient’s head, next to fluoroscopic monitor (Fig. 46.1).
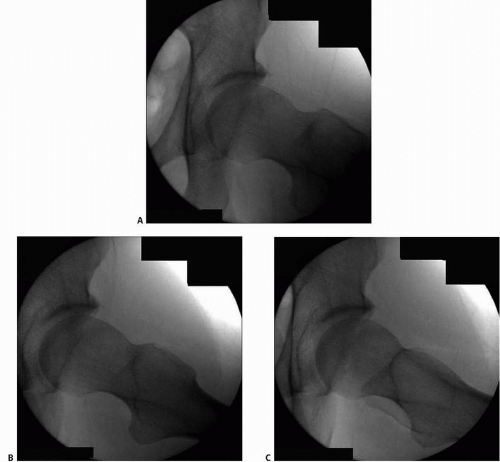
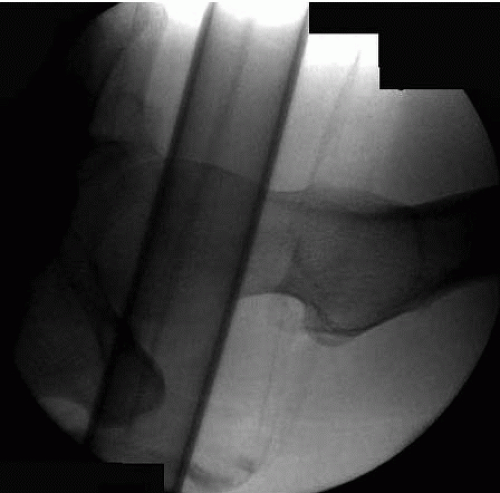
and complete the evaluation of the head-neck junction (Fig. 46.5). Finally, the operative leg is brought back to the “starting position” (neutral abduction, hip flexion of 15° to 20°, full-knee extension, and maximal internal rotation) and traction is applied until adequate distraction of the FH is achieved (Fig. 46.6). In some cases, breaking the seal may be difficult to achieve and gently shaking the hip along with IR and ER of the foot typically achieves atraumatic release of the intra-articular seal in these cases. If the seal is still difficult to release, excessive traction should be avoided and the use of a spinal needle at the beginning of the case will allow for an atraumatic release of the seal. The traction is then released while the leg is prepped and draped to minimize traction time.
safe placement and adequate visualization of the central, peripheral, and peritrochanteric compartments of the hip.
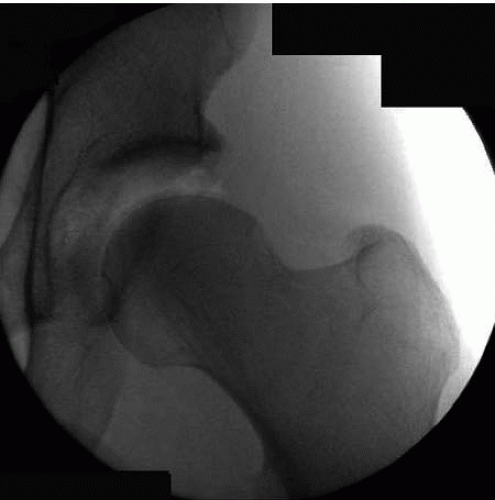 FIGURE 46.6. Intraoperative fluoroscopic image of the hip in traction verifying adequate distractibility (left hip). |
before entering the lateral aspect of the posterosuperior capsule. Byrd (11) described the portal as coursing superior and anterior to the piriformis muscle tendon prior to entering the capsule. However, Robertson and Kelly (10) found that the PL portal passed through the piriformis tendon. This discrepancy may be due to the slight variation in the two authors’ portal placement.
Table 46.1 Distance from portal to anatomic structures | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree