Fractures and Dislocations of the Metacarpals and Phalanges
General Information
Metacarpal and phalangeal fractures are common skeletal injuries that are classified by the pattern of the fracture and the condition of the skin and soft tissues. High-energy injuries cause bone comminution and soft-tissue injury, which adversely affects outcome. This mechanism of injury creates displaced and unstable fractures that often require fracture fixation. In contrast, low-energy injuries cause less damage to the bone and soft-tissue envelope, which makes them more amenable to nonsurgical treatment. The goal of treatment for metacarpal and/or phalangeal fractures is to maintain skeletal length and alignment and restore joint motion.
Diagnostic Criteria
History
A diagnosis of fracture is made by clinical observation confirmed by radiographic findings. The history is important and should include specific details about the amount of force and direction of impact.
Physical Examination
Hand fractures are characterized by pain at the site of fracture, edema, and ecchymoses.
Careful examination of fracture alignment is essential. The finger must be examined both in extension and flexion to detect rotational malalignment. A malrotated finger often appears to be normal in extension, but shows considerable angulation or rotation when examined in flexion (Fig. 1). Comparison
of the digital cascade between the injured and uninjured hand is also helpful (Fig. 2).
of the digital cascade between the injured and uninjured hand is also helpful (Fig. 2).
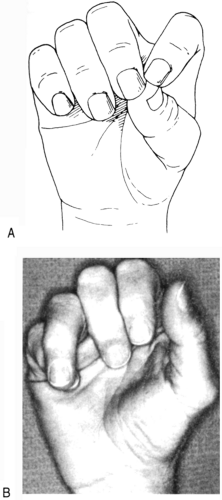 FIG. 2. A: When the digit is flexed, the deformity is quite apparent. B: Active finger flexion generates malrotation of ring finger with digital overlapping. |
The examination of the fractured extremity should be comprehensive. A notation about the soft tissues is necessary, including the ligamentous stability, tendon integrity, skin condition, vascular supply, and neurologic condition.
Radiographic Assessment
Anteroposterior and lateral x-rays are required to determine the pattern of fracture. The injury site should be centered on the radiographic cassette. Lateral x-rays of the digits can be difficult to obtain. To acquire a more accurate lateral view of the injured finger, one should raise it away from the rest of the digits or rotate the hand. Advanced imaging modalities (e.g., computed tomography [CT] or magnetic resonance imaging [MRI]) are not necessary for initial fracture evaluation.
Table 1. Clear descriptors for metacarpal and phalangeal fractures | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Communicating About Fractures
When discussing fractures with colleagues, one should use unambiguous terms with precise meaning. Describing fractures by using traditional fracture classification systems and fracture eponyms has significant problems. Fracture classification systems often are associated with significant rates of interobserver error, do not direct treatment, and are not predictive of outcome. Rather than using fracture eponyms and classification systems, it is better to use basic terms that clearly describe the injury. First, one should describe the location of the injury by identifying the fractured bone and the location of the injury within the bone (intraarticular or extraarticular). Second, one should define the fracture as simple (single fracture line) or comminuted (multiple fracture lines). Third, one should determine whether the fracture is displaced or not displaced and measure the amount of displacement and angulation between the two fracture ends (Table 1). Finally, one must communicate the status of the soft-tissue injury or other circumstance that may affect the treatment pathway.
Determination of Fracture Healing
Fracture healing is determined by clinical and radiographic criteria. A fracture site that is nontender is healed enough to allow active digital range of motion. Most fractures treated by nonoperative methods heal by the formation of callus at the fracture site (secondary bone healing). An early radiographic sign of union is fracture “callus” that bridges the bone ends. Later the callus will organize and “bridging trabeculae” of more mature bone will be seen crossing the site of fracture. Fractures that are treated with rigid plate fixation may undergo a different kind of bone healing (primary bone union) that heals with very little or no callus formation. In general, radiographic findings lag well behind clinical findings.
Nondisplaced Fractures or Stable Injuries
Stable, nondisplaced, closed metacarpal and phalangeal fractures are immobilized in a functional position for 10 to 14 days. The patient is then begun on a
program to restore active range of motion (Tables 2 and 3). Hand immobilization must resist the muscular forces that may cause the fracture to displace and place the joints in their “best” position. The intrinsic muscles are the primary deforming forces in most metacarpal and proximal phalanx fractures. These muscles bend the fractured metacarpal into an apex dorsal angulation and the fractured proximal phalanx into an apex volar angulation (Fig. 3). To keep the ligamentous structures of the metacarpophalangeal (MCP) joint at their maximum length, these joints should be immobilized in 50 to 70 degrees of flexion
(otherwise, they are prone to develop an extension contracture). In contrast, the interphalangeal joints are prone to develop flexion contractures. To keep the ligaments of the interphalangeal joints stretched to their maximum length, these joints should be positioned in extension. Fortunately, this position of MCP flexion and interphalangeal joint extension (i.e., the intrinsic plus position) both relaxes the intrinsic muscles and places the joints in a desirable position.
program to restore active range of motion (Tables 2 and 3). Hand immobilization must resist the muscular forces that may cause the fracture to displace and place the joints in their “best” position. The intrinsic muscles are the primary deforming forces in most metacarpal and proximal phalanx fractures. These muscles bend the fractured metacarpal into an apex dorsal angulation and the fractured proximal phalanx into an apex volar angulation (Fig. 3). To keep the ligamentous structures of the metacarpophalangeal (MCP) joint at their maximum length, these joints should be immobilized in 50 to 70 degrees of flexion
(otherwise, they are prone to develop an extension contracture). In contrast, the interphalangeal joints are prone to develop flexion contractures. To keep the ligaments of the interphalangeal joints stretched to their maximum length, these joints should be positioned in extension. Fortunately, this position of MCP flexion and interphalangeal joint extension (i.e., the intrinsic plus position) both relaxes the intrinsic muscles and places the joints in a desirable position.
Table 3. General principles of initial fracture management | |
|---|---|
|
Displaced Fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










