Foot and Toes
Katherine L. Dec
Foot and toe injuries can limit the functions of the athlete in any weight-bearing sport. True incidence in the athletic population can be difficult to ascertain because of the tendency to self-treat and minimize the injury. Incidence of injury in the foot appears to be greater in older athletes than in younger athletes (1). In this study, a greater number of plantar fasciitis and metatarsalgia injuries were noted compared to all other foot injuries reviewed. Interestingly, this particular anatomical area of the body is treated and advice administered by both medical and allied health providers. Sports medicine physicians, podiatrists, orthopedic surgeons with subspecialty training in foot and ankle and shoe salespeople all treat the foot.
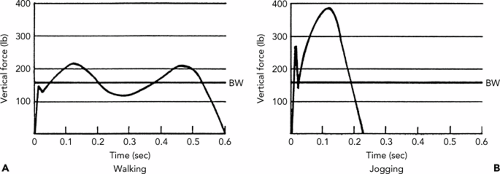
The foot forms the base of support for the entire body in any gravity-controlled situation. Standing, walking, running, or cycling requires the foot to transfer the mechanical power of the legs to the ground for locomotion and to dissipate the forces generated by ground–body interaction (see Figure 33.1). Forces dissipate at three sites with three different actions: knee flexion, ankle dorsiflexion, and subtalar pronation. The foot is adaptable, being both rigid and flexible in different parts of the gait cycle. It is rigid with transfer of power from the lower extremity to the surface, and flexible when responding to changing surface characteristics. There are many demands upon the foot: (a) it must absorb shear loads with sudden stops/starts, (b) absorb the shock with the push-off and landing impact sustained in jumping, (c) bear continuous loads with lifting and standing, and (d) assume repetitive loads when walking or running.
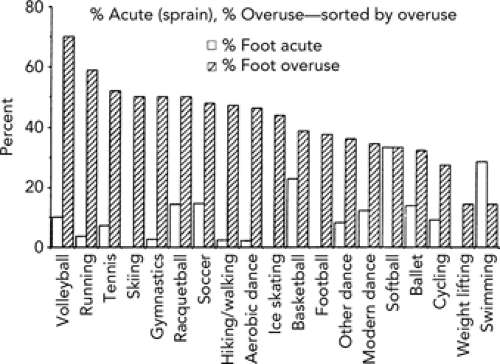
During running, the foot sustains approximately 1.6 to 2.3 times body weight impact in the stance phase (2). On landing from a jump, usually on the forefoot, it is estimated that 4.1 times body weight impact is sustained (3). Nigg (4) has suggested that impact force factor is more of an issue in the muscle tuning/balancing of effort in effecting a change in the foot than the amount of the force. Waller (5) has proposed that the foot and structures deep within it are merely part of a chain linkage system and that a problem with any link in the system can cause imbalance in another segment. The secondarily affected system may actually be more symptomatic than the primary site of involvement. Most sports require running, either in conditioning or as an integral part of the sport. Jogging and running generate the most stress to the foot (6). Garrick and Requa (7) have also taken a good epidemiological look at foot injuries caused by sport, differentiating between acute versus overuse types (see Figure 33.2).
Anatomy
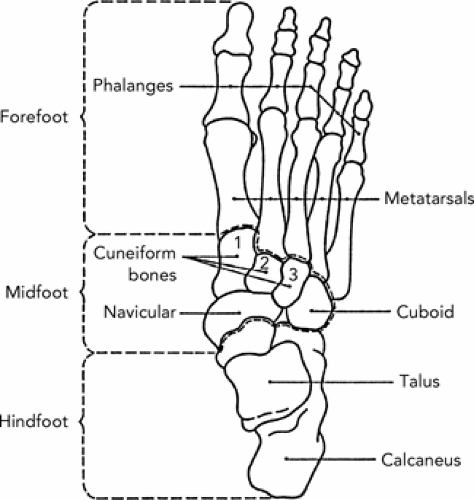
The foot is made up of 28 bones and 57 joints. The bones are distributed in three segments (see Figure 33.3): (a) hindfoot or heel—talus and calcaneus; (b) midfoot—navicular, cuboid, and cuneiform bones; and (c) forefoot—metatarsals, phalangeal bones, and a pair of sesamoid bones. The joint between the hindfoot and midfoot is also called Chopart’s joint; the joint between midfoot and forefoot is Lisfranc’s joint. The medial portion of the calcaneus has a shelf-like piece called the sustentaculum tali. Innervation of the foot comes from the tibial, saphenous, sural, superficial and deep peroneal nerves. There can also be accessory bones, typically termed os, in the foot without biomechanical significance.
The foot has several planes of motion due to the structure of the ankle joint and talus. Typical range of motion (ROM) in a “normal” foot is 45 degrees plantar flexion, 20 degrees dorsiflexion, 30 degrees inversion, 20 degrees eversion, 20 degrees internal rotation, and 10 degrees external rotation.
X-rays. Typically three views are necessary to adequately see foot fractures/dislocations. Standard views are anteroposterior (AP), lateral, and oblique.
Consultation/evaluation. Please see an example protocol in Appendix 1 (8) that can be used as an office note.
Aspects of the history and physical examination are summarized here:
History
Date of injury—acute or gradual in onset?
What activity/sports causes symptoms?
Location of symptoms?
Any previous treatment, including change in footwear and orthotics (off the shelf or prescriptive)?
Training factors. Surface, intensity, and frequency, time during training when symptoms occur, incline or decline of surface.
Medical history. Any prior foot surgeries, injections, osteoporosis, (in females, the female athlete triad) or rheumatoid disease involving the foot (i.e., gout, Reiter’s syndrome, rheumatoid arthritis).
Further questions addressing the lower kinetic chain include the following:
Any surgeries or injuries to the ankle, leg, knee, hip or back? (When mechanics are considered for the lower extremity, the lumbosacral junction through the foot is considered as one unit, as adaptations are made in muscles/joints to maintain stability of the extremity during weight bearing.)
Family history of rheumatoid disease, neuromuscular disorder (i.e., hereditary motor sensory neuropathy [HMSN]), or osteoporosis are important.
Physical examination (done in non–weight bearing and weight bearing includes) the following:
Inspection of the foot. Effusion, ecchymosis, callus pattern, corn, wart, blisters; deformity (i.e., hammer toe); posture, foot position.
If shoes present, inspection of shoes. Check wear pattern; and if orthotics used, how they fit in weight bearing.
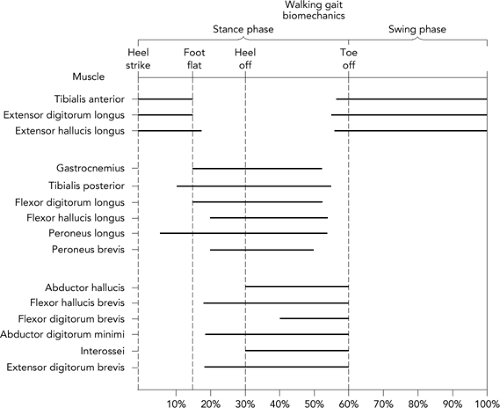
Gait pattern (see Figure 33.4). Lengthy discussions on clinical biomechanics for lower extremity exist in other texts. Focus primarily on movement of the foot, ankle, knee, hip, and pelvis during the heel strike to toe-off part of the cycle. This includes observing the pelvic rotation and list (4 degrees and 5 degrees respectively, on each side), knee flexion moment at stance, and displacement of trunk at toe-off and midstance.
Pelvic/spinal abnormalities. Static testing in standing and supine/prone.
Lower limb abnormalities. Static testing in supine/prone.
Leg length measurement.
ROM. Including first metatarsal-phalangeal (MTP) in ankle dorsiflexion and at rest; also passive midfoot and rearfoot ROM.
Heel examination.
Midfoot examination.
Forefoot examination.
Sensory examination, including assessment for upper motor neuron findings (i.e., clonus and Babinski test).
Biomechanics are important in foot/toe injuries both in how their injury affects the rest of the leg and how the resultant healing affects the rest of the leg. Figures 33.4 and 33.5 outline muscle involvement during walking and running cycle (for foot and lower leg musculature). For example, at heel strike there is eccentric contraction of the quadriceps and anterior tibialis; treatment for tendinitis of the anterior tibialis considers function of the quadriceps, ROM of the foot and ankle, and positioning of the calcaneus.
Any treatment that involves the proximal joints of the lower extremity can affect the biomechanics of the foot (8)a. Core trunk and proximal lower extremity muscles and joints can be more important as speed of gait changes. Neptune et al. (9) note that the gluteus muscles are critical in body support before plantar flexors become active in early stance phase. It is important to consider this relationship, between the foot and the rest of the body biomechanics, when formulating rehabilitation programs for resuming the sport.
Hindfoot
Anatomy. The talus sits on top of the calcaneus and forms the subtalar joint. This joint contributes to
the ROM in the hind foot. The joint is stabilized by the extrinsic lower leg muscles and intrinsic foot muscles. Anteriorly, the border between the hindfoot and midfoot is the transverse tarsal joint. This joint allows the midfoot to rotate for terrain adaptation. The subtalar joint is flexible in pronation but rigid in supination. Note that the biomechanics may explain why a pronated foot is better tolerated in running than a supinated one. Posteriorly, the Achilles tendon inserts on the posterior aspect of the calcaneus, at which point it becomes thinner, with its fibers sweeping underneath the posterior inferior aspect of the heel, and then continuing forward as the plantar fascia to insert on the metatarsal heads and proximal toes. Two bursae are at the insertion of the Achilles tendon, one in front of the tendon (subcutaneous, retro-Achilles bursa) and one between the tendon and the calcaneus (retrocalcaneal bursa).
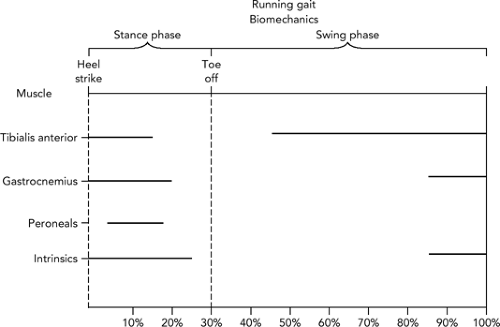
Figure 33.5 Electromyography of the foot during running. (Source: Adapted from
Mann RA, Moran GT, Daugherty SE. Comparative electromyography of the lower extremities in jogging, running and sprinting. Am J Sports Med 1986;14:501, (10).).
Biomechanics. As expected, most foot problems are caused by overuse or repeated microtrauma. Although congenital defects may predispose a foot to injury, the initial etiological factor is almost always overuse.
Painful Heel
A painful heel can be caused by any one of the following (depending upon location of pain and structure involved): bone contusion, bursitis, plantar fasciitis, plantar tear, heel spur, apophysitis, exostosis, Achilles tenosynovitis, calcaneal stress fracture, calcaneal fracture, os trigonum pain, black-dot heel, and bruised or torn fat pad. Talus issues are covered in Chapter 32.
Plantar Calcaneal Pain
Plantar Fasciitis
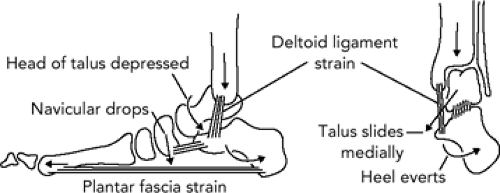
Epidemiology. This is the most common cause of heel pain in sports. Graham (11) contends that most of the pathology is seen around the calcaneal attachment of the plantar fascia and flexor digitorum brevis muscle. In fact, these two structures attach inferior to calcaneal spur and not at its leading edge. Inflammation and/or microtearing near the origin of the plantar fascia is usually involved. The mechanics of the plantar fascia are illustrated in Figure 33.6.
Biomechanics. Normal gait cycle requires the foot to pronate from heel strike to toe-off in order to dissipate the force sustained on the foot during stance phase of gait. Excessive pronation results in abnormal stretching of the plantar fascia in midstance (12) with depression of the longitudinal arch. The presence of an arch is important with gait as it allows a rigid lever for push off, and is called the windlass function of the plantar fascia. As a continuum with the Achilles tendon, tightness in the Achilles tendon may result
in further pronation of the forefoot as dorsiflexion of the foot is limited (13).
Predisposing factors. Pronated foot with high longitudinal arch or a tight Achilles tendon mechanism and related reduced dorsiflexion (14). Associated conditions include pes cavus, pronated foot with forefoot varus, or hypermobile pes planus.
Signs and symptoms. Pain on palpation of the anterior medial calcaneus or arch. Gradual onset of pain, usually located in the medial heel radiating toward the longitudinal arch of the foot. Pain on taking the first few steps in the morning (secondary to shortening of the fascia during sleep) and then a second episode, usually following exercise.
Diagnostic aids. X-ray is typically negative unless there is a traction spur—which is present 60% of the time but is not responsible for the patient’s pain (15). Test passive dorsiflexion of the ankle (there should be 10 to 15 degrees of dorsiflexion). If dorsiflexion is less limited, a tight Achilles mechanism is presumed. Test with knee extended to test gastrocnemius and knee flexed to isolate soleus components of the calf muscles. Squeeze test: cup calcaneus in palm of hand and squeeze (thenar eminence is against medial arch)—usually there is pain at medial arch if plantar fasciitis present. Arch stretch: neutral ankle position with passive dorsiflexion of all toes—pain at calcaneus sign of plantar fasciitis.
Differential diagnosis
Microfracture (stress) or avulsion of the calcaneus
Entrapment of the medial calcaneal branch of the posterior tibial nerve
Tarsal tunnel syndrome
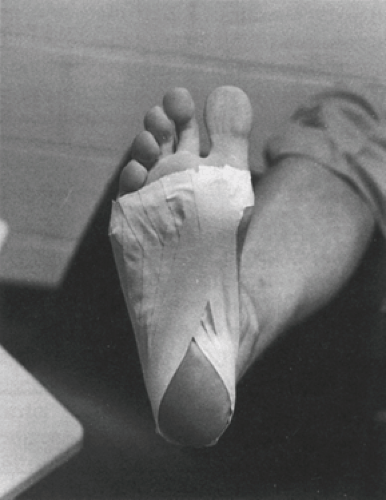
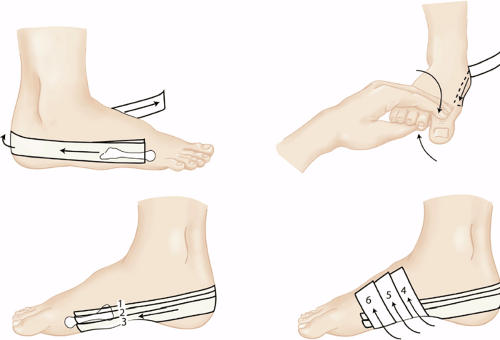
Treatment. Taping (see Figure 33.7) arch support, low dye tape (see Figure 33.8), 1/4 inch heel lifts or heel cups without lift, correction of underlying foot biomechanics with shoe change and/or orthotics1, and stretching the gastrocnemius and soleus. Also add ice massage, cross friction massage (massage is done by thumbs across, 90-degree angle to, longitudinal fibers of plantar fascia), and arch stretch (20). Treatment of any lower kinetic chain issues in the lower limb will also help. Night splints can be very helpful, especially in reducing morning pain (21). Iontophoresis with dexamethasone can be an additional palliative tool, leading to quick results (22). After pain is relieved, intrinsic strengthening is initiated. Surgical intervention for any type of calcaneal/hindfoot pain is a last resort. Surgical removal of calcaneal spurs has been less than satisfactory in the nonathletic population. It should be avoided in an injured athlete. Because the heel pain syndrome is self-limiting, patience may be the most important aspect of any treatment. Also, Achilles and gastrocnemius stretching are appropriate. Overuse protocols should be followed. Occasionally, steroid injections may be administered as well; however, resultant long-term relief is rare.
Calcaneal Stress Fracture
Epidemiology. Most commonly seen in beginning runners, runners who train on asphalt or concrete, or where there is a sudden increase in exercise time. The sports most likely to lead to this type of injury are running and jumping sports (poor landing mechanics increase the risk).
Signs and symptoms. Sudden onset of constant pain is seen with this injury. Percussion tenderness over the calcaneus; compression of the medial and lateral calcaneal tuberosities create extreme pain. The squeeze test (as in the preceding text) can also cause pain in distal calcaneal stress fractures.
Differential diagnosis
Acute calcaneal fracture. Usually the result of trauma—falling on heel from heights
Plantar fasciitis. Pain not as constant, nor onset as sudden in this condition compared with a calcaneal stress fracture.
Calcaneal neuritis. Pain reproduced with pressure or compression over nerve branch; other tests are negative
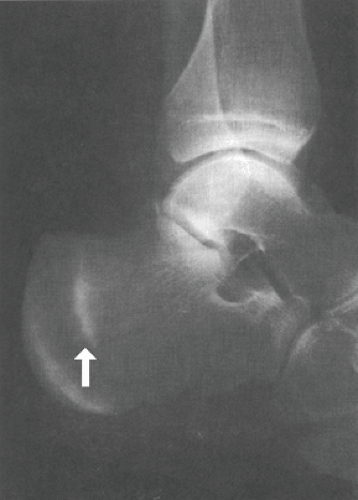
Diagnostic aids. X-ray usually negative because of the lack of sensitivity of x-rays to pick up stress fractures earlier than 3 weeks, and an extremely thin calcaneal cortex. It takes up to 6 weeks before any sclerotic line or cortical change can be seen on x-ray (see Figure 33.9). Axial view is excellent for visualization of the calcaneus. Computed tomography (CT) scans can be helpful in characterizing complex calcaneal fractures. A triple phase nuclear medicine scan is helpful.
Treatment. Similar to any stress fracture. Ambulation should be encouraged if the patient is comfortable; if severe pain is present, consider non-weight bearing with crutches for ambulation. Alternate non–gravity-dependent sports such as swimming can be pursued to keep up cardiovascular fitness.
Return to competition. Consult overuse guidelines.
Os Trigonum Syndrome (Posterior Impingement-Type Syndrome)
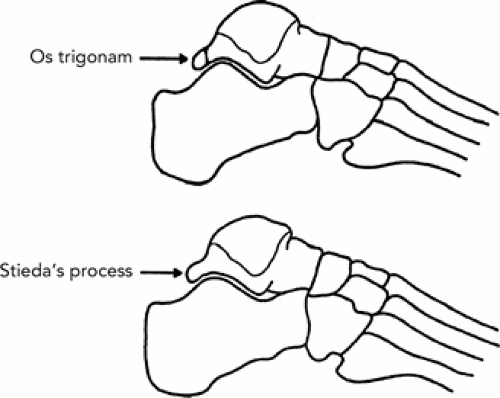
Anatomy and epidemiology. Accessory ossicle at posterior talus. It is found in approximately 23% of the general population (28). The most common sports involved in symptomatic conditions are jumping and ballet (en pointe)—especially in young female dancers (29). Sports that cause distal load with forced full plantar flexion (i.e., soccer) can also be symptomatic. The os trigonum can be attached to the posterior tals (it is then called Stieda’s process) (see Figure 33.10).
Signs and symptoms. Pain in back of ankle with extreme plantar flexion with axial load or distal load to foot. Examples are ballet (en pointe), soccer (kick ball with tip of foot), and runners (downhill run).
Differential diagnosis. This syndrome is a result of (a) acute os trigonum avulsion fracture, (b) irritation of a previous os trigonum fracture, or (c) congenital os trigonum nonunion with irritation. Imaging with lateral x-ray and making a comparison with opposite ankle can help differentiate Sheperd’s fracture (avulsion fracture of the posterolateral process of talus). Also, ancillary lateral view of the ankle in maximum plantar flexion may help. Magnetic resonance
imaging (MRI) is another tool that is useful in differential and treatment decisions.
Treatment. Evaluate for shoe wear that causes pressure to area. Taping may be done to limit forced terminal extension in sports that distally load into forced plantar flexion (kicking with tip of foot). Relative rest from aggravating activity, ice massage, intrinsic foot and ankle strengthening, and NSAIDs are recommended. A xylocaine injection into the posterior capsule can also be used as a diagnostic and treatment tool. Surgical excision of symptomatic os trigonum may be performed if there is no resolution; this is usually done in dancers if they are at least 16 years of age.
Calcaneo Apophysitis (Seiver’s or Sever’s Disease)
Epidemiology. Found most often in males between ages of 8 and 13. With increased participation in youth sports and early specialization in certain sports, this problem has become more common and is also increasingly seen in girls.
Biomechanics. Considered a traction injury eliciting stress from the Achilles tendon on a not-yet-fused posterior calcaneal apophysitis.
Symptoms. Pain usually occurs bilaterally with increased sensitivity to the back of the heel. Walking is usually painless but wearing shoes causes pain.
Diagnostic aids. X-ray is usually of little help, especially if the condition appears to be bilateral. At best, some cortical hypertrophy may be present.
Treatment. Symptomatic because the problem is self-limiting. Activities should be decreased to the point of comfort. Quarter inch heal lifts may take some pressure off the Achilles tendon attachment. Speed of symptom resolution can vary from 2 weeks to 3 months depending upon symptom stage when first treated and ability to “relatively rest” the athlete.
“Black-Dot” Heel
Epidemiology. Seen primarily in runners and athletes in walking casts where cotton padding has balled-up (30).
Biomechanics. Caused by pinching of skin at the bottom of heel between the heel counter and the sole of the shoe.
Signs and symptoms. Painless black or blue plaque on the posterior or posterolateral heel. Oval or circular lesions(s) are found lying just above thickened plantar skin. These lesions are not raised, but represent microhemorrhages of capillaries secondary to repetitive trauma.
Treatment. Self-limiting if insult is removed.
Prevention. Place felt inside shoe to smooth out heel counter/sole junction, change shoe, or replace cast.
Heel Bruise
Epidemiology. Repetitive, high impact.
Biomechanics. Calcaneal fat pad normally cushions the heel on impact. However, the quality of the fat pad can change with age and soften, offering less protection. This condition may predispose heel in the masters athlete, usually a runner, to bone bruising and subperiosteal bleeding. Runners with short overstrides or those who run downhill a great deal are predisposed to this condition.
Symptoms. Pain with compression of fat pad; not typically with squeezing of calcaneus.
Treatment. Firm heel counter or heel cup (worn in athletic and daily wear shoes). A donut pad may initially relieve the acute inflammatory pain. Correction may be made in training technique related to jump landing and heel strike during running.
Posterior Calcaneal Pain
Bursitis Subcutaneous (Retro-Achilles; “Pump Bump”)
Epidemiology. Poor-fitting shoes. Also calcaneal changes related to Haglund’s deformity (see subsequent text).
Signs and symptoms. Pain at superior calcaneal tuberosity. There may be redness, swelling, and significant pain localized to the area of the superficial bursa overlying the Achilles tendon (see Figure 33.11)—directly below position of the heel counter. You may be able to palpate the bursa if it is thickened or enlarged. Squeezing the area between the posterior part of the calcaneus and the Achilles tendon should elicit pain. Also check for decreased passive dorsiflexion.
Treatment. Change shoe or apply padding; ice massage, aspiration and steroid injection. Note that a “pump bump” may result from a chronically inflamed subcutaneous bursitis—small bony flakes or avulsions from the os calcis can form a hardened, thickened bony prominence in longtime running athletes. To treat this, increase padding, and look at heel counter for shape and fit; the athlete may need heel lifts or custom molded orthotics. Surgery is not indicated because of the close proximity of Achilles tendon.
Retrocalcaneal Bursitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree