Glenoid Bone Graft for Instability with Bone Loss
Ryan W. Simovitch
William E. Bragg
Alex Girden
Laurence D. Higgins
Jon J. P. Warner
DEFINITION
Anterior shoulder instability typically results from an injury to the capsule, ligaments, and labrum that stabilize the glenohumeral joint.
In cases of higher energy trauma or recurrent dislocation, there can be significant bone loss or erosion of the anterior glenoid rim.
The key to correctly treating anterior shoulder instability is to recognize whether the lesion involves injury to only soft tissue structures (capsule, labrum, ligaments) or if it also involves the anteroinferior glenoid bone.
ANATOMY
Shoulder stability is provided by both dynamic and static stabilizers (FIG 1).
Dynamic stabilizers include the following:
Rotator cuff
Biceps
Coordinated scapulothoracic motion
Proprioception
Static stabilizers include the following:
Bony anatomy of the glenoid and humeral head
Labrum
Glenohumeral capsule and ligaments
Negative intra-articular pressure
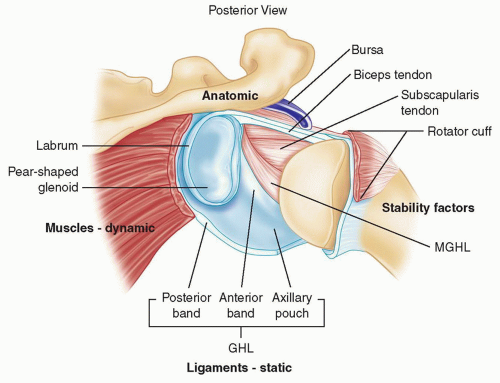
FIG 1 • Shoulder stability depends on the interaction of dynamic and static soft tissue restraints. The bony architecture of the glenoid and humerus also plays a critical role.
The inferior glenohumeral ligament (IGHL) complex limits anterior translation of the humeral head on the glenoid in abduction. It takes origin from the labrum of the inferior glenoid. The complex consists of an anterior band, posterior band, and intervening pouch. The anterior band is responsible for anterior restraint with the arm in high degrees of abduction with external rotation. The posterior band limits posterior translation in abduction and internal rotation.
The humeral head has a surface area approximately 2 to 3 times that of the glenoid, which results in relatively limited bony stability at the shoulder.13
Normal glenoid morphology is the shape of a pear. Contact between the glenoid and humeral head is dependent on shoulder position, with contact area ranging from approximately 10% to 67% of the glenoid surface through the range of motion (see FIG 1).14
The synchronized contractions of the rotator cuff and biceps provide a compressive force directing the convex humeral head into the concave glenoid and labrum unit. This is known as concavity compression.9
PATHOGENESIS
Anterior shoulder instability may occur following a dislocation event that results from a fall or collision with the arm in external rotation and abduction.
An initial dislocation typically requires a closed reduction of the shoulder after muscle relaxation and sedation. Patients
with recurrent dislocations can often self-reduce their shoulders with minimal effort.
A rotator cuff tear should be suspected in patients older than 40 years old who suffer a dislocation episode.
An injury to the labrum in the anteroinferior quadrant of the glenoid can destabilize the IGHL complex as well as stretch or tear the anteroinferior capsule, resulting in anterior shoulder instability.
Recurrent anterior glenohumeral instability can also occur in the setting of anterior glenoid bone loss due to glenoid fracture after a single dislocation event. Instability may also occur from erosion of the glenoid rim as a result of recurrent subluxations or dislocations.
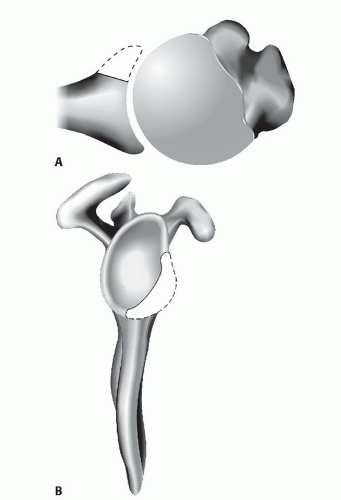
Deficiency of the anterior glenoid rim disrupts the normal mechanism of concavity compression as a result of a decrease in width and depth of the socket (FIG 2).8
Anterior glenoid bone loss or fracture should be suspected in cases of recurrent anterior instability or acute dislocations from a high-energy mechanism.
In cases of anterior glenoid bony deficiency, patients often report recurrent dislocation in their sleep and with minimal trauma.
NATURAL HISTORY
In the context of anterior glenoid bone loss, both open and arthroscopic soft tissue management of anterior shoulder instability have demonstrated increased failure rates compared to the results in patients with normal bony glenoid anatomy.1,2
Burkhart and DeBeer3 have shown that contact athletes with substantial bony glenoid defects, noted as an “inverted pear” morphology at arthroscopy, had an 87% recurrent instability rate compared to 6.5% in contact athletes with a normal bony glenoid who underwent an arthroscopic capsulolabral repair only.
Given the high-failure rate in patients with significant anterior glenoid bone loss, a comprehensive evaluation of the glenoid bony anatomy is imperative before treating recurrent anterior shoulder instability with a capsulolabral reconstruction alone.
PATIENT HISTORY AND PHYSICAL FINDINGS
A complete examination of the shoulder should also include an evaluation for concomitant injuries, and other etiologies of shoulder pain must be ruled out. A thorough examination includes, but is not limited to, the following:
Apprehension test: Apprehension, not simply pain, is required for a positive apprehension test.
Relocation test: Relief of apprehension with posterior pressure is necessary for a positive relocation maneuver.
Load and shift test: The examiner should note the degree of displacement of the humeral head on the glenoid rim.
Belly press: A positive belly press test is when the patient must flex the wrist and extend the arm to maintain the palm of the hand on the abdomen. This indicates insufficiency of the subscapularis muscle.
Assessment for generalized ligamentous laxity: Specifically, hyperextension of the elbows and knees as well as the ability to oppose the thumb to the forearm should be noted.
Rotator cuff: Manual strength testing of the subscapularis, supraspinatus, infraspinatus, and teres minor muscles must be done. Rotator cuff tears can contribute to instability.
Subscapularis insufficiency: Weakness of internal rotation with the shoulder adducted to the side suggests a subscapularis injury but is not specific. Increased external rotation of the injured side with the shoulder adducted compared to the contralateral shoulder, pain with external rotation of the shoulder, a positive belly press sign, or positive lift-off sign should raise suspicion for subscapularis insufficiency.
Deltoid motor strength and lateral shoulder sensation: Weakness of the deltoid in conjunction with decreased sensation of the lateral shoulder indicates axillary nerve injury. Atrophy of the deltoid muscle should also be noted.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs are useful to detect Hill-Sachs lesion, glenoid dysplasia, and anterior glenoid fractures or erosion. Standard images should include a true anteroposterior (AP) view of the glenoid, an axillary lateral view, and a Stryker notch view. Fractures and erosions of the glenoid as well as the position of the humerus on the glenoid should be noted.
If a significant anterior bony glenoid lesion is suspected owing to plain film findings or a history of recurrent dislocations, a computed tomography (CT) arthrogram should be obtained. This study allows an evaluation of the subscapularis
tendon, bony architecture of the glenoid, humeral head and tuberosities as well the degree of capsulolabral injury and redundancy.
A diagnostic agreement study by Rerko12 comparing the accuracy of x-ray, magnetic resonance imaging (MRI), and CT in quantifying glenoid bone loss in recurrent anterior shoulder instability found that three-dimensional (3-D) CT and CT were the most reliable methods.
Both Itoi et al7,8 and Gerber5 have described techniques to quantitatively assess anterior glenoid bone that serve as a guide when bony augmentation is indicated in the treatment of recurrent anterior shoulder instability.
Gerber’s method5 is easily performed on oblique sagittal or 3-D CT reconstructions of the glenoid surface (FIG 3).
Cadaveric studies have shown that the force required for anterior dislocation is reduced to 70% of that required to dislocate an intact glenoid if the length of the glenoid defect measures more than half of the maximal AP diameter of the glenoid fossa.3
DIFFERENTIAL DIAGNOSIS
Bankart lesion
Multidirectional instability
Hill-Sachs lesion
Tuberosity fracture
Rotator cuff tear (especially subscapularis)
Scapular winging (especially serratus anterior dysfunction)
Axillary nerve injury
NONOPERATIVE MANAGEMENT
Nonoperative treatment for recurrent anterior shoulder dislocation includes strengthening of the rotator cuff musculature as well as the periscapular stabilizers. Deltoid muscle strengthening should be incorporated into a rotator cuff strengthening protocol. Periscapular strengthening should focus on the rhomboids, trapezius, serratus, and latissimus dorsi muscles.
Nonoperative treatment of recurrent shoulder dislocation in the setting of a bony glenoid defect, however, is rarely successful.1,2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree