Hemiarthroplasty in the Management of Glenohumeral Arthritis and Irreparable Cuff Insufficiency
Carl J. Basamania
George K. Bal
BACKGROUND
Cuff tear arthropathy is a relatively newly described condition. Codman described a 51-year-old female who was thought to have what he described as a hygroma of the subacromial bursa.7 She was found to have a large collection of semi-viscous fluid within the shoulder in addition to a large, retracted rotator cuff tear. The head of the humerus was nearly devoid of cartilage. He theorized that this degenerative condition of the shoulder was probably the late result of a cuff tear. By all accounts, this case report was an excellent description of the typical findings of cuff tear arthropathy. Although there had been previous reports of patients with massive cuff tears and degenerative conditions of the shoulder as early as 1857,1 it was not until 1975 that Neer introduced the term “rotator cuff tear arthropathy.”24
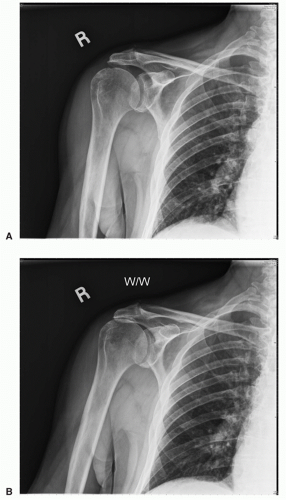
Neer described cuff tear arthropathy as a clinical manifestation of a rotator cuff tear with several specific characteristics. These symptoms included superior migration of head, instability, erosion of the acromion and head, and osteoporosis with collapse of humeral head subchondral bone, as seen in Figure 18-1. Neer et al.24 reported an area of collapse of the proximal aspect of the humeral articular surface in all 26 patients in their series. They considered this finding as a requirement for the diagnosis of rotator cuff tear arthropathy, although it was never made clear why the presence of collapse was a requirement for this diagnosis. Neer did describe a “precollapse” condition of the shoulder as seen in Figure 18-2 that is characterized by the loss of the normal anatomy of the glenohumeral joint, with erosion of the acromion and rounding of the greater tuberosity of the humerus along with narrowing of the acromiohumeral interval to 2 mm or less.23 This “precollapse” state of the shoulder could be considered as a “terminal event” since these probably represent different points in the natural history of the same disease. Once a patient is in the “pre-collapse” stage, there is little difference in the treatment alternatives compared to cuff tear arthropathy.
Rotator cuff tear arthropathy is a condition unique to the shoulder because no other joint has a rotator cuff. It is also unique in that it represents a drastic alteration to joint function. Most other joints undergo degenerative changes. For the most part, their biomechanical function remains the same; the shoulder joint has much poorer, higher friction joint surfaces that compromise function. In the case of cuff tear arthropathy, however, there are significant anatomic and functional alterations that make it quite unlike the original joint. Unfortunately, this problem is further compounded by the fact that there appears to be no way to return the shoulder joint to its nearly normal state as one can with other joint replacements. Cuff tear arthropathy represents the end stage of a mechanical and biological problem for the shoulder.
Once a patient sustains a rotator cuff tear, a number of changes can take place in the shoulder. There is loss of the normal envelope and capsule about the shoulder, possibly resulting in the loss of synovial fluid with subsequent malnutrition of the articular cartilage.9 There are other biochemical changes with the glenohumeral joint in regard to production of various
proteases and collagenases.41 In addition, other investigators have found that patients with large and massive rotator cuff tears have more apatite crystal-induced inflammation.2 The inhospitable environment brought about by these biochemical changes may factor into the irreparability of massive cuff tears.
proteases and collagenases.41 In addition, other investigators have found that patients with large and massive rotator cuff tears have more apatite crystal-induced inflammation.2 The inhospitable environment brought about by these biochemical changes may factor into the irreparability of massive cuff tears.
In addition to these biochemical changes, there are a number of mechanical changes about the shoulder. Loss of cuff function can cause unbalanced force couples about the shoulder with subsequent superior migration of the humeral head.6 This results in mechanical impingement of the head under the acromion. In addition, loss of the normal force couples about the shoulder results in instability of the joint and mechanical abrasion of the cartilaginous surfaces.
One of the difficulties in the treatment of cuff tear arthropathy is simply defining exactly what cuff tear arthropathy actually is. There is a rather large continuum from a simple rotator cuff tear to end-stage rotator cuff tear arthropathy as originally defined by Neer. Cuff tear arthropathy must be differentiated from other conditions that involve deficiencies of the cuff and the presence of arthritis. These conditions include degenerative changes of the glenohumeral joint and a tear of the rotator cuff, inflammatory processes such as rheumatoid arthritis with a dysfunctional cuff, post-traumatic arthritis, low-grade infection, metabolic disease such as gout and pseudogout, and neurogenic conditions such as Charcot arthropathy.
The incidence of rotator cuff tear arthropathy is unknown. Based on his experience, Neer suggested that 4% of patients with a cuff tear go on to develop cuff arthropathy.23,24 Neer postulated that, although the patients may have large cuff tears, some patients may develop bursal envelopes that prevent loss of joint fluid and thus prevent the development of arthropathy due to cartilage malnutrition.23,24 Since no one knows what the true incidence of rotator cuff tears is, it is consequently difficult to determine the true incidence of cuff tear arthropathy. No longitudinal study has assessed the incidence of cuff tear arthropathy; however, Hamada et al.15 reported the long-term radiographic results of non-operative treatment of 22 patients with arthrographically proven massive rotator cuff tears. Five of the seven shoulders that were followed for more than 8 years developed progressive radiographic degenerative changes. Apoil and Augereau3 reported that rotator cuff tear arthropathy developed in more than one-fourth of 56 patients 10 years after open debridement of a degenerative lesion of the rotator cuff. However, these findings are not supported by other studies. In addition to questions about the incidence of cuff tear arthropathy, other questions that have not been answered include, can the progression to arthropathy, if one exists, be altered by physical therapy? What is the role of early surgical intervention in terms of debridement and repair of the cuff in altering the course of this disease process? Finally, are there constitutional factors that predispose some patients to develop arthropathy? We cannot even answer basic questions about predisposing factors. What is the source of pain in a torn rotator cuff? Why do some patients function well without a rotator cuff while others do not? It is doubtful that we will know the cause and incidence of cuff tear arthropathy any time soon.
PHYSICAL FINDINGS
The most consistent finding in cuff tear arthropathy is atrophy of the supraspinatus and infraspinatus muscles (Fig. 18-3). Patients with rotator cuff tear arthropathy may also have an intact posterior cuff, with the tears involving the subscapularis and supraspinatus. In most cases of end-stage rotator cuff tear arthropathy, three or four of the rotator cuff tendons are either completely or partially torn. Patients with significant involvement of the infraspinatus will usually have weakness on external rotation. An external rotation lag sign or horn blower’s sign (Fig. 18-4) may be present due to significant loss of the external rotators, specifically the infraspinatus in the case of the former and both the infraspinatus and teres minor in the latter.35 In addition to external rotation strength testing, it is important to check the status of the patient’s subscapularis with an abdominal compression test or lift-off test.20,30 The loss of the subscapularis can have significant detrimental effects on function as these patients more commonly have anterior- superior escape of the humeral head resulting in a pseudoparalytic shoulder. The surgeon needs to be aware of this specific condition, so that it can be addressed adequately if the patient undergoes an arthroplasty. Active and passive motion should be assessed; passive motion is typically well preserved in these patients. Patients with rotator cuff tear arthropathy typically do not have humeral osteophyte formation or significant capsular contracture. Loss of passive external rotation can occur if the subscapularis is not torn, and excessive passive external rotation may be indicative of a subscapularis rupture. Posterior capsular contracture can be assessed by checking internal rotation with the arm abducted 90 degrees. Significant posterior capsular contractures may shift the instant center of rotation of the humeral head forward during flexion, exacerbating any impingement problem.16,19,31 It is possible that the anterosuperior migration seen often in cuff arthropathy is due to the loss of the subscapularis tendon. The obligate anterior translation of the humeral head may also be worsened by internal rotation contractures.
 FIGURE 18-3. The most consistent finding in cuff tear arthropathy is atrophy of the supraspinatus and infraspinatus muscles. |
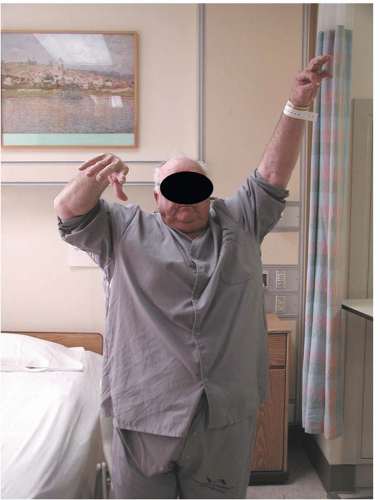 FIGURE 18-4. An external rotation lag sign or horn blower’s sign (Fig. 18-6) may be present due to significant loss of the external rotators, specifically the infraspinatus in the case of the former and both the infraspinatus and teres minor in the latter. |
Most of the patients have profound loss of function, while others have little change in function. Some of these patients may develop a pathologic superior fulcrum under the coracoacromial (CA) arch, resulting in stable shoulder kinematics. This development is probably related to the presence of an adequate residual subscapularis and balanced posterior cuff function6 as well as an intact CA arch. Swelling about the shoulder may be present in addition to loss of the normal biceps contour due to rupture of the long head of the biceps (Fig. 18-5). Anterosuperior subluxation of the humeral head is rare except in patients who have undergone an anterior acromioplasty and resection of the CA ligament. This problem may be further compounded in patients who have lost their subscapularis.22 Although loss of active motion is not unusual, this may be exacerbated by pain. An injection of 10 cc of 1% lidocaine into the subacromial space can be used to try to eliminate the effects of pain.
RADIOGRAPHIC FINDINGS
The diagnosis of cuff tear arthropathy can be easily made on plain radiographs. As mentioned above, the description of cuff tear arthropathy is actually a radiographic description. The axial view should be examined for the presence of anterior
subluxation of the humeral head, which may be indicative of a subscapularis injury. The anteroposterior (AP) radiograph can also show eccentric wear of the glenoid. Unlike osteoarthritis where the glenoid can have posterior erosion, cuff arthropathy patients can have erosion of the superior glenoid tubercle due to eccentric loading and superior migration of the humeral head. This may be a “terminal event” in cuff tear patients as the superior glenoid tubercle may be the last restraint to superior migration of the humeral head.
subluxation of the humeral head, which may be indicative of a subscapularis injury. The anteroposterior (AP) radiograph can also show eccentric wear of the glenoid. Unlike osteoarthritis where the glenoid can have posterior erosion, cuff arthropathy patients can have erosion of the superior glenoid tubercle due to eccentric loading and superior migration of the humeral head. This may be a “terminal event” in cuff tear patients as the superior glenoid tubercle may be the last restraint to superior migration of the humeral head.
 FIGURE 18-5. Swelling about the shoulder may be present in addition to the loss of the normal biceps contour due to rupture of the long head of the biceps. |
The most helpful additional test that should be considered, especially in cases of “pre-collapse,” is the resisted abduction AP or Leclercq radiograph5,14,27 (Fig. 18-6A and B). Often, patients will not have a fixed superior migration of the humeral head and, on static radiographs, the head will appear to be well centered in the glenoid. However, on provocative testing, there may be significant migration due to loss of the cuff and the coronal force couple. If the acromiohumeral interval diminishes on this view, it is highly indicative of a large or massive rotator cuff tear. In Chapter 19, the stress radiograph is performed by fluoroscopic evaluation with active elevation of the shoulder. Either technique is useful. An important message is static AP radiographs can be misleading and do not demonstrate dynamic anterior-superior escape of the humeral head from the CA arch.
Specialized tests, such as magnetic resonance imaging and computed tomography scans, are not necessary to make the diagnosis of cuff tear arthropathy. They may be of some value in assessing the status of the subscapularis, teres minor, and presence of fatty degeneration.
CUFF TEAR ARTHROPATHY CLASSIFICATION
Since the severity of cuff tear arthropathy can vary in patients, it would seem plausible that the degree of superior migration and loss of centralization of the humeral head may have an effect on the patient’s function. Furthermore, it may be that this degree of destabilization could affect the treatment choices for these patients. An effort to categorize cuff tear arthropathy based on the degree of destabilization was proposed by Visotsky.33 The categorization was based on the degree of superior migration from the center of rotation and the amount of instability in the center of rotation. This resulted in the breakdown of cuff tear arthropathy patients into two major groups. In the first group, Type I, the center of rotation remained stable and in the Type II group, the kinematics became unstable due to superior migration of the head. The Type IA subgroup has typical cuff arthropathy changes, specifically, actabularization
of the acromion and femoralization of the head (Fig. 18-7A). Type IB patients have medial erosion (Fig. 18-7B). Type IIA patients have more significant proximal migration but still maintain some stable kinematics due to integrity of the CA arch (Fig. 18-7C). Finally, Type IIB patients have anterior- superior escape due to loss of CA arch37 (Fig. 18-7D). In using this classification, Type IA and IB patients can be treated adequately with a standard hemiarthroplasty or a specific cuff tear hemiarthroplasty with an extended head to allow a greater surface area for articulation. Type IIB patients, because of complete loss of stability, can only be treated adequately with a constrained type of prosthesis such as a reverse total shoulder. It is still not clear which is the best treatment for the Type IIA patients with limited stability. We feel that it would be
best to include a functional parameter to further distinguish this group based on stability. If these patients can forward flex their shoulder at least 80 degrees, they most likely have stable kinematics and can be treated with a hemiarthroplasty. If they do not have at least 80 degrees of motion or if pseudoparalysis is present, they have either limited or poor kinematics and would probably do better with a reverse type of total shoulder. Other considerations that should be taken into account for hemiarthroplasty versus reverse total shoulder replacement in Type IIA patients are age, activity level, and co-morbidities. Given these other factors, reverse total shoulder replacement is preferred in the elderly patients with a lower activity level, particularly those with medical co-morbidities. In this patient population, reverse total shoulder replacement produces better results in most of these patients. Conversely, patients in Type I group could be treated with a reverse type of prosthesis; however, the concern is that a constrained device is not really needed in that group. Furthermore, if one takes into consideration the cost and complications associated with a reverse prosthesis and questionable longevity, especially in a younger patient (<70 years of age), the use of such a device cannot be justified until these concerns have been solved.12,32,36
of the acromion and femoralization of the head (Fig. 18-7A). Type IB patients have medial erosion (Fig. 18-7B). Type IIA patients have more significant proximal migration but still maintain some stable kinematics due to integrity of the CA arch (Fig. 18-7C). Finally, Type IIB patients have anterior- superior escape due to loss of CA arch37 (Fig. 18-7D). In using this classification, Type IA and IB patients can be treated adequately with a standard hemiarthroplasty or a specific cuff tear hemiarthroplasty with an extended head to allow a greater surface area for articulation. Type IIB patients, because of complete loss of stability, can only be treated adequately with a constrained type of prosthesis such as a reverse total shoulder. It is still not clear which is the best treatment for the Type IIA patients with limited stability. We feel that it would be
best to include a functional parameter to further distinguish this group based on stability. If these patients can forward flex their shoulder at least 80 degrees, they most likely have stable kinematics and can be treated with a hemiarthroplasty. If they do not have at least 80 degrees of motion or if pseudoparalysis is present, they have either limited or poor kinematics and would probably do better with a reverse type of total shoulder. Other considerations that should be taken into account for hemiarthroplasty versus reverse total shoulder replacement in Type IIA patients are age, activity level, and co-morbidities. Given these other factors, reverse total shoulder replacement is preferred in the elderly patients with a lower activity level, particularly those with medical co-morbidities. In this patient population, reverse total shoulder replacement produces better results in most of these patients. Conversely, patients in Type I group could be treated with a reverse type of prosthesis; however, the concern is that a constrained device is not really needed in that group. Furthermore, if one takes into consideration the cost and complications associated with a reverse prosthesis and questionable longevity, especially in a younger patient (<70 years of age), the use of such a device cannot be justified until these concerns have been solved.12,32,36
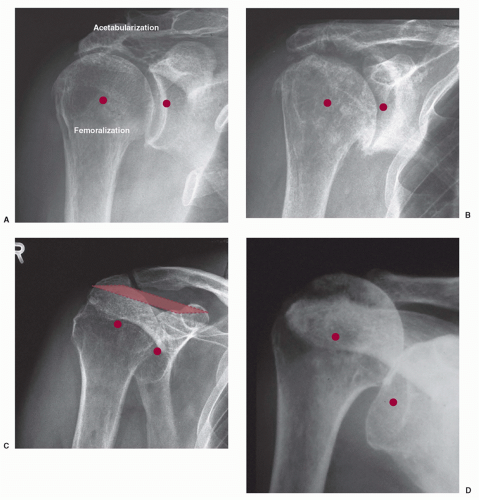 FIGURE 18-7. (A) Type IA subgroup has typical cuff arthropathy changes, specifically acetabularization of the acromion and femoralization of the head. (B) Type IB patients have medial erosion. (C) Type IIA patients have more significant proximal migration but still maintain some stable kinematics due to integrity of the coracoacromial arch. (D) Type IIB patients have anterior-superior escape due to loss of the coracoacromial arch.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|