Abstract
Objectives
To evaluate the differences in gait characteristics and gait symmetry of post-polio syndrome (PPS) patients ambulating with or without shoes and between subgroups walking with different walking aids and orthoses, study the correlation of these data with personal data, illness condition, physical health, frequency of using aids and orthotics and frequency of falls, and derive recommendations for standardization of reporting these data.
Method
Twenty-six PPS subjects ambulated with their own walking devices. We calculated spatio-temporal parameters and symmetry indices (SI) of gait using a data acquired by a motion capture system. We compared inter-subject differences in gait pattern for PPS groups that differed by questionnaire-obtained data of demographics, physical activity, polio history, falls and walking aids. Additional inter-subject comparisons were performed between normal subjects ( n = 16), PPS patients walking with shoes with/without an ankle-foot-orthosis ( n = 11), PPS patients walking with knee-ankle-foot-orthosis ( n = 5), and PPS patients walking with a walker/crutches ( n = 10). We also compared intra-subject variability in PPS subjects who were able to repeat the trials barefoot.
Results
Our main results show that subjects who reported participating in physical activity twice a week or more had significantly better step time and double support symmetry. Subjects who use walking aids on a daily basis had significantly higher gait cadence and shorter stride time. Also, subjects that do not require knee-ankle-foot orthoses and/or walking aids walked with a smaller base width and better symmetry in stance and swing durations than PPS subjects who require these aids.
Conclusions
The gait pattern of PPS patients is related to numerous intrinsic and extrinsic factors. Standardization of the reporting protocol of gait-related data of PPS patients is crucial for patient evaluation and treatment design.
Résumé
Objectifs
Évaluer les différences des caractéristiques et de la symétrie de la démarche de patients syndrome post-polio (PPS) se déplaçant avec ou sans chaussures, dans des sous-groupes utilisant différents appareils et orthèses. Étudier la corrélation de ces éléments avec des données personnelles, le degré de sévérité de la maladie, la santé physique globale, la fréquence d’utilisation d’appareils et d’orthèses et la fréquence des chutes. En déduire des recommandations pour la standardisation de la collecte de ces données.
Méthode
Vingt-six patients PPS se sont déplacés grâce à leurs propres dispositifs d’aide à la marche. Nous avons calculé des paramètres spatio-temporels et des indices de symétrie (IS) de la démarche en nous servant d’informations obtenues par un système de capture de mouvements. Nous avons comparé les différences des schémas de marche entre les sujets répartis en différents groupes PPS en fonction d’éléments recueillis dans des questionnaires axés sur la démographie, l’activité physique, l’histoire de la polio, les chutes et les dispositifs d’aide à la marche. D’autres comparaisons inter-sujets ont été effectuées entres des sujets normaux ( n = 16), des patients PPS marchant avec des chaussures avec ou sans orthèse cheville-pied ( n = 11), des patients PPS marchant avec une orthèse genou-cheville-pied ( n = 5) et des patients PPS marchant avec un déambulateur ou des béquilles ( n = 10). Nous avons également comparé la variabilité intra-individuelle des sujets PPS en mesure de répéter les tests pieds nus.
Résultats
Nos résultats principaux montrent que les sujets ayant une activité physique au moins deux fois par semaine parviennent à un résultat significativement meilleur en terme de temps au bout duquel le pas suivant commence (step time/temps entre les pas) et de symétrie de double appui. Qui plus est, les sujets utilisant quotidiennement des dispositifs d’aide à la marche enregistrent une cadence de marche plus élevée et une foulée significativement plus basse. Enfin, les sujets dont la condition physique ne nécessite pas d’orthèse genou-cheville-pied ou de dispositif d’aide à la marche se déplacent avec moins d’écartement des piedset présentent un délai significativement plus court jusqu’au pas suivant et un double appui plus symétrique
Conclusion
Les schémas de marche de patients PPS dépendent de nombreux facteurs tant intrinsèques qu’extrinsèques. La standardisation des protocoles de collecte d’informations concernant la démarche des patients PPS est essentielle à l’évaluation des malades et à l’adaptation du traitement.
1
English version
1.1
Introduction
Post-polio syndrome (PPS) is a lower motor neuron disorder that affects survivors of paralytic poliomyelitis . The disorder emerges following a stable plateau phase lasting several decades after their recovery from the initial virus attack. Although new reported polio infections are quite rare owing to the polio eradication campaign initiated by the World Health Organization in 1988, there currently are more than 12 million individuals worldwide suffering from PPS. It is estimated that up to 80% of individuals who recovered from their acute poliomyelitis infection, report new neuromuscular complaints . Apart from psychological distress and joint pain , the main symptoms of PPS are progressive weakening of muscles, fatigue, and muscle atrophy .
Deterioration in motor abilities is frequently reported in PPS patients . The main impact of disability for most PPS patients is in mobility-related activities. Ambulatory individuals find it difficult to climb stairs, walk long distances, and perform various normal daily activities. Clinical management of PPS patients aims to restore mobility by means of physiotherapy, muscle training while avoiding overuse, surgical correction of joint deformities, or administration of orthoses and assistive devices . It has been suggested that biomechanical analysis of the PPS gait pattern can lead to optimal design of orthoses for PPS patients .
In light of the need to evaluate the gait characteristic of the PPS patient in order to devise the optimal treatment plan, quantifications of gait parameters may be warranted. Functional tools, e.g. the Timed “Up & Go” test are reliable tools, commonly used to evaluate gait performance . Unfortunately, these tools are not sensitive enough to provide precise quantifications of gait parameters. Therefore, quantitative spatio-temporal parameters are needed in order assess the effectiveness of gait, i.e. gait symmetry and thereby the patient’s risk of falling . Also, these parameters are frequently utilized for patient diagnosis, determining the severity of the patient’s condition, and predicting and monitoring the outcomes of an intervention .
Surprisingly, there is a great paucity in data describing gait of lower motor neuron disease including polio survivors. Importantly, what little data are available is usually lacking better description of the studied PPS group so that the discussion of the results and comparison between studies is compromised. Most studies of PPS gait differ mainly by the inclusion criteria concerning gait and the type of orthotics and walking aids used in the trials. Some of these studies fail to report these crucial data. We therefore aimed to:
- •
evaluate the differences in gait characteristics and gait symmetry of PPS patients ambulating with or without shoes and between subgroups walking with different walking aids and orthoses;
- •
study the correlation of these data with personal data, illness condition, physical health, frequency of using aids and orthotics and frequency of falls, and;
- •
derive recommendations for standardization of reporting of descriptive and quantitative data.
In order to reach these goals, we considered two variables as major outcome measures: barefoot/shod gait and type of walking aid/orthosis. Spatio-temporal parameters and gait symmetry were calculated in order to distinct between the different groups and conclude regarding the effectiveness of shoes and the variability of gait patterns in the different stages of the PPS. We further considered data of demographics, physical activity, polio history, falls and walking aids and its relation to the gait characteristics.
1.2
Methods
1.2.1
Subjects
We recruited 26 PPS out-patients (17 males and nine females; average age and standard deviation 57 ± 10.7 years old; height 164.5 ± 7.4 cm; weight 67.8 ± 10.4 kg; age at the time of initial illness 2 ± 1.6 years old). The PPS was verified according to the March of Dimes Criteria for clinical diagnosis of PPS and met the criteria of PPS according to Halstead . All of the participants demonstrated functional ability to ambulate with or without walking aids. We also tested a control group of 16 healthy subjects (10 females, six males; age 35.9 ± 11.9 years old; height 169.6 ± 4.5 cm). The trials were approved by a local Helsinki committee (approval number 0544-10-HMO). Each patient read and signed an informed consent form pretrial.
1.2.2
Trial protocol
We developed a motion capture-based protocol for acquiring spatio-temporal data. Four passive light-reflecting markers were placed bilaterally on the calcaneal tuberosity and the distal end of the second metatarsal or on their projection outward when shoes were worn. The motion of the patient was captured using a 4-camera system at a frequency of 120 Hz. All the subjects walked at a chosen comfortable velocity along a 5.5-m long marked path, several times. Each subject was then encouraged to try and walk without shoes if possible, and the trial was repeated. A ceiling-mounted safety harness was applied when a subject had difficulties maintaining balance during gait.
The subjects then answered a questionnaire regarding: gender, age, height, weight, age of initial poliomyelitis infection, childhood history (number of limbs with weakness, scoliosis, orthopaedic surgery, walking aids), marital status, education, physical health, exercise and its frequency during the last month, current walking aids, orthopaedic shoes, occasionally using a wheelchair, ability to ambulate at home and outdoors, number of falls indoors, number of falls outdoors or on stairs, and working in the last week.
1.2.3
Data processing
The 3D coordinates of the markers were calculated using a commercial software (Simi Motion, Germany). Initial contact and toe-off were marked manually using the video footage. A self-designed code (LabView 11, National Instruments, USA) was used to calculate spatio-temporal parameters ( Tables 1–3 ). Our code automatically calculates the Symmetry Index (SI) for the stance, swing, and double support durations, and the step length and base width according to the following equation :
where X L and X R are the values of a spatial or temporal parameter of the left and right leg, respectively. The SI ranges between ‘0’ for complete symmetry and ‘200’ for asymmetry.
| Orthopaedic surgery in childhood | Usage of walking aids on a daily basis | Physical activity more than twice a week | Falling indoors in the last 6 months | Occasionally using a wheelchair | |
|---|---|---|---|---|---|
| Velocity (m/s) | 0.148 | 0.054 | 0.971 | 0.016 | 0.056 |
| Cadence (steps/min) | 0.051 | 0.033 | 0.971 | 0.039 | 0.280 |
| Temporal data (s) | |||||
| Stride time | 0.097 | 0.028 | 0.971 | 0.039 | 0.251 |
| Step time | 0.060 | 0.108 | 0.971 | 0.046 | 0.251 |
| Stance duration | 0.216 | 0.108 | 0.971 | 0.028 | 0.156 |
| Swing duration | 0.169 | 0.033 | 0.857 | 0.305 | 0.378 |
| Double support | 0.488 | 0.196 | 0.491 | 0.039 | 0.199 |
| Single support | 0.148 | 0.028 | 0.801 | 0.277 | 0.415 |
| Temporal data (% GC) | |||||
| Step time | 0.869 | 0.108 | 0.227 | 0.829 | 0.494 |
| Stance duration | 0.869 | 0.324 | 0.914 | 0.096 | 0.923 |
| Swing duration | 0.530 | 0.790 | 0.325 | 0.072 | 0.721 |
| Double support | 0.575 | 0.700 | 0.491 | 0.072 | 0.626 |
| Single support | 0.869 | 0.533 | 0.403 | 0.053 | 0.626 |
| Spatial data (cm) | |||||
| Stride length | 0.621 | 0.295 | 0.857 | 0.039 | 0.047 |
| Step length | 0.668 | 0.268 | 0.971 | 0.033 | 0.047 |
| Base width | 0.006 | 0.324 | 0.538 | 0.053 | 0.056 |
| Foot progression (°) | 0.003 | 0.268 | 1.000 | 0.403 | 0.871 |
| SI | |||||
| Step time | 0.818 | 0.123 | 0.007 | 1.000 | 0.673 |
| Stance duration | 0.303 | 0.268 | 0.446 | 0.516 | 0.415 |
| Swing duration | 0.668 | 0.790 | 0.290 | 0.781 | 0.820 |
| Double support | 0.717 | 0.656 | 0.030 | 0.877 | 0.280 |
| Step length | 0.921 | 0.929 | 0.403 | 0.033 | 0.923 |
| Base width | 0.818 | 0.054 | 0.914 | 0.477 | 0.012 |
| PPS-BRF | PPS-SHOD | Z | P value | |
|---|---|---|---|---|
| Velocity (m/s) | 0.59 (0.19); 0.2–0.86 | 0.65 (0.21); 0.3–0.98 | −0.565 | 0.572 |
| Cadence (steps/min) | 91.1 (11.5); 67.9–108.8 | 90.7 (10.7); 75–110.8 | −0.031 | 0.975 |
| Temporal data (s) | ||||
| Stride time | 1.36 (0.18); 1.11–1.79 | 1.34 (0.16); 1.1–1.6 | −0.420 | 0.675 |
| Step time | 0.67 (0.09); 0.55–0.89 | 0.67 (0.08); 0.54–0.8 | −0.157 | 0.875 |
| Stance duration | 0.92 (0.17); 0.73–1.4 | 0.91 (0.11); 0.75–1.06 | −0.455 | 0.649 |
| Swing duration | 0.44 (0.08); 0.32–0.61 | 0.43 (0.08); 0.35–0.61 | −0.189 | 0.850 |
| Double support | 0.24 (0.11); 0.13–0.56 | 0.24 (0.06); 0.14–0.33 | −0.189 | 0.850 |
| Single support | 0.44 (0.09); 0.33–0.65 | 0.44 (0.08); 0.36–0.61 | −0.140 | 0.889 |
| Temporal data (% GC) | ||||
| Stance duration | 68.8 (5.0); 60.8–77.8 | 68.5 (3.7); 61.4–73.8 | −0.282 | 0.778 |
| Swing duration | 32.4 (5.2); 22.2–39.2 | 32.3 (3.7); 26.2–38.6 | −0.031 | 0.975 |
| Double support | 17.8 (6.0); 8.6–31.1 | 17.7 (3.7); 11.5–24.1 | −0.094 | 0.925 |
| Single support | 32.4 (6.2); 19.0–43.3 | 32.6 (3.8); 25.2–38.5 | −0.031 | 0.975 |
| Spatial data (cm) | ||||
| Stride length | 77.5 (20.9); 40.3–102.8 | 85.1 (24.5); 41.0–120.4 | −1.412 | 0.158 |
| Step length | 38.2 (10.8); 17.9–50.3 | 42.4 (12.2); 20.8–59.9 | −1.413 | 0.158 |
| Base width | 18.2 (5.3); 11.3–27.4 | 17.3 (7.3); 6.3–29.3 | −0.408 | 0.683 |
| Foot progression (°) | 11.6 (12.2); −4.7–32.7 | 8.5 (10.7); −8.9–23.9 | −1.036 | 0.300 |
| SI | ||||
| Step time | 20.1 (8.8); 1.9–32.4 | 13.2 (7.1); 1.1–28.3 | −1.852 | 0.064 |
| Stance duration | 14.6 (6.1); 6.3–27.5 | 10.7 (5.7); 3–22 | −1.664 | 0.096 |
| Swing duration | 34.4 (12.9); 13.8–53.7 | 20.7 (13.7); 5.3–48.2 | −2.668 | 0.008 |
| Double support | 26.4 (19.9); 2.2–71.4 | 24.9 (16.5); 6.5–54.3 | −0.282 | 0.778 |
| Step length | 30.9 (29.0); 1.8–108.6 | 23.0 (14.1); 1.6–43.4 | −0.973 | 0.331 |
| Base width | 9.4 (7.8); 0.1–28.6 | 16.1 (13.9); 0.4–51.1 | −1.538 | 0.124 |
| PPS-SHOES ( n = 11) | PPS-KAFO ( n = 5) | PPS-AID ( n = 10) | NORM ( n = 16) | P value | |
|---|---|---|---|---|---|
| Velocity (m/s) | 0.74 (0.14); 0.44–0.98 c,d | 0.42 (0.17); 0.3–0.72 d | 0.3 (0.26); 0.05–0.89 a,d | 1.09 (0.15); 0.8–1.31 a,b,c | 0.000 |
| Cadence (steps/min) | 91.7 (11.7); 75–110.8 c,d | 83.3 (8.4); 70.4–92.7 c,d | 50.0 (23.5); 11.1–90.3 a,b,d | 106.8 (9.0); 90.4–121.6 a,b,c | 0.000 |
| Temporal data (s) | |||||
| Stride time | 1.33 (0.17); 1.1–1.6 d | 1.45 (0.17); 1.3–1.73 | 3.4 (2.9); 1.3–11.1 | 1.1 (0.1); 1–1.3 a | 0.000 |
| Step time | 0.66 (0.09); 0.54–0.8 d | 0.73 (0.08); 0.65–0.85 d | 1.67 (1.41); 0.67–5.43 | 0.56 (0.05); 0.49–0.66 a,b | 0.000 |
| Stance duration | 0.88 (0.11); 0.75–1.05 d | 1.03 (0.16); 0.87–1.28 d | 2.69 (2.7); 0.77–9.84 | 0.69 (0.07); 0.59–0.85 a,b | 0.000 |
| Swing duration | 0.45 (0.08); 0.35–0.61 c | 0.42 (0.07); 0.36–0.53 c | 0.72 (0.23); 0.52–1.31 a,b,c | 0.43 (0.04); 0.34–0.51 c | 0.000 |
| Double support | 0.21 (0.04); 0.14–0.29 d | 0.31 (0.09); 0.17–0.43 | 0.99 (1.19); 0.11–4.03 | 0.13 (0.03); 0.09–0.18 a | 0.000 |
| Single support | 0.45 (0.08); 0.36–0.61 c | 0.42 (0.07); 0.36–0.53 c | 0.72 (0.23); 0.52–1.31 a,b,d | 0.43 (0.04); 0.34–0.51 c | 0.000 |
| Temporal data (% GC) | |||||
| Stance duration | 67.4 (3.4); 61.4–72.8 d | 71.7 (2.9); 66.9–74.1 d | 74.3 (7.5); 65–88 d | 61.8 (1.7); 59.1–65.5 a,b,c | 0.000 |
| Swing duration | 33.6 (3.0); 30.1–38.6 d | 29.1 (4.7); 25.9–37.3 | 27.0 (8.9); 12–39.9 d | 38.2 (1.7); 34.6–40.9 a,c | 0.000 |
| Double support | 16.4 (3.0); 11.5–21.3 d | 20.4 (5.7); 10.7–24.6 | 25.2 (11.3); 10.1–46.5 d | 11.7 (1.7); 8.75–14.64 a,c | 0.000 |
| Single support | 34.0 (2.7); 30.4–38.5 d | 29.3 (5.5); 25.2–38.8 | 26.4 (8.7); 11.6–38.2 d | 38.1 (2.0); 34.6–41.5 a,c | 0.000 |
| Spatial data (cm) | |||||
| Stride length | 95.6 (14.7); 68.4–120.4 d | 61.2 (23.9); 41.0–101.3 d | 65.6 (27.5); 33.1–116.8 d | 123.0 (10.9); 107.0–144.1 a,b,c | 0.000 |
| Step length | 47.6 (7.5); 33.1–59.9 c,d | 30.6 (12.1); 20.8–51.1 d | 31.6 (14.2); 18.2–59.4 a,d | 60.8 (5.0); 53.2–69.4 a,b,c | 0.000 |
| Base width | 14.9 (6.2); 6.3–27.5 b | 24.3 (4.5); 17.3–29.3 a,d | 21.1 (9.4); 5.6–35.7 d | 10.6 (3.3); 6.5–20.1 b,c | 0.001 |
| Foot progression (°) | 10.8 (9.5); −4.9–23.9 | 5.5 (12.1); −8.9–18.3 | 7.1 (10.3); −10.9–26.1 | 6.5 (3.2); 1.2–13.3 | 0.447 |
| SI | |||||
| Step time | 11.5 (5.6); 1.1–21.3 d | 19.4 (12.2); 5.2–33.6 | 61.3 (62.3); 4.2–219.7 | 4.1 (2.8); 0.2–11.2 a | 0.000 |
| Stance duration | 9.2 (5.3); 3.0–22.0 b,d | 17.7 (3.9); 12.4–23.3 a,d | 11.8 (12.2); 0.1–38 | 2.6 (1.6); 0.5–6.8 a,b | 0.000 |
| Swing duration | 14.8 (7.3); 5.3–26 b,d | 46.2 (8.4); 36.8–59.3 a,d | 36.5 (42.1); 9.5–151.6 | 4.0 (3.6); 0.7–11.8 a,b | 0.000 |
| Double support | 27.3 (17.6); 6.5–54.3 | 22.0 (12.4); 11.2–41.5 | 121.2 (143.7); 5–450.6 | 10.9 (9.6); 0–36.1 | 0.001 |
| Step length | 22.0 (15.0); 1.6–43.4 d | 20.2 (13.1); 4.2–39.5 | 117.3 (145.8); 0.4–481.5 | 5.1 (4.2); 0.1–13.4 a | 0.000 |
| Base width | 19.3 (13.9); 3.2–51.1 | 7.7 (6.9); 0.4–17.5 | 13.3 (7.4); 1.3–25.6 | 16.8 (15.8); 0.6–52.8 | 0.347 |
a Statistically significant difference compared to PPS-SHOE.
b Statistically significant difference compared to PPS-KAFO.
c Statistically significant difference compared to PPS-AID.
1.2.4
Statistical analyses
Statistical analyses were performed using SPSS 13.0 (SPSS Chicago, IL, USA). The Mann-Whitney U test was used to evaluate the differences in spatio-temporal parameters and SI for PPS groups that differed by their answers to the questionnaire. Next, we compared a subgroup of 14 PPS patients who were able to repeat the trials of shod gait with or without orthotics and walking aids (PPS-SHOD) and were able to perform the trial again barefoot (PPS-BRF) using the Wilcoxon 2-related samples test. We then compared results of four groups: normal subjects walking without shoes (NORM; n = 16), PPS patients walking with shoes and with or without ankle-foot-orthosis (AFO; study group labeled PPS-SHOE; n = 11), PPS patients walking with knee-ankle-foot-orthosis (KAFO; PPS-KAFO; n = 5), and PPS patients walking with either a walker or crutches in addition to orthotics and shoes (PPS-AID; n = 10). The Kruskal-Wallis test was conducted to compare the effect of shoes, orthotics and walking aids on the spatio-temporal and SI data. We applied the Tamhane post-hoc test to determine which groups differed with regard to their walking aids. P < 0.05 was considered statistically significant.
1.3
Results
We found no difference in gait parameters in PPS sub-groups that differed by gender (male or female), age (above or below 60 years old), body mass index (BMI < 25 or BMI ≤ 25), age of initial poliomyelitis infection (< 2 or ≥ 2 years old), childhood history of weakness in number of limbs (both legs involved or not), walking aids in childhood (yes/no), scoliosis at initial illness (yes/no), education (above or below 12 years), marital status (married or not), perceived physical health (feel healthy or not), exercise during the last month (yes/no), orthopaedic shoes (yes/no), ability to ambulate at home and outdoors (yes with or without difficulty or with aids or assistance or cannot walk), falling outdoors in the last 6 month (yes/no), and working in the last week (yes/no). We did, however, find a connection between several spatio-temporal gait parameters and questionnaire-based subgroups ( Table 1 ). Specifically, PPS subjects who are not using walking aids on a daily basis had significantly higher gait cadence and shorter stride time. Their gait velocity was higher when compared to subjects who did use walking devices on a daily basis, average velocity of 0.673 m/s and 0.454 m/s, respectively, however the difference was not statistically significant. PPS subjects who reported participation in physical activity more than twice a week had better step time and double support symmetry. PPS subjects who did not report falling indoors in the last 6 months had significantly higher gait velocity and cadence, shorter double support stance and step durations, as well as longer step length and better step length SI. PPS subjects who are not using a wheelchair walked with significantly longer step length and had less symmetry of their base width, however only one of these subjects had SI of base width that was above normal. Finally, PPS subjects who went through orthopaedic surgery in childhood walked with a smaller than normal foot progression angle and had significantly wider base width.
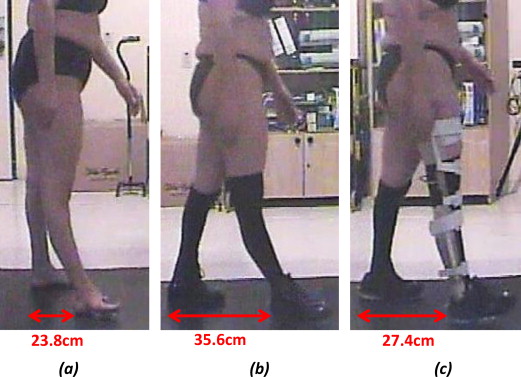
The results of intra-subject variability of 14 PPS patients who were able to perform the test with (PPS-SHOD) and without (PPS-BRF) their shoes, orthotics and walking aids are presented in Table 2 . Although the mean gait velocity was increased from 0.59 m/s for PPS-BRF to 0.65 m/s for PPS-SHOD, the difference was not statistically significant ( P = 0.572; Table 2 ). Among the 14 PPS subjects, only nine walked faster wearing their shoes and orthotics. A similar finding concerns the mean stride length increase from 77.5 cm for PPS-BRF to 85.1 cm for PPS-SHOD ( Table 2 ). Although 11 subjects increased their stride length, the results were insignificant ( P = 0.158). An example for the difference in step lengths when ambulating barefoot, with shoes, and with orthotics is depicted in Fig. 1 . In this figure, sagittal images of a 43-year-old female PPS patient who ambulated without shoes ( Fig. 1 a), with orthopaedic shoes ( Fig. 1 b) and with KAFO ( Fig. 1 c) are presented at the time of right foot heel strike. The step length of the subject was short when she ambulated without shoes and genu recurvatum of the right leg can be seen. When walking with her orthopaedic shoes, the patient increased her step length by 11.8 cm and when donning the KAFO, the hyperextension of the knee is prevented, however the orthosis imposes a decrease in step length to only 3.6 cm longer than the step length achieved while walking without shoes. All temporal-related SIs decreased when shoes and orthotics were used in the trials ( Table 2 ). The decrease in SI of the swing duration was statistically significant ( P < 0.01).
When comparing the gait characteristics of PPS patients walking with shoes, with or without AFO (PPS-SHOES), with shoes and KAFO (PPS-KAFO), with shoes, orthotics and wither a walker or crutches (PPS-AIDS) and normal gait (NORM), we found significant differences for most of the spatio-temporal parameters of gait and SIs ( Table 3 ). As could be expected, the normal gait was characterized by higher velocity and cadence, shorter stance duration, longer stride and step lengths. These parameters differed statistically for the NORM group when compared to the three PPS groups ( Table 3 ). Other characteristic of normal gait were smaller base width), longer single support duration, and better SI, however the statistical significance was found interchangeably for one or two of the PPS groups ( Table 3 ).
The PPS-SHOES group walked with a smaller base width and better symmetry in stance and swing durations when compared to the PPS-KAFO group. They also walked with a higher velocity and cadence, longer stride length and single support duration, however these findings were not found to be statistically significant ( Table 3 ).
The PPS-AID group was characterized by the slowest gait velocity, reduced cadence, long stride time, stance and double support duration, short swing and single support durations, short step length and high SIs. The variability and range of SIs for the PPS-AID was very high.
1.4
Discussion
PPS patients exhibit decreased functional ability, mainly impaired due to gait deficiencies. In addition to the custom functional, clinical and electro-physiological examinations, computational gait analysis provides further insight into the motor function and control of the patient. In this study, we compared spatio-temporal data and gait symmetry of PPS patients ambulating barefoot, with shoes, with orthotics and walking aids and compared them to normal gait. The necessity of exploring these differences arose from the great paucity in data describing the gait of PPS patients and more importantly, the lack of uniformity in reporting the personal characteristics of the study group and the conditions of the trials, compromising the conclusions of comparisons made between different studies of PPS gait.
In our study, the gait pattern of the PPS subjects was not associated with gender, age, BMI, education, and marital status. Also, apart from association with history of orthopaedic surgery at childhood, no correlation was found between gait characteristics and polio history. Most of the subjects (76.9%) went through corrective orthopaedic surgery at childhood and walked with a significantly smaller than normal foot progression angle and had significantly wider base width. This finding may suggest that altered tendon length at the ankle joints and ankle/foot arthrodesis caused alteration of ankle/foot progression bio-mechanical mechanism, thereby compelling the subject to increase his or her base width to maintain stability and to compensate the lack of bio-mechanical rockers.
The physical health of PPS patients affects their daily activities and participation in the community . In this study, we found that subjects who reported participating in physical activity twice a week or more had significantly better step time and double support symmetry, i.e. lower SI. Gait symmetry and gait double support duration were shown to be the variables most strongly associated with prediction of multiple fallers , and we found correlation between reports of falling indoors in the last 6 months and significantly reduced gait velocity and cadence, longer double support stance and step durations, as well as shorter step length and higher step length SI, indicating high asymmetry. These findings suggest that PPS fallers reduce their gait cadence and maintain double support for longer and uncertain distances and likely use walking aids in order to increase their stability and reduce the risk of falling. These taken precautions cost them their velocity of advancing forward as their step length is reduced.
Walking aids and orthopaedic shoes are an integral part in the life of a PPS patient. The deterioration of the motor condition of the PPS patient involves increasing the need of walking aids and orthotics. Although the symptoms of the syndrome vary for each individual, the typical cluster of symptoms comprises mainly of a gradual increase in muscle weakness, particularly but not exclusive to the muscles injured in the initial virus attack. This condition reduces the control of the patient over his or her joints. Following this first stage of the appearance of the symptoms, the patient will adopt certain motor mechanisms that will compensate for the muscle weakness and allow the PPS patient to continue with daily activities. Since gait asymmetry is now a daily routine in the life of the patient, it imposes alteration of the state of loadbearing on the joints, caused by instability of the joints and prolonged loadbearing on the preferred side, or secondary biomechanical changes. Consequently, joint pain often arises. Coupled with muscle pain as part of the PPS, antalgic gait is common and the gait pattern is affected. At this stage, most patients will require new walking aids and/or orthotics, to be used on a daily basis. These aids will usually restore joint stability, thereby reducing joint pain, allowing the patients to walk longer distances without fatiguing and prevent joint pain.
In this study we found that subjects who use walking aids on a daily basis (69.2%) had significantly higher gait cadence and shorter stride time. Their gait velocity and spatial gait parameters did not significantly differ from subjects who did not use walking aids on a daily basis, although the gait velocity was lower in subjects who daily used walking aids. In an attempt to maintain a high gait velocity, PPS patients who depend on assistive devices increase their cadence. At progressive stages of the PPS, the patient will be less able to walk independently without fatiguing and will resort to using a wheelchair. In our study, although we included only subjects that had functional walking ability with or without walking aids, 26.1% of the subjects reported occasionally using a wheelchair. These subjects had significantly shorter step length, since their physical status was more deteriorated.
When comparing gait characteristics of PPS patients walking with their customary shoes and orthotics and walking barefoot, we found no statistically significant differences, excluding the SI of the swing duration, which was improved for shod gait ( Table 1 ). Although most of the subjects walked faster and increased their stride length during shod gait, the results were not statistically significant. These results suggest that the PPS patients adopt a certain gait pattern, which allows them to optimally compensate for muscle weakness and atrophy, and enables a comfortable gait so that when the shoes and orthotics are doffed, only slight changes in the gait characteristics appear. This conclusion, however, does not imply that the gait pattern of the PPS patient cannot be altered by replacing existing orthotic or walking aid with a new one, but that the patient will require time to acquaint himself or herself with the new restrictions or and liberties provided by the replaced orthotic or aid.
Walking aids and orthotics are prescribed to PPS patients to improve balance during the stance phase and ensure foot clearance in the swing phase so that the risk of falling is minimized. The walking aids also improve endurance, relieve pain and prevent further deterioration of joint degradation . The use of orthopaedic shoes, AFO, KAFO, crutches and walkers, alters the gait pattern by controlling the interaction properties between the shoe and the ground, or decreasing the range of motion of the ankle and knee joints. Although these compensation strategies may enable the patients to make the most of their residual capacities and keep their mobility, in the long term, these strategies can induce joint degeneration .
We found that when compared to normal gait pattern, PPS inter-subject variability was greater and significant differences were evident in most of the spatio-temporal parameters and SIs ( Table 3 ). Our results show that PPS gait is characterized by slower velocity and cadence, prolonged stance duration, and shorter step lengths. Prolonging the stance duration from the mean normal value of 61.8% to mean values of 67.4%, 71.7%, and 74.3% for the PPS-SHOES, PPS-KAFO, and PPS-AID, respectively, was accompanied by shorter swing and single support durations and longer double support duration ( Table 3 ). These temporal data suggest that the subjects felt imbalanced in swinging the leg forward, thereby transferring their entire body load to the other leg. This insecurity relates to the weakness of the muscles that control the body posture and joint stability during load bearing activities and prevent falling.
PPS patients walking with shoes with or without AFO had a smaller base width and better symmetry in stance and swing durations when compared to the PPS patients ambulating with KAFO ( Table 3 ). The locked KAFO is usually prescribed to patients whose symptoms are progressed so that their knee extensors are weak and is crucial for knee stabilization. However, maneuvering with a locked knee unilaterally is designated to produces gait asymmetry. We presented a visual example of the effects of shoes and KAFO on the step length and knee angle in a PPS patient ( Fig. 1 ). This subject has been using the KAFO for the realignment of the femur and tibia. Realignment of limb segment may prove to be harmful as some of the patient’s deformities and compensations are beneficial to produce functional gait . Therefore, the choice for prescribing a certain type of orthosis and adjusting its parameters of function can critically affect the gait pattern of the patient. Most orthotics prescribed to PPS patients are KAFO, designed to lock the unstable knee joint , therefore augmenting stability during gait. Since the patient cannot flex the knee during swing, this result in compensation in the form of circumduction, vaulting or hip hiking or a combination of these. The design of the stance-control orthosis (SCO) locks the knee during load-bearing state and unlocks during non-load bearing state. Studies have shown that PPS patients walk faster while ambulating with an SCO than with a locked KAFO .
PPS patients who require the assistance of a walker or crutches in addition to orthopaedic shoes and/or orthotics are patients whose gait is the most restricted and affected by their deteriorating condition. Accordingly, the gait of these patients who participated in this study, was characterized by the an extremely slow gait velocity, reduced cadence, long stride time, stance and double support durations, short swing and single support durations, short step length and high SIs. The variability and range of SIs for the PPS-AID was very high.
The main limitation of our study is the small sample group; however we were able to show the differences in gait pattern, obviously from normal gait, but more interestingly between sub-groups ambulating with different orthotics and aids. A study of larger population, where PPS patients are divided into groups according to more specific device types will shed more light on the consequences of prescribing certain orthotics or aids. The presented data herein may already provide the basis for understanding some of the factors, which may link spatio-temporal parameters, gait symmetry, and the progress of the PPS. Another limitation is the single-day measurements that may not be representative of the general gait pattern.
Following the conclusions presented herein, we recommend standardization of the reporting protocol of gait-related data of PPS patients. Studies are usually recruiting small PPS groups, which, as shown herein, have great inter-subject variability so that it is important to present all the personal characteristics that differ between subjects. The specific inclusion criteria relating to diagnosis of PPS and motor abilities at the time of recruitment should be addressed. Also, researchers should provide specific details of orthoses and walking aids used by their subjects and note whether the trial protocol was such that the subject ambulated with their own footwear and aids. Since gait laboratories are equipped with different hardware and software, using different calculation algorithm, and different trial protocols, we believe that following the aforementioned guidelines will reduce the difficulty of comparing results between studies.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
We appreciate the help of Hadassah physiotherapists Asaf Frechtel, Yael Bresler, Yshai Peleg, Adina Forst, and Shira Eisenberg, with the data collection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





