Femoral Fractures
Manish K. Gupta
Robert L. Kalb
FEMORAL NECK FRACTURE
Femoral neck fractures are the second most common hip fracture of the 280,000 that occur each year. These occur in two populations. Five percent are in young adults with high-energy injuries, whereas 95% are in elderly with underlying osteoporosis.
Mechanism of Injury
In the elderly, femoral neck fractures result from a fall while standing. Three common mechanisms are
Fall directly onto the greater trochanter
Lateral rotation with sudden increase in load
Spontaneous completion of a stress fracture that causes the fall (incidence increased with severity of osteoporosis)
Diagnosis
The patient may present with a history of hip pain over weeks and then a sudden fall due to a stress fracture. Pain with walking occurs in a nondisplaced fracture. There is inability to walk with displaced fractures. On physical examination, note shortening and rotation of the leg and pain with palpation of the hip and with range of motion.
Radiology
Anteroposterior (AP)/lateral views should be used to evaluate the fracture line and to assess degenerative arthritis. If no fracture line is seen and index of suspicion is high for fracture, get a magnetic resonance imaging scan (Fig. 1).
Initial Treatment
Bed rest with Buck’s traction, 5 lb on affected extremity, to prevent motion. Prevent blood clots by placing calf pumps and start enoxaparin (Lovenox) low-molecular-weight heparin. Make sure to discontinue Lovenox 12 hours preoperatively. A medical consultation is needed for surgical clearance. Draw preoperative laboratory tests: prothrombin time/partial thromboplastin time, complete blood cell count, chemistry profile, electrocardiogram, chest x-ray, and urinalysis. Do all in emergency room on admission to avoid delay in medical clearance.
Definitive Treatment
For all fractures, orthopedic evaluation is warranted. Nondisplaced fractures can be treated with non-weight bearing for 6 to 8 weeks; however, surgical treatment is best if pain is severe. For displaced fractures, surgical treatment with prosthetic replacement (hemiarthroplasty) is standard. Deep venous thrombosis (DVT) prophylaxis is continued 4 weeks postoperatively with fondaparinux (Arixtra), 2.5 mg q.d. Rehabilitation goals are to decrease pain and resume walking to prevent complications of sepsis, skin ulcers, pneumonia, bowel dysfunction, and DVT.
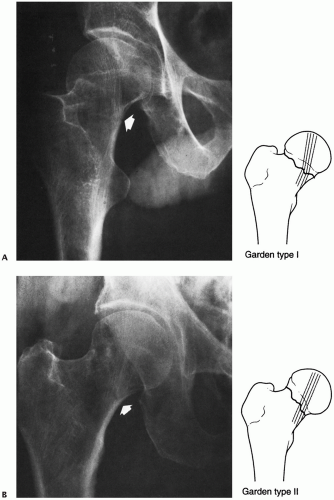 Figure 1 The Garden classification of femoral neck fractures. Type I fractures can be incomplete, but much more typically, they are impacted into valgus and retroversion (A). Type II fractures are complete but undisplaced. These rare fractures have a break in the trabeculations, but no shift in alignment (B). Type III fractures have marked angulation but usually minimal to no proximal translation of the shaft (C). In the Garden type IV fracture, there is complete displacement between fragments, and the shaft translates proximally (D). The head is free to realign itself within the acetabulum, and the primary compressive trabeculae of the head and acetabulum realign (white lines).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





