Metal-on-metal total hip replacements (THRs) and hip resurfacings are coming under increasing scrutiny in light of concerns that they fail because of high wear and elevated metal ions. The aim of this study was to investigate the modes of failure in a collection of 433 metal-on-metal THRs and hip resurfacings and to examine the correlations between the reasons for revision and a range of patient and implant variables considered relevant to implant wear.
Modern metal on metal hip replacement bearings are often seen as a durable option for younger patients because they are stronger and considered to produce lower rates of wear and osteolysis. The use of metal-on-metal bearings has increased since the introduction of large-diameter components for hip replacements and hip resurfacings, which offer protection against dislocation. Consequently, metal-on-metal bearings are reported to be second in popularity to polyethylene-on-metal bearings. However, concerns remain regarding the potential biologic reactivity and long-term effects of cobalt-chromium alloy metal particles and ions, particularly in light of recent reports of soft tissue masses, necrosis, and systemic effects of elevated ion levels. Although the incidence of these problems is thought to be relatively low, there have been calls to severely limit the use of metal-on-metal bearings.
Our research center has collected a large number of failed metal-on-metal implants, including first-generation McKee-Farrar total hip replacements (THRs), early generation hip resurfacings (McMinn; Corin Group, PLC, Cirencester, UK and Wagner; Sulzer, Winterthur, Switzerland), and a range of contemporary large-diameter modular THRs and hip resurfacings. In 2006, we published a retrieval study of implant failure modes in metal-on-metal surface arthroplasties and reported that aseptic loosening and femoral neck fracture comprised most failures. We also reported that revision directly attributed to wear of the bearings was relatively rare.
The aim of this study was to investigate the modes of failure in a larger collection of metal-on-metal THRs and hip resurfacings and to examine the correlations between the reasons for revision and a range of patient and implant variables related to wear.
Methods
Between 1991 and 2010, 433 metal-on-metal implant retrievals were collected at the Los Angeles Orthopaedic Hospital Implant Retrieval Laboratory from 35 surgeons. Of the 433 retrievals submitted, 9 were postmortem retrievals collected as part of an institutional review board–approved willed joint donation program.
At revision, all components and periprosthetic tissues were fixed in 10% buffered formalin. The femoral resurfacing components were resected with a portion of the femoral neck, if possible. The components were then cleaned, photographed, and examined grossly.
Then, 185 femoral and 121 acetabular components were measured for wear depth using the Coordinate Measuring Machine (BRT 504, Mitutoyo, Aurora, IL, USA) using 300 to 400 points digitized over the surface of the implant. Wear was adjusted by time in vivo to calculate wear depth per year in micrometer per year for each component.
The following implant variables were analyzed: implant design or type and nominal ball diameter. The following patient variables were analyzed: patient age at implantation surgery, patient gender, time in vivo, and reason for revision. These variables were based on the revising surgeon’s clinical assessment, which prompted the revision surgery, rather than the findings based on the retrieval analysis.
The presence of adverse local tissue reactions (ALTRs) was noted by the revising surgeon, which included osteolysis and/or fluid-filled or solid masses, whereas suspected metal hypersensitivity or allergy was determined after implant retrieval and histopathologic analysis. If there was a fluid-filled or solid mass, the surgeon was asked to assess the size of the mass as small, medium, or large.
Representative pieces of periprosthetic tissue were embedded in paraffin blocks for routine sectioning and staining with hematoxylin and eosin. Each case was given a score for aseptic lymphocytic vasculitis-associated lesions (ALVAL) by one of the authors who specialize in orthopedic pathology (P.C.). The ALVAL scoring guidelines involved the assignment of points for the synovial lining integrity, inflammatory cell type and extent of tissue infiltration, and degree of tissue reorganization as a result of inflammation or necrosis, as previously described. The presumptive diagnosis of metal hypersensitivity/allergy was assigned to cases that had a high ALVAL score (8, 9, or 10 out of 10) and when other causes for the unexplained pain, such as infection or excessive wear, were excluded.
In 97 cases, the radiographic variables analyzed included both cup abduction angle and cup anteversion angle measured from standard anteroposterior radiographs using the EBRA software (Einzel-Bild-Roentgen-Analysis, University of Innsbruck, Austria). In 157 cases, only the abduction angle was measured using standard anteroposterior radiographs, using the intertear drop mark to level the radiographs. Radiographs were not available for the remaining retrievals, and in some other cases, the radiographs either did not include the entire pelvis or did not allow for accurate measurement of the cup position angles.
Statistical analysis was performed using SPSS version 15 analytic software (SPSS, Inc, Chicago, IL, USA). Box plots were used to compare differences in continuous variables, followed by Wilcoxon rank sum tests to assess the associated statistical certainty.
Results
Implant Types and Reasons for Revision
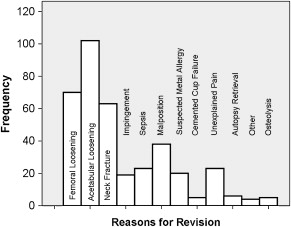
For the collection of retrievals in the present study (both THRs and conventional hip resurfacings), the most frequent reason for revision surgery was acetabular loosening (N = 102), followed by femoral loosening (N = 70) and femoral neck fracture of hip resurfacings (N = 63) ( Fig. 1 , Table 1 ). An example of a loosened acetabular component and a radiograph of a loosened femoral component are shown in Figs. 2 and 3 .
| Femoral Loosening | Acetabular Loosening | Neck Fracture | Impingement | Sepsis | Malposition | Suspected Metal Allergy | Cup Cement | Unexplained Pain | Autopsy Retrieval | Other | Osteolysis | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BHR | 21 | 8 | 8 | 3 | 4 | 20 | 10 | 0 | 7 | 0 | 0 | 0 | 81 |
| Conserve® Plus | 36 | 18 | 28 | 1 | 10 | 4 | 1 | 0 | 4 | 2 | 1 | 2 | 107 |
| McMinn | 6 | 18 | 3 | 0 | 2 | 0 | 0 | 5 | 0 | 1 | 0 | 0 | 35 |
| Cormet | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| ASR | 0 | 1 | 12 | 0 | 0 | 7 | 2 | 0 | 1 | 0 | 0 | 0 | 23 |
| Durom | 0 | 2 | 0 | 3 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 8 |
| Metasul | 2 | 19 | 0 | 5 | 2 | 1 | 3 | 0 | 4 | 2 | 1 | 0 | 39 |
| WMT THR | 2 | 16 | 0 | 3 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 24 |
| Other Resurfacing | 0 | 3 | 11 | 1 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 19 |
| Other THR | 2 | 12 | 1 | 3 | 2 | 2 | 3 | 0 | 6 | 1 | 1 | 3 | 36 |
| Total | 70 | 102 | 63 | 19 | 23 | 38 | 20 | 5 | 23 | 6 | 4 | 5 | 378 |


Most of the retrievals were of Conserve® Plus (Wright Medical Technology, Arlington, TN, USA) metal-on-metal resurfacing implants (N = 111) because this site was contracted to evaluate all retrievals in the multicenter Food and Drug Administration trial. This retrieval was followed by the BIRMINGHAM HIP Resurfacing System (BHR, N = 81) (Smith & Nephew, Inc, Memphis, TN, USA). For these 2 implants, the most commonly observed reason for revision was femoral loosening. In contrast, for the McMinn first-generation hip resurfacing arthroplasty, the Metasul THR (Zimmer, Inc, Warsaw, IN, USA), the Wright Medical conventional THRs, and other conventional THRs, acetabular loosening was by far the most frequently observed reason for revision (see Table 1 ). Among different types of resurfacing implants, the greatest number of femoral neck fractures was observed with the Conserve® Plus and the ASR (DePuy, Inc, Warsaw, IN, USA) retrievals.
Gender
Of the retrievals, 189 were from men and 201 from women. The gender was unknown in 43 deidentified retrievals. The reasons for revision were similarly distributed in both genders; acetabular loosening was the most commonly observed failure mode, followed by femoral loosening and femoral neck fracture. However, women had a higher frequency of acetabular loosening than men (60 vs 42) and a higher number of malpositioned cups that were abducted at more than 55° (30 vs 18) ( P = .19). Women were more likely than men to be assigned a prerevision diagnosis of suspected metal hypersensitivity (20 vs 3) ( P = .0004). Women had a significantly higher median cup anteversion than men (21.4° vs 13.6°, respectively; P = .05), but both genders had the same median cup abduction angle of 45°. There were 36 pseudotumors in 201 female retrievals, and 19 pseudotumors in 189 male retrievals. The incidence of pseudotumors was significantly higher in women ( P = .03).
The median femoral wear rate per year was 5.25 μm/y in men compared with 6.3 μm/y in women ( P = .3) ( Fig. 4 ). Similarly, median cup wear rate per year was 4.37 μm/y in men compared with 5.71 μm/y in women ( P = .34).
Design
It should be noted that wear was not measured in every component but, rather, was measured predominantly in those components for which high wear was suspected as a contributing cause of failure. Moreover, the distribution of wear was not normal because there were a few outliers for each type. For example, the mean femoral component wear per year in vivo was highest with the ASR, which was 19.7 μm/y, whereas the median femoral wear for the same ASR components was 8.6 μm/y ( Fig. 5 ). The smallest mean femoral wear was found with the Metasul, 5.1 μm/y, and the median femoral wear rate with the Metasul was 4.5 μm/y. In contrast, the highest mean acetabular wear was with the BHR, 19.5 μm/y, comparable with that of conventional metal-on-metal THRs, 19.4 μm/y (see Fig. 4 ). The median wear values, however, were generally below 10 μm/y, whereas the BHR and the conventional THRs had median values of 9.9 μm/y and 10.2 μm/y, respectively. It must also be noted that the conventional THRs included some older-generation designs. In general, values of wear per year were higher for the cup than for the ball ( Fig. 6 ).
Old Versus Current Designs
There were 67 early metal-on-metal resurfacing designs of McMinn, 2 of Wagner, and 167 of current-generation metal-on-metal resurfacing designs (Conserve® Plus, ASR, BHR, ReCap [Biomet, Warsaw, IN, USA], Cormet [Corin, Cirencester, England, UK], Durom [Zimmer, Warsaw, IN, USA]) in the collection. The median femoral wear rate was higher in the old design, which was 7.40 μm/y, than in the current design, which was 6.03 μm/y; however, this difference was not significant ( P = .67). The median cup wear rate was higher in the current design than in the early design (5.37 μm/y vs 2.39 μm/y, respectively; P = .12).
Pseudotumors
The femoral ball wear was higher in failures with pseudotumors, with a median of 8.00 μm/y, than in retrievals without pseudotumors, with a median of 5.25 μm/y, ( P = .057) ( Fig. 7 ). The acetabular wear was also higher in retrievals with pseudotumors, with a median wear rate of 10.02 μm/y, than in failures without pseudotumors, with a median wear rate of 4.15 μm/y ( P = .05) ( Fig. 8 ). Cup abduction was significantly higher in retrievals with pseudotumors, with a median acetabular abduction angle of 52.0°, than in those without pseudotumors, with an angle of 44.1° ( P <.001) ( Fig. 9 ). Median acetabular anteversion angle was also significantly higher in retrievals with pseudotumors (23.8°, pseudotumors; 18.9°, no pseudotumors; P = .052).
Cup Position Angles
Femoral component wear was higher in cases in which the cup was in more than 50° abduction, with a mean femoral wear rate of 21.7 ± 21.1 μm/y, than in cases in which the cup was in 30° to 50° abduction, which had a mean femoral wear rate of 5.7 ± 4.5 μm/y ( P <.001) ( Fig. 10 ). In addition, acetabular cup wear was higher in cases in which the cup was in more than 30° abduction, with a mean wear rate of 22.7 ± 41.0 μm/y, than in cases in which the cup was in 30° to 50° abduction, which had a mean cup wear rate of 9.8 ± 25.0 μm/y ( P <.001) ( Fig. 11 ).
Femoral component wear was very similar (although slightly higher) in cases in which the acetabular component was positioned at more than 25° anteversion, with a mean wear rate of 10.9 ± 12.6 μm/y, compared with cases in which the cup was in 5° to 25° anteversion, which had a mean femoral wear rate of 9.5 ± 11.0 μm/y, and this difference was not significant ( P = .6). Similarly, acetabular cup wear was higher in cases in which the acetabular component was in more than 25° anteversion, with a mean wear rate of 19.8 ± 20.8 μm/y, than in cases in which the cup was in 5° to 25° anteversion, which had a mean cup wear rate of 7.1 ± 11.0 μm/y, although the difference was not statistically significant ( P = .1).
Suspected Metal Hypersensitivity/Allergy
In cases in which metal hypersensitivity/allergy was considered to be likely based on an ALVAL score of 8 to 10, the median femoral component wear rate was 3.42 μm/y, which was significantly less than in cases in which metal hypersensitivity/allergy was considered to be unlikely, median 6.9 μm/y ( P = .004) ( Fig. 12 ). The median acetabular wear rate was smaller in the group in which metal hypersensitivity/allergy was considered likely than in the group in which it was considered not likely (2.61 μm/y vs 5.38 μm/y, respectively; P = .097).







