Glenohumeral Arthrodesis
Robin R. Richards
INTRODUCTION
The advent of total shoulder arthroplasty and the refinement of other reconstructive procedures have narrowed the indications for glenohumeral arthrodesis.50 Nevertheless, arthrodesis of the glenohumeral joint continues to provide a valuable method of shoulder reconstruction for specific indications.19,29,80 Although the procedure is infrequently performed, it reliably provides patients with a stable, strong shoulder. Albert first attempted glenohumeral arthrodesis in 1881. Since then a voluminous literature has evolved outlining different indications for the procedure and a variety of surgical techniques for performing glenohumeral arthrodesis. Controversies have developed in the literature about the indications for the procedure and the optimum position for glenohumeral arthrodesis.2,62 More recently, discussion has arisen of the functional results that can be achieved with the procedure.15,30 In this chapter, the complex and revision problems are addressed and then the complications and the results of glenohumeral arthrodesis are discussed.
Arthrodesis is an important method of shoulder reconstruction. The procedure has stood the test of time and continues to deserve a place in the shoulder surgeon’s armamentarium. For certain specific indications, it provides the best method of restoring function to the shoulder.
INDICATIONS
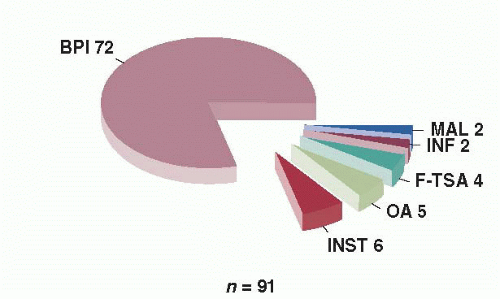
Glenohumeral arthrodesis can effectively restore shoulder function to highly selected patients. Successful glenohumeral arthrodesis reliably results in a strong and stable shoulder. However, the procedure sacrifices all rotation through the glenohumeral joint. Wherever possible, shoulder arthroplasty is preferable to glenohumeral arthrodesis, if for the particular patient there is a choice between the two procedures (Fig. 26-1). Shoulders can be fused if an arthroplasty fails, although fusion in this situation is a technical challenge. The indications for surgery in the author’s personal series are illustrated in Figure 26-2.
Paralysis
All authors agree that the presence of a flail shoulder is an indication for glenohumeral arthrodesis. Patients with anterior poliomyelitis, severe proximal root, and irreparable upper trunk brachial plexus lesions and some patients with isolated axillary
nerve paralysis are candidates for glenohumeral arthrodesis.59,61 These patients have good function in their elbows and hands, but are unable to optimize their upper extremity function because of their inability to place their hand in space. If such a patient has good function in the periscapular musculature, particularly the trapezius, levator scapula, and serratus anterior, glenohumeral arthrodesis stabilizes the extremity and allows effective hand function.54 Such patients can then fully utilize their upper extremity potential and can work effectively at bench level. In addition, many patients with flail shoulders develop inferior subluxation of the glenohumeral joint owing to periarticular paralysis (Fig. 26-3). This condition is uncomfortable and, in some patients, frankly painful. Such patients often find that they must keep their arm in a sling to avoid injuring it. Painful inferior subluxation of the shoulder provides another indication for stabilization of the glenohumeral joint.
nerve paralysis are candidates for glenohumeral arthrodesis.59,61 These patients have good function in their elbows and hands, but are unable to optimize their upper extremity function because of their inability to place their hand in space. If such a patient has good function in the periscapular musculature, particularly the trapezius, levator scapula, and serratus anterior, glenohumeral arthrodesis stabilizes the extremity and allows effective hand function.54 Such patients can then fully utilize their upper extremity potential and can work effectively at bench level. In addition, many patients with flail shoulders develop inferior subluxation of the glenohumeral joint owing to periarticular paralysis (Fig. 26-3). This condition is uncomfortable and, in some patients, frankly painful. Such patients often find that they must keep their arm in a sling to avoid injuring it. Painful inferior subluxation of the shoulder provides another indication for stabilization of the glenohumeral joint.
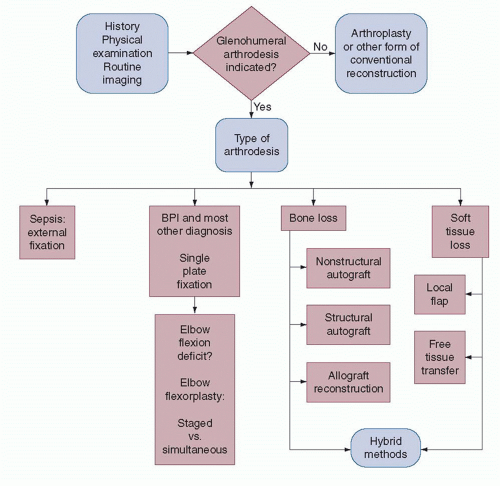 FIGURE 26-1. Algorithm for evaluation and management of patients presenting to be considered for glenohumeral arthrodesis. BPI, brachial plexus injury. |
Patients who have the combination of a flail shoulder and flail elbow need both shoulder and elbow reconstruction. In this situation, glenohumeral arthrodesis combined with elbow flexorplasty improves the result of the elbow flexorplasty. Without shoulder stabilization, elbow flexion tends to drive the humerus posteriorly, resulting in shoulder extension, rather than elbow flexion. Arthrodesis of the shoulder in some flexion and abduction helps prevent this phenomenon and optimizes the result that can be achieved with the elbow flexorplasty. Patients with flail shoulders often have a tendency to internally rotate their upper extremity to their chest when some function remains in the powerful internal rotators of the shoulder (pectoralis major, latissimus dorsi) and no function remains in the external rotators. Shoulder stabilization either in the form of arthrodesis or L’Episcopo tendon transfer reduces this undesirable tendency.54
There is a wide degree of variability in the disability caused by axillary nerve paralysis, and many patients have virtually full motion following paralysis of the axillary nerve, provided the rotator cuff musculature is undisturbed (endurance is never normal). Patients with isolated paralysis of the axillary nerve can
be treated by either muscle or tendon transfer or glenohumeral arthrodesis. Numerous reports exist in the literature on the value of muscle and muscle tendon transfer to restore shoulder function following paralysis of the axillary nerve.28 It is generally agreed that multiple transfers are necessary to restore deltoid function and that significant problems can occur with gliding of transfers over the acromion. It is often necessary to harvest autogenous tissue, such as fascia lata, to prolong the transfers, and the process of rehabilitation is challenging following such procedures. In author’s experience such transfers are indicated primarily for pediatric patients and adult patients who have only partial paralysis of the axillary nerve.28 However, pediatric patients do well with glenohumeral arthrodesis, and some authors feel they are better able to adapt to the procedure.40 If total paralysis of the axillary nerve is present and significant limitation of shoulder function ensues, glenohumeral arthrodesis is recommended by the author, recognizing that the alternative of muscle transfers may be available in carefully selected patients. Glenohumeral arthrodesis is useful in such patients, provided their symptoms justify the procedure. El-Gammal used freefunctioning gracilis transplantation combined with shoulder arthrodesis to restore function in pediatric patients with elbow and shoulder paralysis caused by poliomyelitis.24
be treated by either muscle or tendon transfer or glenohumeral arthrodesis. Numerous reports exist in the literature on the value of muscle and muscle tendon transfer to restore shoulder function following paralysis of the axillary nerve.28 It is generally agreed that multiple transfers are necessary to restore deltoid function and that significant problems can occur with gliding of transfers over the acromion. It is often necessary to harvest autogenous tissue, such as fascia lata, to prolong the transfers, and the process of rehabilitation is challenging following such procedures. In author’s experience such transfers are indicated primarily for pediatric patients and adult patients who have only partial paralysis of the axillary nerve.28 However, pediatric patients do well with glenohumeral arthrodesis, and some authors feel they are better able to adapt to the procedure.40 If total paralysis of the axillary nerve is present and significant limitation of shoulder function ensues, glenohumeral arthrodesis is recommended by the author, recognizing that the alternative of muscle transfers may be available in carefully selected patients. Glenohumeral arthrodesis is useful in such patients, provided their symptoms justify the procedure. El-Gammal used freefunctioning gracilis transplantation combined with shoulder arthrodesis to restore function in pediatric patients with elbow and shoulder paralysis caused by poliomyelitis.24
Reconstruction Following Tumor Resection
En bloc resection of periarticular malignant tumors often requires sacrifice of the rotator cuff or the deltoid, or both. If the resection requires sacrifice of these tissues, reconstruction of the shoulder with an arthroplasty is inadvisable owing to the high risk of instability if an unconstrained prosthesis is used and to the certainty of loosening if a constrained prosthesis is used. Kiss et al. reviewed 91 shoulder resections and found that the best results were achieved when the function of the rotator cuff was preserved.34
Glenohumeral arthrodesis is the procedure of choice to reconstruct the shoulder following wide resection of periarticular malignancies. Specific techniques have been recommended for glenohumeral arthrodesis following tumor resection.39 These include the use of specialized fixation devices and bone-grafting techniques. Vascularized bone grafts and massive allografts are sometimes necessary because of the large defects created by tumor resection.37 These techniques will be discussed later.
Shoulder Joint Destruction by Infection
Destruction of the shoulder joint by septic arthritis remains an indication for glenohumeral arthrodesis. In the past, tuberculous arthritis was a common indication for glenohumeral arthrodesis. Worldwide, this condition remains prevalent, although in the Western world it has become relatively uncommon. Septic arthritis continues to occur, and when it does, the shoulder joint can be destroyed with resultant pain and limitation of function. Most surgeons would agree that in a young patient with shoulder dysfunction, for this reason, arthrodesis of the shoulder, as opposed to total shoulder arthroplasty, would be indicated. Although total shoulder arthroplasty can be performed in patients with a remote history of sepsis, if there is a recent history of sepsis or if the patient is young, arthrodesis provides a more satisfactory alternative.
Wick et al. reported the long-term results after infection in 15 patients. Complications occurred in five patients. The complication rate was lower in patients less than 50 years of age and in those patients who had fewer than four previous operations.79
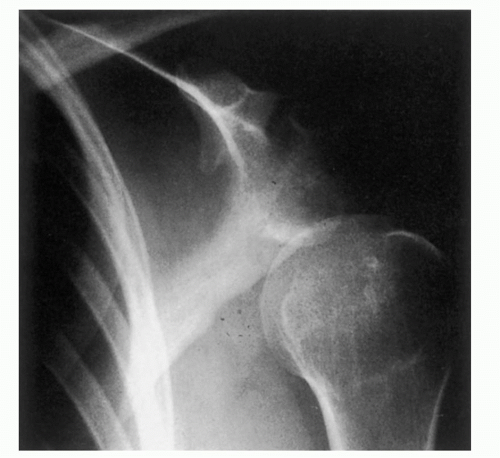
Failed Total Shoulder Arthroplasty
The author of this study has seen several patients who have had multiple unsuccessful shoulder arthroplasties. Although the results of shoulder arthroplasty are generally good, there are some patients in whom loosening, sepsis, and implant breakage occur. These patients often have severe loss of humeral and glenoid bone stock (Fig. 26-4). In this situation the surgeon must choose between attempting a repeat revision of the shoulder arthroplasty and reconstruction of the shoulder joint by arthrodesis. The results of revision total shoulder arthroplasty are suboptimal when compared with the results of primary arthroplasty. The decision between these two alternatives must be made on the basis of the patient’s age, the presence or absence of active sepsis, the bone stock that remains in the proximal humerus and glenoid, the symptoms the patient is experiencing, the quality and function of the rotator cuff and the deltoid, and the technical experience and expertise of the surgeon. In several patients who were significantly disabled the author has carried out glenohumeral arthrodesis following failed total shoulder arthroplasty and found it to be a helpful procedure for the patient. It is his belief that glenohumeral arthrodesis must be considered when the reconstructive surgeon is confronted with a patient with a history of multiple failed total shoulder arthroplasties.
Scalise and Iannotti reviewed seven patients who had arthrodesis following failed prosthetic shoulder arthroplasty. Four of the seven patients had undergone additional bonegrafting procedures in order to obtain union. The results of the study suggested that arthrodesis could achieve satisfactory clinical outcomes and that the patient should be aware of the frequent need for additional surgical procedures to obtain fusion.69 Conversely, Sperling and Cofield reported
their experience performing total shoulder arthroplasty after attempted shoulder arthrodesis in three patients.73
their experience performing total shoulder arthroplasty after attempted shoulder arthrodesis in three patients.73
Shoulder Instability
Virtually, all patients with shoulder instability can be treated by soft tissue or bony reconstructive procedures to stabilize the glenohumeral joint. Rarely, a patient will present with chronic shoulder instability after multiple attempts at surgical stabilization. If every surgical therapeutic alternative has been exhausted, the patient’s shoulder remains symptomatically unstable, and the patient does not wish to wear a thoracobrachial support, then arthrodesis can be indicated to restore shoulder stability. In this situation, careful assessment of the patient’s psychologic makeup must be carried out and one must be certain the patient has a full understanding of the implications of the procedure. Diaz et al. report arthrodesis to be a viable treatment option for this group of patients.20 The author considers arthrodesis for such patients if secondary osteoarthritic changes have begun to develop in the glenohumeral joint. These patients, however, may continue to experience problems and may not function at as high a level as other patients undergoing arthrodesis. Much has been written about the difficulties in managing such patients.55,63
Rotator Cuff Tear
Severe shoulder dysfunction can result from massive rotator cuff tears.23 Most rotator cuff tears can be managed by coracoacromial decompression and repair of the cuff. In patients who have massive rotator cuff tears that cannot be repaired, some authors have reported good results with debridement of the cuff tear and coracoacromial decompression.60 Longstanding rotator cuff tears can lead to cuff tear arthropathy as reported by Neer et al.49 This difficult pathologic entity can be treated by prosthetic arthroplasty with limited goals. Glenohumeral arthrodesis should be kept in mind as a possible alternative form of reconstruction in such patients when the technical skill of the surgeon or the available tissues do not permit cuff reconstruction and the patient is sufficiently symptomatic to exchange the loss of glenohumeral motion for the relief of pain. In author’s experience, this situation rarely, if ever, develops.
Malunion
Glenohumeral arthrodesis is rarely indicated for post-traumatic deformity. Most patients with post-traumatic deformities, such as osteonecrosis of the humeral head, chronic fracture dislocations, tuberosity impingement, and a malunion of the proximal humerus, are best treated by shoulder reconstruction using either osteotomy, arthroplasty, or a combination of both. If these procedures are not possible, then glenohumeral arthrodesis can be considered.
Osteoarthritis
The presence of glenohumeral osteoarthritis in an otherwise normal shoulder is an indication for total shoulder arthroplasty. However, almost all patients with glenohumeral osteoarthritis are of sufficient age that they are excellent candidates for total shoulder arthroplasty. If the patient were to develop osteoarthritis at a relatively young age, then glenohumeral arthrodesis might be considered,3 particularly if the patient was a laborer and modified work was not available to him or her. The results of total shoulder arthroplasty are so much superior that arthrodesis is rarely indicated for patients with this diagnosis.
Rheumatoid Arthritis
Patients with rheumatoid arthritis affecting the glenohumeral joint commonly have multiple problems in their upper extremity. Glenohumeral arthrodesis is recognized as a procedure that can decrease pain arising in the glenohumeral joint.32,53,67 Obliteration of glenohumeral motion has a negative influence on the upper extremity function. Frequently both upper extremities are involved. It is believed that patients with rheumatoid arthritis are much more effectively treated by total shoulder arthroplasty.25 Favorable reports of the combination of shoulder and elbow arthroplasty have appeared in the literature, and the author of this study would advocate this method of reconstruction for such patients.
CONTRAINDICATIONS TO GLENOHUMERAL ARTHRODESIS
Glenohumeral arthrodesis should not be performed if an alternative method of shoulder reconstruction is available. Many patients are amenable to arthroplastic reconstruction that preserves glenohumeral motion and has greater potential to restore function. Glenohumeral arthrodesis places a significant functional demand on the patient, requiring a major effort on
the part of the patient to rehabilitate the shoulder following surgery and to strengthen the thoracoscapular musculature. The procedure is contraindicated in a patient who cannot cooperate with such a program of rehabilitation. Similarly, the procedure is contraindicated in any patient with a progressive neurologic disorder who may experience paralysis or weakness of the trapezius, levator scapula, or serratus anterior. Glenohumeral arthrodesis relies on these muscles to motor the extremity, and significant weakness will grossly impair shoulder function following the procedure.
the part of the patient to rehabilitate the shoulder following surgery and to strengthen the thoracoscapular musculature. The procedure is contraindicated in a patient who cannot cooperate with such a program of rehabilitation. Similarly, the procedure is contraindicated in any patient with a progressive neurologic disorder who may experience paralysis or weakness of the trapezius, levator scapula, or serratus anterior. Glenohumeral arthrodesis relies on these muscles to motor the extremity, and significant weakness will grossly impair shoulder function following the procedure.
RESULTS
Review of Literature
Many techniques for glenohumeral arthrodesis have been reported. Some authors have used extra-articular arthrodesis, others have reported on methods of intra-articular arthrodesis, and still others have combined the two methods. In reviewing the literature, it is apparent that internal fixation has been employed more frequently in recent years. Historically, most authors have recommended external immobilization, although recently reports of glenohumeral arthrodesis without external immobilization have appeared.36,59 Now author of this study discusses extra-articular arthrodesis, intra-articular arthrodesis, the use of internal fixation, and the use of external fixators.
Extra-articular Arthrodesis
Extra-articular arthrodesis is primarily a historical procedure used before the antibiotic era to treat tuberculous arthritis. This treatment method was used to avoid entering the tuberculous joint and to obliterate motion at the joint without activating and spreading the infection. Watson-Jones78 described a technique utilizing a Cubbin’s approach16 to the shoulder, decorticating the superior and inferior surfaces of the acromion. A bone flap was then cut into the greater tuberosity and both the clavicle and the acromion were osteotomized. The arm was abducted and the acromion positioned to lie between the two edges of the bone flap in the proximal humerus. A spica cast was applied for 4 months.
Putti52 described a technique, whereby the spine of the scapula and the acromion were exposed subperiosteally. The spine of the scapula was detached; the acromion split, the medial and lateral portions, and the upper end of the humerus are exposed. The lateral surface of the humerus was split similar to the method described by Watson-Jones and the spine of the scapula was driven down into the humerus with the arm abducted. Spica cast immobilization was necessary following this procedure. Neither Watson-Jones’ nor Putti’s technique was truly extra-articular because the shoulder joint was usually entered when creating the split in the proximal humerus.
Brittain8 described a true extra-articular arthrodesis. This arthrodesis used a large tibial graft that was placed between the medial humerus and the axillary border of the scapula. The graft was maintained in position by its “arrow” shape (the pointed end was inserted into the humerus and the opposite, notched, end into the axillary border of the scapula). The graft was stabilized by its shape and adduction of the arm, which produced a compressive force along the long axis of the graft. DePalma18 reported that the failure rate of the arthrodesis was high owing to fracture of the long tibial graft.
Intra-articular Arthrodesis
Gill27 combined intra-articular and extra-articular arthrodesis. Gill used a U-shaped incision centered 2 cm below the acromion combined with a downward limb to the incision. Gill denuded the superior and inferior surface of the acromion and excised the rotator cuff. The glenoid fossa was decorticated as was the cartilaginous surface of the humeral head. An osseous flap was elevated from the anterolateral surface of the humerus, and a wedge-shaped slice of bone, with its base superiorly, was removed from the humerus. The arm was then abducted and impacted onto the acromion. The position was maintained by suture of the capsule and rotator cuff to the periosteum on the superior surface of the acromion. This technique is predicated on the assumption that it is desirable to fuse the glenohumeral joint in a large amount of abduction. This can be desirable in children when internal fixation is not used because, with time, the amount of abduction decreases. The technique is undesirable in adults owing to the likelihood of excessive abduction being retained following arthrodesis.
Makin41 reported on a method of glenohumeral arthrodesis in children that preserves the growth potential of the proximal humeral epiphysis. Makin fused the shoulder in 80 to 90 degrees of abduction, fixing the humerus to the glenoid with Steinman pins inserted first into the humerus in a proximal—distal direction and then driven in the reverse direction into the glenoid. Makin followed his children to adult life and noted that there was only a small loss in humeral length and no change in position of the fused shoulder. He recommended this technique, stating that this amount of abduction was necessary to maintain the growth potential of the proximal humeral epiphysis. The author has had no experience with this technique. If this amount of abduction was maintained, the shoulder would be dysfunctional in adulthood.
Moseley45 reported division of the rotator cuff insertion and excision of the intra-articular portion of the biceps tendon. Moseley advocated suture of the biceps tendon into the bicipital groove after division of its origin. This is an important step to remember in those patients who have functioning biceps, to avoid the unsightly cosmetic deformity identical with that seen in rupture of the long head of the biceps tendon. The author performs a biceps tenodesis during glenohumeral arthrodesis in all patients who have a functional biceps. Moseley denuded the inferior surface of the acromion as well as the articular cartilage of the humeral head and glenoid fossa. This is an important step in performing glenohumeral arthrodesis because the humeral head presents such a small area to the glenoid across which fusion can occur.
Beltran et al.7 performed glenohumeral arthrodesis through an anterior approach. They osteotomized the coracoid and created a tunnel that crossed the humerus and entered the glenoid cavity. They utilized a screw for internal fixation and in addition used a Cloward reamer to position a fibular graft from the proximal humerus into the infraglenoid area. Other techniques for glenohumeral arthrodesis have been described by May42 and Davis and Cottrell.17
Internal Fixation
A variety of methods of internal fixation have been advocated for glenohumeral arthrodesis. It is generally agreed that internal fixation is desirable because it maintains the position of the arthrodesis and can decrease the length of time so that
plaster immobilization is necessary to obtain an arthrodesis. Makin advocated the use of Steinman pins in children who are undergoing glenohumeral arthrodesis at an early age. Carroll9 reported on the use of a wire loop to maintain the position of glenohumeral arthrodesis. Carroll advocated the use of 22-gauge wire passed through the head of the humerus and the anterosuperior lip of the glenoid. He employed this method of arthrodesis in 15 patients, and all patients achieved solid bony union between the third and fourth month following surgery. Carroll noted that it was possible to manipulate the shoulder following surgery and change the position of the arthrodesis. As time has gone by, most authors have advocated more rigid forms of internal fixation. At present, few surgeons would use a wire loop as a method of internal fixation when performing glenohumeral arthrodesis.
plaster immobilization is necessary to obtain an arthrodesis. Makin advocated the use of Steinman pins in children who are undergoing glenohumeral arthrodesis at an early age. Carroll9 reported on the use of a wire loop to maintain the position of glenohumeral arthrodesis. Carroll advocated the use of 22-gauge wire passed through the head of the humerus and the anterosuperior lip of the glenoid. He employed this method of arthrodesis in 15 patients, and all patients achieved solid bony union between the third and fourth month following surgery. Carroll noted that it was possible to manipulate the shoulder following surgery and change the position of the arthrodesis. As time has gone by, most authors have advocated more rigid forms of internal fixation. At present, few surgeons would use a wire loop as a method of internal fixation when performing glenohumeral arthrodesis.
Other authors have reported the use of screws to obtain fixation during glenohumeral arthrodesis. May42 used a single stabilizing wood screw crossing the humerus and entering the glenoid fossa. Davis and Cottrell17 used a similar technique and added a muscle pedicle bone graft that was fixed in place with wood screws. Cofield and Briggs15 and Leffert38 also reported on the use of compression screw fixation without the use of a plate. Beltran7 developed a special fixation device using a screw bolt and washer to obtain glenohumeral arthrodesis. In addition, Beltran used an acromiohumeral screw and a fibular graft as methods of internal fixation.
The Association for Osteosynthesis (AO) group first advocated the use of plate fixation in 1970. They described this method of arthrodesis as not requiring supplementary plaster immobilization. The AO group advocated the use of two plates for internal fixation.46 The first plate was applied along the spine of the scapula and then bent down over the humerus, maintaining a position of 70 degrees of abduction between the vertebral border of the scapula and the humerus. The object of this position was to obtain a clinical position of 50 degrees of abduction, 40 degrees of internal rotation, and 25 degrees of flexion. They anchored this plate to the scapula with a long screw placed down through the plate and the acromion and into the neck of the glenoid (Fig. 26-5). They also noted that fixation could be improved by the insertion of two long screws inserted through the plate and the humeral head and into the glenoid. “If necessary,” a second plate applied posteriorly was advocated to improve the internal fixation. The author of this study has rarely found it necessary to use two plates when performing glenohumeral arthrodesis.
Kostuik and Schatzker36 have reported on the use of the ASIF technique. They did not use external immobilization postoperatively and reported good results in their patients. Riggins59 reported on shoulder fusion without external immobilization in 1976. Both the AO group and Riggins supplemented their arthrodeses with bone grafts. Riggins treated four patients with the use of a plate for internal fixation. Two of the patients had above-elbow amputations. The arthrodesis was successful in each case. Miller et al.43 analyzed five fixation techniques for shoulder arthrodesis biomechanically and found double-plate fixation to provide the highest bending and torsional stiffness in comparison to single-plate fixation, external fixation with screws, external fixation alone, and screws alone (techniques listed in decreasing level of stiffness). Ruhmann et al.65 found the strength of three humeroglenoid screws and three acromiohumeral screws to be similar to plate arthrodesis.
This author and his colleagues have reported on the results of a modified method of glenohumeral arthrodesis using internal fixation in 14 adult patients with brachial plexus palsy.58 We first used a single 4.5 AO/ASIF dynamic compression (DC) plate applied over the spine of the scapula onto the shaft of the humerus. We advocate placement of two cancellous compression screws passing through the plate and the proximal humerus into the glenoid first to achieve compression at the glenohumeral arthrodesis site. The plate is anchored to the scapula with a long screw passing through the spine of the scapula into the area of the coracoid base. Anchorage of the plate by this method, as opposed to the AO method, which inserts the screw into the glenoid neck, provides good fixation, yet leaves room for the large compression screws in the glenoid, which are felt to be more important in obtaining arthrodesis. Initially, we advocated the use of a postoperative spica cast because adult patients with brachial plexus injuries generally have significant osteoporosis, poor muscular control, and decreased proprioception, resulting from their neurologic injury. Bone grafts were not used in this series, and no nonunions occurred. More recently, we have begun to use thermoplastic thoracobrachial orthoses when performing glenohumeral arthrodesis and no longer use a spica cast (see the following discussion).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree