Femoral Shaft
Theerachai Apivatthakakul
Chang-Wug Oh
INDICATIONS
The standard treatment of femoral shaft fractures is closed intramedullary nailing.1 However, in some situations an intramedullary nail may be contraindicated or technically not feasible. These may include polytrauma patients, associated femoral shaft and neck fractures, pelvic and acetabular fractures, spinal fractures, patients with pulmonary compromise, pediatric femoral shaft fractures, a deformed or stenotic femoral canal, and periprosthetic femoral fractures. In these situations, plate fixation has many advantages and is often the only feasible option.2, 3, 4, 5 and 6 Conventional open plating requires extensive exposure, stripping of muscle and periosteum around the bone fragments, and injury to the blood supply, all of which can lead to delayed union, nonunion, infection, or implant failure.7 With the evolution of the plate fixation in the past decade,8 minimally invasive plate osteosynthesis (MIPO) has gained popularity with acceptable clinical outcomes.9, 10, 11, 12 and 13
PATIENT POSITIONING
The patient is positioned supine on a radiolucent operating table. A padded bolster is placed under the distal thigh and knee to maintain it in 30 degrees of knee flexion. A small bump should be placed under the ipsilateral hip to offset external rotation of the limb such that the patella faces directly anteriorly. However, the presence of a hip bump must be remembered and removed at the end of the procedure when determining limb rotation. A standard fracture table with traction is not recommended because manipulation of the fracture is difficult. Instead, a fully radiolucent flat top table is used.
Preparation of the lower limb is performed depending on the configuration of the fractures. In simple transverse, oblique, spiral, or wedge fractures, determination of the length can be done by using the apposition of the fragments. In these cases, the injured lower extremity is prepared with the uninjured lower extremity elevated in a hemilithotomy position in order to obtain an AP and lateral x-ray of the fractured femoral shaft. In comminuted or segmental comminuted fractures in which the length cannot be determined by fragment apposition, both the lower extremities may be sterilized and prepared in the field to directly compare the length and rotation. With this method, the lateral x-ray view is obtained by lifting the uninjured limb upward to avoid obstruction of the x-ray. The image intensifier is positioned on the contralateral side of the patient. The c-arm is tilted so that the fluoroscopy beam is able to obtain orthogonal images along the entire length of the femur.
SURGICAL APPROACHES
A direct lateral approach is the standard approach for MIPO of the femur, as it provides access to the entire femur with no main neurovascular structures at risk. Before making incisions, the fracture must be provisionally reduced to restore the alignment as close to anatomic as possible. Mark the location of the fractures on the skin, and determine the plate length by the desired plate-span ratio and plate-screw density.14 In general, we prefer to err on the side of using longer plates with fewer screws to maximize stability while minimizing the biologic insult. Make incisions proximally and distally corresponding to the proximal and distal ends of the plate (Fig. 11.1). Dissect deep through the iliotibial band, and split the vastus lateralis longitudinally. The lateral femoral cortex is exposed with two Hohmann retractors.
 Figure 11.1 The incisions are made several centimeters in length, based on the planned plate length and position. |
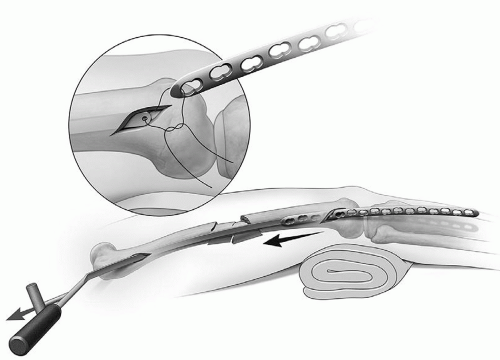 Figure 11.2 Tie a suture to the tip of the tunneling instrument and the plate hole and pull the plate back into the tunnel. |
Preparation of the submuscular tunnel under the vastus lateralis can be done either proximal to distal or distal to proximal. A tunneling instrument can be a helpful tool to prepare the tunnel over the lateral cortex, as it is easier to advance and change direction than with the beveled end of a plate. This tunnel should be created in a submuscular but extraperiosteal plane. Once the tunneler is passed through the far incision, use a suture to connect the tunneler to the plate and pull it back into the tunnel to preserve the track (Fig. 11.2).
In osteoporotic fractures with previous proximal plate fixation, open fractures, or when a lateral external fixator is in place, an anterior approach can be considered to avoid implant removal or pin tract contamination. This involves splitting the rectus and vastus intermedius, and should be avoided when possible.
REDUCTION TECHNIQUES
There are two general methods for reduction of the femoral shaft fractures when using a minimally invasive technique. First, the fracture is reduced and the desired reduction is maintained with devices such as cerclage wires, collinear reduction forceps, an external fixator, Schanz pin joysticks, an intramedullary splint, or a femoral distractor. Collinear reduction forceps or cerclage wires are useful in reduction and maintain reduction of simple long oblique or spiral fractures. In fracture patterns with a single butterfly fragment, two wire loops around the proximal and distal end of the butterfly is a very effective provisional reduction tool. External fixators or Schanz pin joysticks are typically the first choice for simple transverse, short oblique or comminuted fractures in which cerclage wiring or a collinear clamp cannot be used.
The second general reduction strategy involves introducing the plate first adjacent to an unreduced fracture, and reducing the fracture indirectly “under” the plate, using traction, bumps, percutaneous reduction tools, or screws through the plate. This method is recommended in wedge or comminuted fractures, since anatomical reduction is not needed or possible. After fixation of the plate to one fragment, reduction is done to achieve correct length, angulation, and rotation. Then, using a cortical screw through a plate hole or a collinear clamp, the other fragment is realigned and reduced to the plate. In simple transverse or short oblique fractures, this technique is more difficult because the fracture must be anatomically reduced before using reduction screw.
Reduction with Mini-Open Cerclage Wiring
Cerclage wiring for reduction of long oblique or spiral fractures has been well described. The mechanism of reduction is that the wire applies circumferential force around the bone to bring the fragments to their anatomic position and maintains the reduction while the plate
and screw are applied. Historically, the disadvantage of cerclage wiring in the femur is that a large exposure is often needed, which can involve stripping of the muscle and periosteum and disruption of the blood supply. Traditional wire passers for cerclage techniques were designed for open wiring through large incisions. Newer modular cerclage wire passers have been designed specifically for minimally invasive techniques.15,16 These devices have a larger curve and angle of the handle away from the skin, making them amenable to use through much more limited exposures. Two detachable arms can be independently inserted anteriorly and posteriorly around the femur at the fracture site through a 2-cm incision, minimizing insult to the local biology.
and screw are applied. Historically, the disadvantage of cerclage wiring in the femur is that a large exposure is often needed, which can involve stripping of the muscle and periosteum and disruption of the blood supply. Traditional wire passers for cerclage techniques were designed for open wiring through large incisions. Newer modular cerclage wire passers have been designed specifically for minimally invasive techniques.15,16 These devices have a larger curve and angle of the handle away from the skin, making them amenable to use through much more limited exposures. Two detachable arms can be independently inserted anteriorly and posteriorly around the femur at the fracture site through a 2-cm incision, minimizing insult to the local biology.
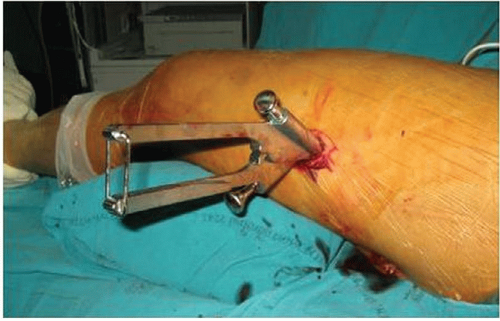 Figure 11.3 The arms of the modular wire passer are passed around the femur through a small incision. The arms are connected to mate the tubes at the fracture site. |
To perform this technique, first make an incision approximately 2 cm long in the region of the fracture site. Longitudinally split the fascia lata and vastus lateralis to access the fracture site. Use a long clamp to penetrate the intermuscular septum and the linea aspera.
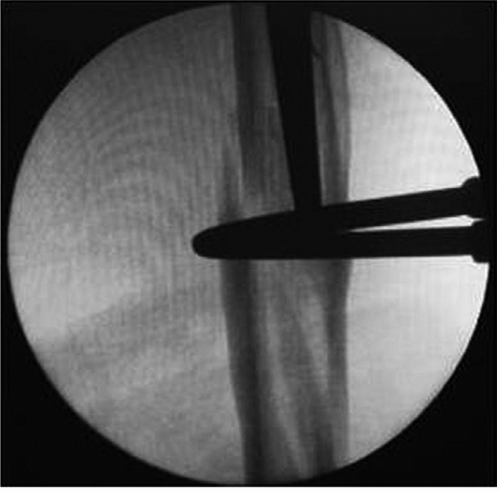
Preparation of the wire path using a tunneling device is necessary to facilitate insertion of the cerclage passer through the fascia lata and the muscle envelope. Place one trocar in each tube of the cerclage passer to prevent the soft tissue from entering the cannulated tubes of the passer. Insert one-half of the cerclage passer into the prepared tunnel and pass it around the femur posteriorly. It is critical to contact bone while passing the device to avoid injury to the sciatic nerve. Next, insert the other half of the forceps. Connect the flat parts of the forceps and close the handles, allowing the tips to mate around the femur (Fig. 11.3). The correct closed position can be verified by the image intensifier (Fig. 11.4). Remove the trocar from each side of the forceps, and pass the wire through the tube until it passes through the opposite side. Unlock the forceps and disconnect the two halves of the forceps (Figs. 11.5 and 11.6). For long spiral fractures, a second wire can be helpful to achieve a more concentric reduction and distribute the forces during wire tightening (Fig. 11.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree