Glenohumeral Arthrodesis
Brent B. Wiesel
Robin R. Richards
DEFINITION
Despite significant advances in shoulder arthroplasty and other reconstructive procedures, glenohumeral arthrodesis remains an important treatment option in appropriately selected patients.
The goal of glenohumeral arthrodesis is to provide a stable base for the upper extremity to optimize elbow and hand function.
Given the tremendous normal range of motion of the glenohumeral joint and the relatively small amount of surface area available for fusion, particularly on the scapular side, successful arthrodesis is technically demanding and requires meticulous surgical technique.
ANATOMY
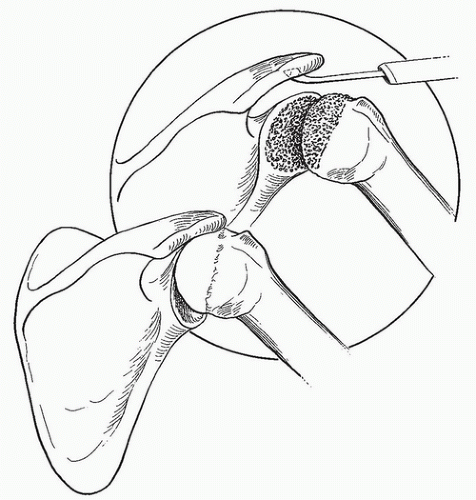
The surface area of the glenoid is too small to allow for predictable fusion. Therefore, to increase the area available for fusion, the glenohumeral articular surface and the articulation between the humeral head and undersurface of the acromion are decorticated (FIG 1).
The bone of the scapula is extremely thin, with only the glenoid fossa and base of the coracoid providing sufficient strength for fixation.
We use a position of 30 degrees of abduction, 30 degrees of forward flexion, and 30 degrees of internal rotation.
This position brings the hand to the midline anteriorly, allowing the patient to reach his or her mouth with elbow flexion.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history and physical findings are specific to the underlying condition requiring arthrodesis.
The common finding among all patients is symptomatic dysfunction at the glenohumeral joint that prevents them from effectively using the involved extremity.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard radiographs, including an anteroposterior (AP), lateral, and axillary view, are used to assess any deformities as well as the bone stock available for fusion.
A computed tomography (CT) scan can be used if there is concern regarding bone loss on the glenoid side, especially in the setting of failed arthroplasty.
When the neurologic condition of the shoulder girdle muscles is unclear, electrodiagnostic testing of the scapular muscles is indicated.
SURGICAL MANAGEMENT
Indications
The presence of a flail shoulder is an indication for glenohumeral arthrodesis.
Paralysis in patients with a flail shoulder can be the result of anterior poliomyelitis, severe proximal root or irreparable upper trunk brachial plexus lesions, or isolated axillary nerve paralysis.
Many patients with flail shoulders develop a painful inferior subluxation that responds well to arthrodesis.
The need for fusion following isolated axillary nerve injury depends on the level of impairment. Many patients, especially those with partial paralysis, have reasonable function; however, complete injury often leads to pain and significant limitation of shoulder function.
Glenohumeral arthrodesis is useful following en bloc resection of periarticular malignant tumors requiring resection of the deltoid, rotator cuff, or both.
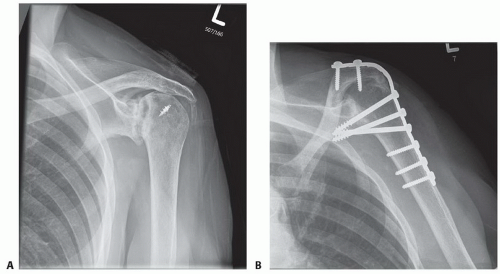
Fusion is useful for the treatment of joint destruction following septic arthritis of the shoulder, particularly in young patients (FIG 2).
Arthrodesis is a salvage option for patients with multiple failed total shoulder arthroplasties who have insufficient bone stock or soft tissue for revision arthroplasty.
Symptomatic, uncontrolled shoulder instability that is recalcitrant to soft tissue or bony reconstructive procedures can be managed with fusion.
Rarely, arthrodesis is indicated in young laborers with severe osteoarthritis who are poor candidates for arthroplasty because of their young age and high activity levels.
Contraindications
The primary contraindication to glenohumeral arthrodesis is weakness or paralysis of the periscapular muscles, especially the trapezius, levator scapula, and serratus anterior.
Progressive neurologic disorders that are likely to lead to paralysis of these muscles also are a contraindication.
Arthrodesis of the opposite shoulder is a contraindication to fusion.
Shoulder fusion requires a significant effort by the patient to rehabilitate the shoulder and is contraindicated in patients who are unwilling or unable to participate in such a program.
Preoperative Planning
Preoperative radiographs should be evaluated for any bone defects that may require bone grafting.
The surgeon should make sure that a 10-hole pelvic reconstruction plate and a set of handheld bending irons are available (FIG 3).
Positioning
The patient is placed in the beach-chair position with the back of the table elevated 30 to 45 degrees.
A folded sheet is placed medial to the scapula to elevate it from the table.
The drapes are applied as medial as possible, allowing access to the scapula and the anterior chest wall. The arm is draped free (FIG 4).
We do not routinely use intraoperative fluoroscopy; however, early in their experience with this procedure, surgeons may find fluoroscopy useful to confirm the position of the hardware.
Approach
We perform glenohumeral arthrodesis using a 10-hole, 4.5-mm pelvic reconstruction plate.
Compression across the glenohumeral articular surface is achieved by placing the initial screws from the plate through the proximal humerus and into the glenoid fossa.
The plate is then anchored to the spine of the scapula by a screw directed into the base of the coracoid.
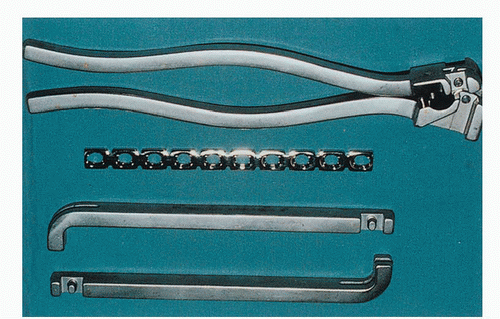 FIG 3 • Handheld bending irons and a plate press are needed to contour the 4.5-mm pelvic reconstruction plate. (From Iannotti JP, Williams GR, eds. Disorders of the Shoulder: Diagnosis and Management, ed 2. Philadelphia: Lippincott Williams & Wilkins, 2007:684.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|