The concept of femoroacetabular impingement (FAI) emerged following the observation that FAI can be precipitated by acetabular reorientation and can produce new labral damage. Interest in the association between chondrolabral damage and variations in femoral and acetabular anatomy has established a causal relationship between mechanical aberration in the function of the hip joint and the development of labral and cartilage damage. The accepted definition of FAI is that it is characterized by abnormal mechanical contact between the rim of the acetabulum and the upper femur. Combinations of certain morphologies and movements may lead to FAI.
Key points
- •
Femoroacetabular impingement (FAI) is a clinical syndrome of hip pain, limitation in movement, and joint damage from abnormal mechanical contact of the acetabular rim and the proximal femur.
- •
There is a high prevalence of morphologic abnormalities associated with FAI in asymptomatic individuals.
- •
Cross-sectional and longitudinal studies support FAI playing a causative role in the development of osteoarthritis and need for total hip arthroplasty in certain patients.
- •
Surgical treatment approaches for FAI include hip arthroscopy, anterior mini-arthrotomy with/without arthroscopic assistance, and surgical dislocation of the hip.
What is femoroacetabular impingement?
The modern concept of femoroacetabular impingement (FAI), especially its causal relation to acetabular labral and cartilage damage, emerged following the observation that FAI can be precipitated by acetabular reorientation and can produce new labral damage. Following this observation, interest in the association between chondrolabral damage and variations in femoral and acetabular anatomy has established a causal relationship between mechanical aberration in the function of the hip joint and the development of labral and cartilage damage. The resulting modern accepted definition of FAI is that it is characterized by abnormal mechanical contact between the rim of the acetabulum and the upper femur. Certain anatomic femoral or acetabular morphologies, hip-specific supraphysiologic flexion or rotational movements, repetition, and forceful motions may damage the acetabular labrum and the cartilage around the rim of the acetabulum, leading to a clinical syndrome of hip pain, limitation of movement, and joint damage now known as FAI.
What is femoroacetabular impingement?
The modern concept of femoroacetabular impingement (FAI), especially its causal relation to acetabular labral and cartilage damage, emerged following the observation that FAI can be precipitated by acetabular reorientation and can produce new labral damage. Following this observation, interest in the association between chondrolabral damage and variations in femoral and acetabular anatomy has established a causal relationship between mechanical aberration in the function of the hip joint and the development of labral and cartilage damage. The resulting modern accepted definition of FAI is that it is characterized by abnormal mechanical contact between the rim of the acetabulum and the upper femur. Certain anatomic femoral or acetabular morphologies, hip-specific supraphysiologic flexion or rotational movements, repetition, and forceful motions may damage the acetabular labrum and the cartilage around the rim of the acetabulum, leading to a clinical syndrome of hip pain, limitation of movement, and joint damage now known as FAI.
Classification
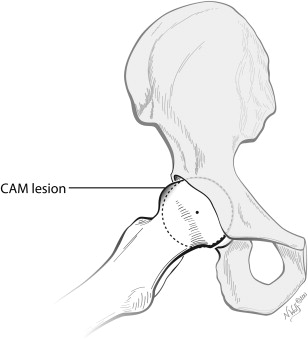
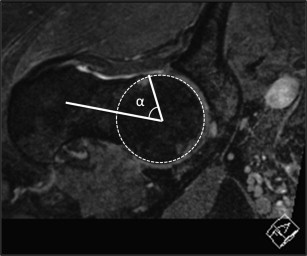
Two distinct hip morphotypes have been described that are associated with intracapsular, mechanical FAI. The CAM morphotype of FAI is an aspherical epiphyseal extension that produces a characteristic bump at the junction of the femoral head and femoral neck ( Fig. 1 ). The origin is thought to be caused by an extension of the upper femoral epiphysis along the anterolateral femoral neck junction ; however, the pathogenesis of this bump is not well understood and may represent a distinct type of upper femoral chondroepiphyseal maturation. Because the size, location, and extension of the deformity are unique for each hip, the ability to visualize the prominence using plain radiographs is variable. Frog-lateral, cross-table lateral, or Dunn-lateral views may be used; however, the reliability depends on the location of the deformity and the rotation of the limb during the radiograph. Because of this variability, radial magnetic resonance imaging (MRI) reconstructions are often used to more accurately assess the morphology of the head-neck junction and minimize the chance of missing CAM lesions ( Fig. 2 ). On either plain radiographs or radial sequences, the severity of deformity can be characterized by the alpha angle of Nötzli. The alpha angle estimates the degree at which the radius of curvature of the femoral head begins to increase. Thus, larger alpha angle measurements indicate a more aspherical femoral head.
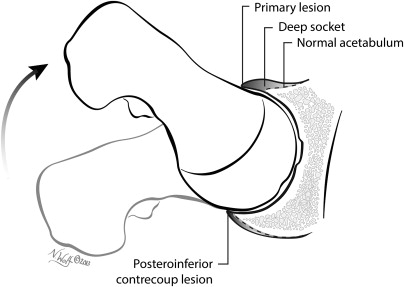
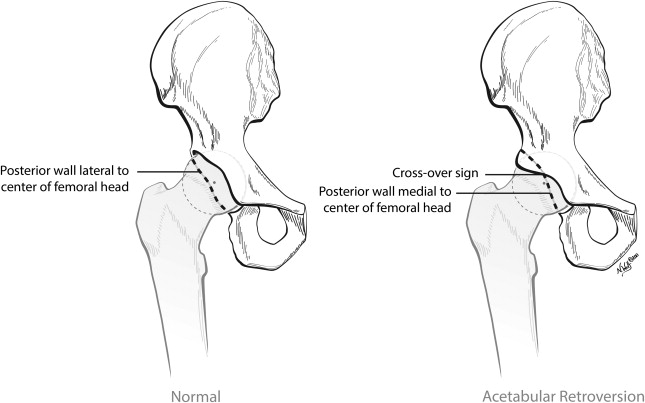
Acetabular-sided deformity or pincer impingement includes global overcoverage, focal overcoverage, and retroversion of the acetabulum, and results in premature contact between the femoral neck and acetabular rim when the hip is flexed ( Fig. 3 ). These features are recognizable radiographically using an anteroposterior (AP) pelvis radiograph. The coverage of the acetabulum relative to the femoral head is traditionally assessed using the lateral center-edge angle (LCE). There is general agreement that a normal LCE is between 25° and 35° and that hips with an LCE greater than 40° are at risk for impingement in flexion. Focal overcoverage can be assessed using the crossover sign that is observed when the anterior acetabular wall crosses over the posterior acetabular wall on a properly oriented AP pelvis radiograph ( Fig. 4 ). There is conflicting information regarding the sensitivity of the crossover sign. Although the crossover sign may represent true focal acetabular overcoverage in some cases, in others it may be artifactually caused by the orientation of the anterior inferior iliac spine. In addition, when a crossover sign is accompanied by a posterior wall sign, which occurs when the posterior wall of the acetabulum is located medial to the center of the femoral head, the acetabulum may be retroverted and the posterosuperior femoral coverage may be insufficient. A crossover sign accompanied by a posterior wall sign may be associated with anterior impingement when the hip is flexed and posterosuperior instability when the hip is in extension.
Many hips are thought to have features of both CAM-type femoral morphology and acetabular overcoverage, resulting in so-called mixed-type impingement.
Pathophysiology
The mechanics of impingement limit the degree of sagittal plane hip motion, diminishing the degree to which an affected individual is able to squat. Normal mechanical gait parameters are altered in patients affected by CAM-type FAI, with demonstrated decrease in hip abduction and frontal plane motion compared with control hips. Chegini and colleagues used computational models to analyze stresses along the acetabular rim in simulated dysplastic and impinging joints. Impingement was modeled by increasing the alpha angle and the acetabular depth using a standing-to-sitting motion and was shown to cause distortion and shearing at the bone-tissue interface, a calculated conclusion that is consistent with damage observed clinically in impinging joints at the time of surgery. These mechanical studies support theories developed by observing patterns of chondral injury at the time of surgical treatment.
CAM-type impingement, in which an aspherical bump enters the acetabular fossa during flexion, causes labral distortion and shear forces within the peripheral acetabulum that can cause detachment of the labrum from the rim of the acetabulum and full-thickness or partial-thickness delamination injuries of the hyaline cartilage within the joint. In contrast, the damage pattern in hips with pincer-type mechanics is more peripheral. These hips often have a characteristic trough located in the femoral neck, thought to be related to remodeling caused by chronic and repetitive contact between the acetabular rim and femoral neck. The labrum is therefore crushed between the bony acetabular rim and femoral neck and the peripheral-most acetabular cartilage may become detached and frayed. In addition, contrecoup chondrolabral lesions in the posterior acetabulum, thought to result from anterior levering of the femur causing posterior shear, have been observed clinically. The two major differences between CAM-type and pincer-type injury patterns are the increased depth of chondral injury associated with the CAM mechanism, and confinement of damage to the rim and peripheral acetabulum in pincer-type impingement.
Clinical presentation
The presentation of patients with symptomatic anterior FAI has been described by multiple investigators. Patients usually present with insidious-onset pain about the hip that is characteristically localized to the groin but may be experienced in the buttock, lower back, trochanteric region, or the anterior thigh and knee. Pain may be precipitated by athletic activity or activities that require flexion, such as crouching or sitting. The pain pattern often goes unrecognized by primary physicians, leading to missed diagnosis or misdirected treatment. Because the symptoms caused by FAI are not disease specific, careful patient history is essential when entertaining the diagnosis of FAI.
The physical examination of a patient with symptomatic FAI is characterized by painful limitation of hip flexion. In patients with highly irritable hip joints, hip guarding and compensatory lumbar motion may confound the physical examination. Range of motion is usually limited in hips that are morphologically prone to symptomatic FAI, with average flexion reportedly slightly greater than 90°. The classic provocative maneuver is the anterior impingement test, which is pain elicited by flexion, adduction, and internal rotation of the affected hip ( Fig. 5 ). Other provocative tests include the resisted straight-leg raise and the posterior impingement test. Clinical symptoms and physical examination signs must be correlated with radiographic data to firmly establish the diagnosis of FAI.
Prevalence of disease
The prevalence of clinically significant FAI remains unknown. The reported prevalence of FAI varies widely depending on the parameters used to define the condition. Ochoa and colleagues reviewed 155 patients with a mean age of 32 years (range, 18–50 years) who presented to primary care or orthopedic clinics with a chief complaint of hip pain. Based on radiographic signs of FAI (herniation pits, pistol grip deformity, crossover sign, center-edge angle >39°, and/or alpha angle >50°), the investigators reported that 87% of the patients had at least 1 finding consistent with FAI, and 81% had at least 2 findings.
However, several recent studies have established a high prevalence of morphologic abnormalities associated with FAI in asymptomatic individuals as well:
- •
Reichenbach and colleagues reported on 1,080 asymptomatic military recruits in Sumiswald, Switzerland, of whom 430 were randomly selected, and 244 agreed, to undergo a radial sequence MRI looking for abnormal morphology at the femoral head-neck junction.
- ○
Mean age was 19.9 years
- ○
Adjusted overall prevalence of CAM-type deformity was 24% [95% CI 19, 30].
- ○
- •
Jung and colleagues evaluated 838 asymptomatic hips in 419 randomly selected patients aged 25 to 92 years who underwent abdominal or pelvic computed tomography (CT) for medical diseases unrelated to the hip. AP scout views of CT scans were used to measure asphericity of the femoral head-neck junction using the alpha angle as described by Nötzli and colleagues. Study participants were classified according to criteria defined by Gosvig and colleagues based on the Copenhagen Osteoarthritis Study.
- ○
For men, the three categories for α-angle ranges were:
- 1.
Pathological (≥83°)
- 2.
Borderline (69° to 82°)
- 3.
Normal (≤68°).
- 1.
- ○
For women, the three categories for α-angle ranges were:
- 1.
Pathological (≥57°)
- 2.
Borderline (51° to 56°)
- 3.
Normal (≤50°).
- 1.
- ○
Ages ranged 25 to 92 years
- ○
Men <50 years of age: mean α-angle was 57.2° with 14% demonstrating pathologic α-angles.
- ○
Women <50 years of age: mean α-angle was 45.3° with 7% demonstrating pathologic α-angles
- ○
- •
Hack and colleagues studied 200 asymptomatic volunteers using radial MRI reformats.
- ○
Ages ranged 21.4 to 50.6 years; mean 29.4 years
- ○
α-angles were measured at both the 3 o’clock and 1:30 position with CAM deformity defined as an angle exceeding 50.5°.
- ○
At the 1:30 position, 53% of the volunteers had evidence of CAM morphology
- ○
At the 3 o’clock position, 14% had elevated α-angles.
- ○
These prevalence data in patients with minimal or no symptoms show the importance of clinical correlation during the diagnostic work-up for FAI. The presence of imaging findings consistent with FAI alone is not sufficient to warrant intervention. The treating clinician must rely on the history, physical examination, and imaging findings to determine whether a symptomatic patient is symptomatic because of FAI.
Causative role in osteoarthritis
The contemporary theory of FAI as a causative factor in the development of osteoarthritis has been championed by Ganz and colleagues, and holds that the morphologic abnormalities of the femoral head and/or acetabulum result in abnormal contact between the femoral neck/head and the acetabular margin. This abnormal contact leads to supraphysiologic stress causing tearing of the labrum and avulsion of the underlying cartilage region ( Fig. 6 ). The continued abnormal contact results in further deterioration and wear of the articular cartilage, with eventual onset of arthritis. However, questions remain as to whether FAI is a cause or a result of osteoarthritis and whether joint deformities in FAI are congenital, developmental, or the reaction to the arthritic process (osteophytes).
Recent epidemiologic studies have attempted to clarify the role of FAI in the pathogenesis of osteoarthritis:
- •
The Nottingham United Kingdom Genetics of Osteoarthritis and Lifestyle (GOAL) study examined the morphology of the hip in 566 persons with unilateral hip osteoarthritis and compared this to the contralateral asymptomatic hip to non-osteoarthritic control hips from 1,100 subjects who had undergone intravenous urograms.
- ○
All patients were ≥45 years of age or older; mean age was 66 years.
- ○
48% of the subjects were women.
- ○
CAM morphology was defined as a ratio of head to neck diameter less than 1.27.
- ○
Based on this criterion, the investigators reported a 5.5% risk of developing osteoarthritis in the contralateral non-osteoarthritic hip compared to a 3% risk in the control group.
- ○
A pistol grip deformity conferred an 8.3% risk of developing osteoarthritis in the contralateral non-osteoarthritic hip compared to a 3.6% risk in the control group.
- ○
Both factors were strongly and significantly associated with an increased risk of developing hip osteoarthritis after adjusting for age, body mass index, and gender.
- ○
In addition to this representative cross-sectional study, longitudinal studies of FAI have established the temporal relationship of cause to effect, by measuring proximal femoral morphology before it is altered by osteoarthritis:
- •
A prospective study of FAI in the Cohort Hip and Cohort Knee (CHECK) study reported on a Dutch national sample of 723 patients presenting for the first time with recent onset of hip or knee pain. Initial AP pelvic radiographs were measured to determine the α-angle, and subjects were followed for 5 years to determine the risk of developing end-stage osteoarthritis.
- ○
Ages ranged 45 to 65 years
- ○
80% of the cohort was female
- ○
Subjects had no osteoarthritis at baseline with either a Kellgren-Lawrence osteoarthritic grade of 0 (76%) or grade 1 (24%).
- ○
Hips with a baseline AP α-angle >83° had a 25% risk of developing end-stage osteoarthritis within 5 years compared to a less than 2% risk of end-stage osteoarthritis in hips with an α-angle less than 83° (odds ratio of 9.7 adjusted for age, sex, BMI and baseline Kellgren-Lawrence grade).
- ○
Hips with both an α-angle >83° and decreased internal rotation ≤20° had a 53% risk of developing end-stage osteoarthritis within 5 years.
- ○
- •
The Chingford cohort provides another recent longitudinal study of the relationship between hip morphology and the development of osteoarthritis. 1003 healthy female subjects were enrolled after undergoing a baseline AP radiograph of the pelvis, which was measured the presence of CAM and pincer deformity. At 19 year follow-up, these radiographs were repeated. Of those patients who went on to THA, the baseline hip morphology was compared to a random sample of 243 hips that did not require THA.
- ○
Ages ranged 44 to 67 years
- ○
Median AP α-angle in those who required THA was 62.4° at baseline compared to 45.8° in controls ( P = .001).
- ○
The odds ratio of needing a THA increased 1.05 for each 1° increase in initial α-angle.
- ○
Recent evidence also suggests that FAI morphology may result from early exposure to high-impact sports, and may therefore be developmental in origin rather than a reaction to the arthritic process. Kapron and colleagues reported that 95% of 134 hips in collegiate football players had at least one radiographic sign of CAM or pincer impingement, which exceeds the reported prevalence in asymptomatic members of the general population. Siebenrock and colleagues showed a 10-fold increase in the prevalence of CAM morphology in a cohort of elite basketball players compared with nonactive age-matched controls. In addition, the investigators showed increasing alpha angles in the athletes during skeletal maturation, and suggested that repeated high-stress activities during childhood may modulate growth of the proximal femur toward an abnormal shape via subclinical physeal injury.
Based on the previously mentioned studies in which FAI morphology was studied before the presence of radiographic osteoarthritis and the prevalence studies in young, asymptomatic persons it is clear that FAI, and its morphologic risk factors, are common in young adult hips and predisposes to the later development of osteoarthritis in certain patients. Longitudinal studies also support that, in both men and women aged 45 to 65 years, the presence of CAM deformities at baseline substantially increases the risk of developing osteoarthritis and the need for a THA. However, in most hips the presence of a CAM lesion is not sufficient in isolation to lead to the development of clinically significant and symptomatic osteoarthritis. At this point, there is insufficient evidence from longitudinal population studies to confirm a similar association between the presence of a pincer deformity and the development of clinical or radiographic osteoarthritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





