Glenoid Replacement: Technical Considerations
Julie Y. Bishop
Ian K. Y. Lo
Evan L. Flatow
INTRODUCTION
It has been generally accepted through the years that when damage to the glenoid articular surface is significant, consideration should be given to glenoid resurfacing. When large cysts are present in the subchondral bone and underlying vault, severe irregular erosion or incongruity of the glenoid surface is present; when there is posterior erosion of the glenoid, glenoid replacement is indicated. However, concern for component survival has prompted many surgeons to consider humeral head replacement without glenoid resurfacing (“hemiarthroplasty”) for glenohumeral arthritis. Studies have shown that resurfacing the glenoid during shoulder replacement provides predictable pain relief and functional improvement in patients with degenerative arthritis (1, 2, 3). These studies include a meta-analysis of prospective randomized trials, which reported better pain control and function in patients undergoing total shoulder replacement versus humeral head replacement (2). Therefore, the current trend is to replace the glenoid whenever the patient has adequate soft-tissue support and glenoid bone stock. Glenoid resurfacing generally is avoided when there is insufficient bone to implant a component or when the rotator cuff is severely deficient or irreparable. Obtaining adequate exposure is a critical aspect of glenoid component implantation and has been one of the most challenging aspects. Glenoid component loosening has been a major concern and the most common complication of glenoid replacement. However, the correlation between radiographic evidence of loosening and actual symptomatic loosening is still unclear. Thus, this chapter will address not only the technical aspects of glenoid component implantation but also glenoid component loosening, the significance of radiolucent lines, and how to address any bony deficiencies that may be present.
GLENOID LOOSENING
Glenoid loosening remains the most common long-term complication of total shoulder replacement (4, 5, 6, 7, 8, 9, 10, 11, 12). Early loosening can be caused by unequal stress distribution
resulting from abnormal migration of the humeral component as occurs with rotator cuff deficiency or shoulder instability (13,14). Other possible causes for early loosening include prosthetic design (i.e., metal backed), infection, inadequate bone stock, or poor fixation to bone (6,15). Thus, with the trend turning toward more glenoid resurfacing procedures, emphasis must be placed on improving the quality of glenoid fixation. This in turn is dependent on the technical aspects of fixation, the quality of bone stock (or rather the amount of glenoid deficiency), the presence of glenohumeral instability, and the function of the rotator cuff.
resulting from abnormal migration of the humeral component as occurs with rotator cuff deficiency or shoulder instability (13,14). Other possible causes for early loosening include prosthetic design (i.e., metal backed), infection, inadequate bone stock, or poor fixation to bone (6,15). Thus, with the trend turning toward more glenoid resurfacing procedures, emphasis must be placed on improving the quality of glenoid fixation. This in turn is dependent on the technical aspects of fixation, the quality of bone stock (or rather the amount of glenoid deficiency), the presence of glenohumeral instability, and the function of the rotator cuff.
Radiographic Evaluation
Routine radiographic series has long been the standard evaluation for detecting radiolucent lines and subsequent glenoid loosening. However, the accuracy of radiographs for measurement of radiolucent lines has been debated because differences in patient positioning and individual variations in glenoid version can produce incomparable serial radiographs, making assessment of the bone-cement interface difficult (19,37,38). Although fluoroscopy and computerized tomography (CT) both may improve the accuracy of evaluating the bone-implant interface (40,41), the senior author feels that anteroposterior (AP) and axillary views can be considered as accurate when the outline of the glenoid component can be seen in profile with sharp edges on both views. With increasing glenoid rotation, the accuracy of determining the size and presence of lucent lines is decreased. Some authors suggest that all radiographs be made within 10 degrees of neutral to allow accurate assessment of radiolucent lines about the glenoid (38).
Radiolucent Lines
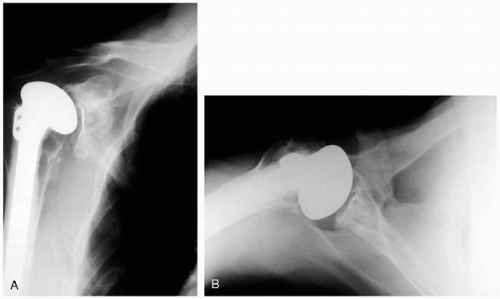
Radiolucent lines found at the bone-cement interface of the glenoid component have been a common finding. Reported rates range from 12% to 94% (4,6,16, 17, 18, 19, 20, 21, 22, 23). The significance, the location, and the size of radiolucent lines have long been a controversial topic (10,19,24). Although longer term follow-up has correlated an increased incidence of radiolucent lines with component loosening and symptoms (4,18,20,23,25, 26, 27), others found no relation between the incidence of radiolucent lines to symptomatic clinical loosening (4,6,19,28, 29, 30). More recent studies have found an increased incidence of radiolucencies with keel versus pegged components (36). Although the mere presence of a radiolucent line does not itself signal component loosening, the progressive widening of radiolucent lines on serial radiographs likely does (4,20,26,28,31,32). Radiographic loosening has in the past been defined as a line that is greater than 2 mm wide at the bone-cement interface, or overall progressive radiolucency (Fig. 4-1) (4,6,24,33,34). Collectively, most studies do agree that operative technique, glenoid preparation, and cementing protocol are all important surgical factors in avoidance of radiolucent lines. However, no definitive protocol has been delineated. Early techniques for placing glenoid components generally have used manual cement pressurization, with no specifically designed instruments, and resulted in a high incidence of radiolucent lines. Modern techniques for
pressurizing the cement have been developed using specifically designed instruments, which can decrease the incidence of immediate radiolucent lines (35). However, a study in 2002 still described a 94% incidence of radiolucent lines (36). The senior author has helped to develop a specific protocol for glenoid resurfacing using modern instrumented cement pressurization. This technique, which will be described in detail, when compared to the previous manual packing technique, has been found to reduce the overall incidence of radiolucent lines for both keeled and pegged components. Furthermore, when comparing components that were implanted with the new cementing technique, pegged components appeared to have fewer radiolucent lines than keel components. This finding has also been confirmed in a previous study (36), yet it is uncertain why this may be. This may be related to the geometry of the peg component, which may allow for a more precise fit, or the rounded design of pegs, which may make it difficult to visualize a clear border; possibly it could signify better pressurization of the cement in a smaller space. Still, both keeled and pegged components placed with instrumented pressurization techniques resulted in a low incidence of radiolucent lines; thus the senior author feels that either component still can be used based on preference. Although long-term follow-up is not yet available, the hope is that the reduction of radiolucent lines will also decrease glenoid loosening and improve overall component survival (Fig. 4-2).
pressurizing the cement have been developed using specifically designed instruments, which can decrease the incidence of immediate radiolucent lines (35). However, a study in 2002 still described a 94% incidence of radiolucent lines (36). The senior author has helped to develop a specific protocol for glenoid resurfacing using modern instrumented cement pressurization. This technique, which will be described in detail, when compared to the previous manual packing technique, has been found to reduce the overall incidence of radiolucent lines for both keeled and pegged components. Furthermore, when comparing components that were implanted with the new cementing technique, pegged components appeared to have fewer radiolucent lines than keel components. This finding has also been confirmed in a previous study (36), yet it is uncertain why this may be. This may be related to the geometry of the peg component, which may allow for a more precise fit, or the rounded design of pegs, which may make it difficult to visualize a clear border; possibly it could signify better pressurization of the cement in a smaller space. Still, both keeled and pegged components placed with instrumented pressurization techniques resulted in a low incidence of radiolucent lines; thus the senior author feels that either component still can be used based on preference. Although long-term follow-up is not yet available, the hope is that the reduction of radiolucent lines will also decrease glenoid loosening and improve overall component survival (Fig. 4-2).
Glenoid Bony Deficiencies
A major technical factor limiting the use of glenoid components has been glenoid bone stock deficiency. Initial assessment of bone deficiency can be made on routine radiographs of the glenohumeral joint. A true AP of the glenohumeral joint, an axillary, and a scapular lateral are the standard radiographs obtained in preparation for a shoulder arthroplasty. The axillary can best evaluate posterior glenoid wear; however, true asymmetry at times is difficult to ascertain. Thus, if there is significant asymmetry or the bony wear pattern is unclear, a CT scan can be obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree