Fasciotomy of the Leg for Acute Compartment Syndrome
George Partal
Andrew Furey
Robert V. O’Toole
DEFINITION
Compartment syndrome remains one of the most devastating orthopaedic conditions if not treated appropriately. The potential clinical sequelae and medicolegal implications of possible missed compartment syndrome make it one of the most important entities in all of orthopaedic surgery.5
Compartment syndrome is a condition, with numerous causes, in which the pressure within the osteofascial compartment rises to a level that exceeds intramuscular arteriolar pressure, resulting in decreased blood flow to the capillaries, decreased oxygen diffusion to the tissue, and, ultimately, cell death. This is the rare orthopaedic emergency for which evidence indicates that delay in treatment results in worse outcomes.10, 13, 29, 30, 31, 34
The clinical sequelae of missed compartment syndrome can be life- and limb-threatening. Myonecrosis can lead to acute renal failure and multiorgan failure if not appropriately managed.24
Any situation that leads to increased pressure within the compartment can result in compartment syndrome.
The impermeable fascia prevents fluid from leaking out of the compartment and also prevents an increase in volume that could reduce pressure within the compartment.
The incidence of compartment syndrome is 7.3 per 100,000 male patients and 0.7 per 100,000 female patients.
This chapter describes acute compartment syndrome (ACS), in contrast to exertional compartment syndrome.
Exertional compartment syndrome is a transient chronic condition brought on by exercise. Unlike ACS, exertional compartment syndrome is not an emergency, and its treatment is beyond the scope of this chapter.
ANATOMY
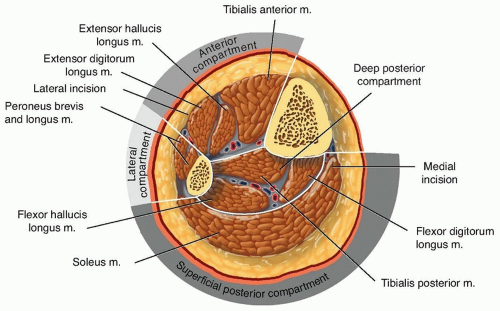
The lower leg has four compartments: anterior, lateral, superficial posterior, and deep posterior (FIG 1; Table 1).
The anterior compartment is bound anteriorly by fascia, laterally by the anterior intermuscular septum, and posteriorly by the interosseous membrane between the fibula and tibia.
The four muscles in this compartment are the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius.
The neurovascular bundle includes the deep peroneal nerve and the anterior tibial artery.
The deep peroneal nerve provides sensation to the first dorsal web space of the foot and motor function to all the muscles in the anterior compartment.
The anterior tibial artery travels in this compartment just anterior to the tibiofibular interosseous membrane and continues in the foot as the dorsalis pedis artery.
The lateral compartment is bordered anteriorly by the fascia, posteriorly by the posterior intermuscular septum, and medially by the fibula.
The lateral compartment has only two muscles: the peroneus longus and the peroneus brevis.
The major nerve supply to the lateral compartment is the superficial peroneal nerve, which supplies the two muscles
of the compartment. The nerve supplies sensation to the dorsum of the foot, except the first dorsal web space.
Table 1 Compartments of the Lower Leg
Compartment
Muscles
Major Arteries
Nerves
Anterior
Tibialis anterior
Extensor hallucis longus
Extensor digitorum longus
Peroneus tertius
Anterior tibial
Deep peroneal
Lateral
Peroneus brevis
Peroneus longus
None
Superficial peroneal
Deep peroneal (proximal in leg)
Deep posterior
Posterior tibialis
Flexor hallucis longus
Flexor digitorum longus
Posterior tibial
Peroneal
Tibial
Superficial posterior
Gastrocnemius
Soleus
None
None
Because the deep peroneal nerve courses proximally around the fibular head, both the deep and superficial peroneal nerves travel proximally within this compartment.
No main vessels are present in this compartment, and the muscles receive their blood supply from the peroneal and anterior tibial arteries.
The deep posterior compartment contains the flexor digitorum longus, tibialis posterior, and flexor hallucis longus muscles. Popliteus is thought to lie within this compartment proximally.
Although it is not considered a separate compartment, the tibialis posterior muscle can have its own fascial covering.
The deep posterior compartment contains the main neurovascular bundle of the posterior compartment, which consists of the tibial nerve, posterior tibial artery and vein, and peroneal artery and vein.
The superficial posterior compartment contains the gastrocnemius, soleus, and plantaris muscles, which are supplied by branches of the tibial nerve, posterior tibial artery, and peroneal arteries.
No major artery travels in this compartment.
PATHOGENESIS
Although the exact pathophysiology is not completely understood, the syndrome is thought to be the result of either a decrease in the space available for the tissues within the fixed compartment or an increase in the size of the tissues within the compartment.
Either case can result in an increase in pressure above a critical value.
Increased fluid content and swelling of damaged muscles can be caused by the following:
Bleeding into the compartment (from fractures, large vessel injury, or bleeding disorders)
Fractures are the most common cause of compartment syndrome. It is estimated that 9.1% of tibial plateau fractures develop compartment syndrome.7
Blunt trauma is the second most common cause, accounting for 23% of cases.19
Increased capillary permeability (eg, burns, ischemia, exercise, snake bite, drug injection, intravenous fluids)
Decreased compartment size can be caused by the following:
Burns
Tight circumferential wrapping, dressings, casts
Localized external pressure, such as lying on the limb for an extended period of time or from pressure on the “well leg” in the lithotomy position on the fracture table
Elevated pressure prevents perfusion of the tissue from the capillaries and results in anoxia and necrosis.
The impermeable fascia prevents fluid from escaping, causing a rise in compartment pressure, such that it exceeds the pressure within the veins, resulting in collapse of the veins or an increase in venous pressure.22
The final event is cellular anoxia and necrosis.24
During necrosis, an increase in intracellular calcium concentration occurs, coupled with a subsequent shift of water into the tissue, causing the tissue to swell further, adding to the pressure.12 This “capillary leakage” adds to the increased pressure in the compartment, thus creating a vicious cycle. Lindsay et al17 reported that prolonged ischemia of the muscle results in adenosine triphosphate breakdown and that the amount of energy depletion during ischemia determines the extent of the ischemic damage.
The effects on muscle and nerve function are time-dependent.
Prolonged delay results in greater loss of function.
Red muscle fibers (eg, anterior compartment of the leg), which rely predominantly on aerobic metabolism, are far more vulnerable to ischemia than “white” muscle fibers (eg, gastrocnemius muscle), which rely on anaerobic metabolism.14
The exact pressure at which change within the compartment occurs has been the subject of debate and has evolved over time.
Initially, the pressure of 30 mm Hg was reported to be the maximum pressure above which irreversible muscle damage occurred.40
Currently, clinicians have recognized the importance of the patient’s blood pressure when considering the compartment pressure and use an absolute difference between diastolic blood pressure and compartment pressure of less than 30 mm Hg as an indicator of ACS.18
Animal studies have highlighted the importance of the systemic pressures relative to the compartment pressure.
Whiteman and Heckman40 found that irreversible ischemic changes occurred when the compartment pressure was elevated within 30 mm Hg of the mean arterial pressure and within 20 mm Hg of the diastolic pressure.
Research4 on limb ischemia at the University of Pennsylvania led to similar conclusions. Bernot et al4 coined the term delta P, referring to the difference between the mean arterial pressure minus the compartment pressure, with a lower number reflecting less blood flow. The authors4 found that cellular anoxia and death occur with pressure within 20 mm Hg of the mean arterial pressure; however, at pressures within 40 mm Hg, oxygen tension was reduced, but anoxia was not indicated and aerobic metabolism persisted.
McQueen et al18 used the cutoff of compartment pressure within 30 mm Hg of the diastolic blood pressure as a fasciotomy threshold. No adverse clinical outcomes occurred as a result of not releasing compartments with pressures that were more than 30 mm Hg from the diastolic blood pressure, and this has come to be the value currently used most often as a threshold for compartment syndrome.
NATURAL HISTORY
The outcome of compartment syndrome depends on location, trauma to the tissue, and time to intervention.
Six hours of ischemia currently is the accepted upper limit of viability. Rorabeck and Macnab31 reported almost complete recovery of the limb function when fasciotomies were performed within 6 hours of the onset of symptoms.
Muscle undergoes irreversible change after 8 hours of ischemia, whereas nerves can incur irreversible damage in 6 hours.10
Compartment syndrome can have broad effects on multiple systems.
As muscle necrosis occurs, myoglobin, potassium, and other metabolites are released into circulation.
As a result, several metabolic conditions can arise, including myoglobinuria, hypothermia, metabolic acidosis, and hyperkalemia. In turn, these biochemical phenomena can cause renal failure, cardiac arrhythmias, and, potentially, death.
PATIENT HISTORY AND PHYSICAL FINDINGS
Diagnosis of compartment syndrome is a clinical challenge, and significant variation among clinicians likely exists.25 Studies of diagnosis in patients are limited by lack of a reliable gold standard other than “fasciotomy was performed,” which is what typically is used in the literature.
Compartment syndrome is, for the most part, still a clinical diagnosis. However, the use of physical examination findings to diagnose compartment syndrome has not been well validated.38
The key to successful handling of compartment syndrome is early diagnosis and treatment. Therefore, the orthopaedic surgeon must be familiar with the risk factors and signs and symptoms of the diagnosis, obtain a detailed documented history, and perform a thorough physical examination.
Risk Factors for Compartment Syndrome
The patient’s history is critical. Certain aspects of the patient’s history render the syndrome more likely.
Risk factors for compartment syndrome include age younger than 35 years, male gender, and mechanism of sport injury.19, 26, 43
The most common cause of ACS is fracture, and the second most common cause is soft tissue injury.
Tibial fractures are associated with a high rate of compartment syndrome, with rates for shaft fractures ranging from 1% to 11%.25, 38 Proximal tibial fractures are at particular risk, especially high-energy tibial plateau fractures, with rates of approximately 15% to 28%3, 9, 33 and fracture-dislocations reported to be as high as 53%.20, 36 Ballistic proximal fibular fractures20 also have been shown to be at particular risk for developing compartment syndrome.
It should be noted that open fractures can still develop ACS, and some authors have found no difference in incidence of ACS with open compared with closed fractures.18, 19
The existence of any of the following characteristics should heighten the surgeon’s suspicion: high-energy injury mechanism, a patient receiving anticoagulation medication, or a patient with a tight circumferential dressing.
Physical Examination of Acute Compartment Syndrome
Little rigorous data exist regarding the validation of clinical examination findings. The most widely cited review of the literature on this topic includes only four patients with compartment syndrome.38
The classic “Ps” taught in medical schools (pain out of proportion, pain with passive range of motion, paresthesias, pulselessness, pallor, paralysis, and pressure on palpation) for diagnosing compartment syndrome are not equally useful, and little validation work has been conducted.38
Pain out of proportion to the injury is a classic symptom of the diagnosis. Patient injury severity and perception and expression of pain vary substantially, rendering this judgment difficult in clinical practice. The amount of pain medicine needed by the patient is a useful predictor of compartment syndrome in a pediatric setting.2
Patients in whom pain might be difficult to ascertain include those with head injuries; those using ethanol or drugs; those who are intubated or sedated; those who have major distracting injuries, such as long bone fracture; those receiving large amounts of pain medicine; and those with any other factor that might alter the patient’s ability to accurately sense and communicate pain levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree