Abstract
The complications of total hip arthroplasty (THA) during the immediate postoperative period consist mainly in dislocation of the prosthesis, haematomas under antocoagulants, early infections, dismantling of osteotomy, neurological injury, heterotopic ossification and delayed restoration of the range of motion of the hip joint. We present here an infrequently described case of haematoma of the pectineus muscle following THA. Haematomas are not described in literature except in rare cases of compressive haematoma associated with neurological injury. In our case, the intraoperative blood losses were not particularly massive, there were no anticoagulation accident or postoperative trauma and no secondary deglobulinization. The question to be considered is that of a possible stretching of the pectineus during hip dislocation, and possibly during the surgical procedures for the implementation of the prosthesis with increased length, as it is the case here. Haematomas of the pectineus are probably underdiagnosed as they imitate other, more known, symptomatologies.
Résumé
Les complications de prothèse totale de hanche (PTH) durant la période postopératoire immédiate sont principalement : luxations de la prothèse, hématomes sous anticoagulants, infections précoces, démontages d’ostéotomie, atteintes neurologiques, ossifications hétérotopiques et récupérations retardées des amplitudes articulaires. Nous décrivons un cas non habituellement connu d’hématome du muscle pectiné après PTH. Les hématomes ne sont pas décrits dans la littérature en dehors des cas rares d’hématome compressif avec atteinte neurologique. Dans notre cas, les pertes sanguines peropératoires n’étaient pas particulièrement massives, il n’y a pas eu d’accident d’anticoagulation, ni traumatisme postopératoire ni déglobulisation secondaire. Se pose la question du possible étirement du muscle pectiné lors de la luxation de la hanche, et éventuellement lors des gestes opératoires pour mise en place d’une prothèse de longueur augmentée comme ici. Les hématomes du pectiné sont donc probablement sous diagnostiqués car ils miment des symptomatologies plus connues.
1
English version
1.1
Introduction
The annual number of hip prostheses in France is constantly increasing: 73,000 cases for coxarthrosis in 2001 , 135,000 in 2009, representing the second most common surgical procedure. Furthermore, a massive demand is expected in the next 20 years . The complications during the immediate postoperative period (first 2 months) consist mainly in dislocations of the prosthesis, haematomas under anticoagulants, early infections, dismantling of osteotomy, neurological injury, heterotopical ossification and delayed restoration of the range of motion of the hip joint . We are presenting below a less frequently described case of haematoma of the pectineus muscle following a total hip arthroplasty.
1.2
Case study
This 75-year-old man was admitted for a right hip prosthesis because of an evoluted coxarthrosis on dysplasia in absence of acetabular coverage. His only history consisted in colonic diverticulosis, appendicectomy, biliary surgery as well as prostate adenoma resection. There was no existing coagulation disorder.
The hip prosthesis replacement was made in left lateral position with, first, a posterolateral approach after Moore, without immediate complication. The implants trade name is Tornier (38330 Saint-Ismier–France): acetabular cup Dynacup size 56, prosthesis Meije Duo size 5 (femur neck lateralized and of 4 mm increased length), ceramic head of a diameter of 36. The patient received low molecular weight heparin injections at preventive dosage.
The patient was admitted in the physical and rehabilitation medecine department at D7: the testing allowed a right hip range of motion limited to 75/5/15 (adduction and rotations being not graded), and regarding the muscles, the gluteal muscles and hip flexors were very poor at M2. The patient complained of pain at the fold of the groin and presented with a subcutaneous haematoma visible at the inner thigh. After 15 days of rehabilitation, the functional evolution was satisfactory allowing walking with canes. The range of motion had improved, with flexing rated at 105°. Muscular testing had also improved with all muscles at M4 except the hip flexors still at M2 and the inability to raise the heel from the bed. Furthermore, the patient complained of persistent pain at the fold of the groin, regularly graded 5 or 6 out of 10 on visual analog scale (VAS) and increased at the end of the hip flexing, making it difficult to climb the stairs, in adduction as well as in dorsal decubitus (extension at 0°). Walking on even ground was not painful.
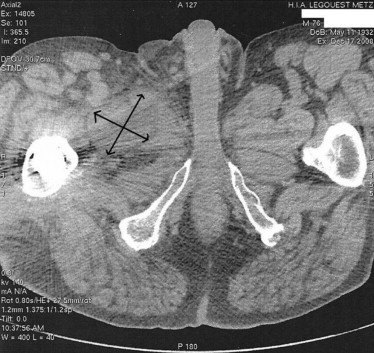
The classical radiography considered as normal was not contributive ( Fig. 1 ). A CAT-scan was then carried out which revealed a haematoma of the right pectineus muscle associated with a right posterior subcutaneous haematoma facing the surgical procedure site ( Fig. 2 ). CAT-scan was preferred to echography (the reference examination in the early diagnosis of haematomas) in view of this unusual symptomatology. The biological follow-up showed an inflammatory syndrome always decreasing (absence of hyperleucocytosis and CRP at 9 mg/L). The relevance of draining was discussed, the patient considering that he had regained sufficient autonomy (walking with a cane at a 2 km/h speed), he wanted to get back home as soon as possible. In absence of secondary clinical worsening, it was decided not to delay the patient’s discharge from hospital. The patient was informed of the necessity to reconsult immediately in case of modification of the symptomatology.

The patient was seen regularly as outpatient: at 1 month after discharge with hip flexors graded at M3 and a right hip range of motion at 100/−5/30. This range of motion is lower than that usually found at this postsurgery stage in this patient whose pain hindered the physiotherapy. At month 3, the motor recovery was complete, at 1 year, there was no deficit either. Considering the good clinical evolution, no control by imaging was performed.
1.3
Discussion
Following a total hip prosthesis, the causes of pain are numerous and of varied origins : first, pain due to the approach, extraprosthetic causes (rachidian pathology, tendinomyopathy of the hip abductors), infectious or mechanical etiologies (failure of anchorage, conflict pathology).
Haematomas are not described in literature, except in rare cases of compressive haematomas . This complication is classically described as following bad anticoagulation (overdosing) or insufficient hemostasis. It usually appears as a progressive external sciatic polpliteal paralysis with deglobulinization. If it appears early, the differential diagnosis with primary neurological injury without haematoma, most frequently due to an indirect trauma (compression, stretching or intraoperative ischemia), may be problematic.
Pouliot described in 2008 a unique case of major retroperitoneal haematoma which occurred three years and a half after surgery and was attributed to an iliopsoas/cup conflict .
Moreover, the muscular haematomas found in haemophilia are most frequently related to the psoas-iliac with often the spontaneous onset of pain at the groin exacerbated during flexing of the hip against resistance. The other muscular sites in this disorder of the coagulation are the upper limb muscles, the calf and the thigh, without any description of an individualized haematoma of the pectineus muscle .
In the present case, the intraoperative blood losses were not particularly massive for this type of surgery (loss of 3.9 points of haemoglobin), there was no anticoagulation accident, there were no postoperative trauma and no secondary deglobulinization.
The question is raised of a possible stretching of the pectineus muscle during the hip dislocation, and perhaps during the surgical procedures in use for the implementation of a prosthesis of increased length as was the case here (the tests with a standard prosthesis not allowing the restoration neither of the offset nor of the length).
Our clinical case presents the originality of having imitated a haematoma of the psoas considering the impossibility to actively raise the heel in dorsal decubitus and the onset of pain at the end of passive flexing, without any discomfort when walking.
Since the classical complications have not been proven on classical radiography and the limitation of the functional state being persistent, it was justified to use the CAT-scan, an imaging which may have its proper limits but revealed to be of helpful contribution in our case. However, echography remains the examination of reference, and would probably have led to the diagnosis, while being nonradiant.
Finding out an isolated haematoma of the pectineus muscle reminds us that if this muscle is often, by convenience, assimilated to the adductors, it is not part of them. Inserted from the pubis (pectineal crest) to the medial branch of trifurcation of linea aspera and innervated by the obturator nerve, its twisted muscular fibres allow it to be altogether flexor of the hip (incidently), adductor, and external rotator, and make it an excellent coaptor of the hip .
1.4
Conclusion
To our knowledge, there is no other example in literature of haematoma of the pectineus. If this observation appears as nondescribed previously, it is justified to examine the incidence of the onset of haematomas of the pectineus muscle during surgery of total hip prosthesis which are not identified as such because potentially taken for haematomas of the psoas, more frequent. It would be of interest to investigate this onset with regard to the different surgical approaches.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







