External Fixation of the Mature Tibia
J. Tracy Watson
DEFINITION
Indications for external fixation of the tibial shaft in trauma applications include the treatment of open fractures with extensive soft tissue devitalization and contamination. Other indications include the stabilization of closed fractures with high-grade soft tissue injury or compartment syndrome. External fixation is favored when the fracture configuration extends into the metaphyseal/diaphyseal junction or the joint itself, making other treatment options problematic.
For patients with multiple long bone fractures, external fixation has been used as a method for temporary, if not definitive, stabilization.3
With the introduction of circular and hybrid techniques, indications have been expanded to include the definitive treatment of complex periarticular injuries, which include high-energy tibial plateau and distal tibial pilon fractures.4
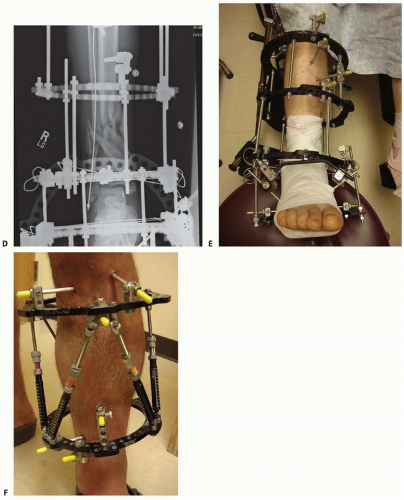
Hexapod fixators can be used to perform gradual reductions of the tibial shaft or periarticular injuries in cases of severe soft tissue injury where soft tissue coverage procedures are contraindicated and in cases of delayed presentation where acute distraction and reduction would compromise neurovascular elements12 (FIG 1F).
Contemporary external fixation systems in current clinical use can be categorized according to the type of bone anchorage used.
Fixation is achieved either using large threaded pins, which are screwed into the bone, or by drilling small-diameter transfixion wires through the bone. The pins or wires are then connected to one another through the use of longitudinal bars or circular rings.
The distinction is thus between monolateral external fixation (longitudinal connecting pins to bars) and circular external fixation (wires and/or pins connecting to rings).
Acute trauma applications primarily use monolateral frame configurations and are the focus of techniques described here.
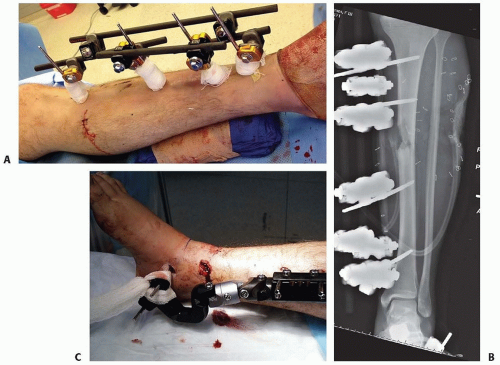
The first type of monolateral frame is modular with individual components: separate bars, attachable pin-bar clamps, bar-to-bar clamps, and Schanz pins (FIG 1A,B). These “simple monolateral” frames allow for a wide range of flexibility with “build-up” or “build-down” capabilities.
The second type of monolateral frame is a more constrained type of fixator that comes preassembled with a multipin clamp at each end of a long rigid tubular body. The telescoping tube allows for axial compression or distraction of this so-called monotube-type fixator (FIG 1C).
For diaphyseal injuries, the most common type of fixator application is the monolateral frame using large pins for skeletal stabilization.
Simple monolateral fixators have the distinct advantage of allowing individual pins to be placed at different angles and varying obliquities while still connecting to the bar. This is helpful when altering the pin position to avoid areas of soft tissue compromise (ie, open wounds or severe contusion).9
The advantage of the monotube-type fixator is its simplicity. Pin placement is predetermined by the multipin clamps. Loosening the universal articulations between the body and the clamps allows these frames to be easily manipulated to reduce a fracture.
Many high-energy fractures involve the metaphyseal regions, and transfixion techniques using small tensioned wires are ideally suited to this region. They have better mechanical stability and longevity than traditional half-pin techniques.
Small tensioned wire circular frames or hybrid frames (frames using a combination of large half-pins and transfixion wires) can be useful in patients with severe tibial metaphyseal injuries that occur in concert with other conditions such as soft tissue compromise or compartment syndrome or in patients with multiple injuries (FIG 1D,E).
Hexapod fixators are ring fixators consisting of six distractors and 12 ball joints which allow for 6 degrees of freedom of bone fragment displacement. By adjusting the simple distractors, gradual three-dimensional corrections or acute reductions are possible without the need for complicated frame mechanisms (FIG 1F).
ANATOMY
The bulk of the tibia is easily accessible in that most of the diaphyseal portions are subcutaneous.
The hard cortical bone found in this location is ideally suited to the placement of large Schanz pins, which achieves excellent mechanical fixation.
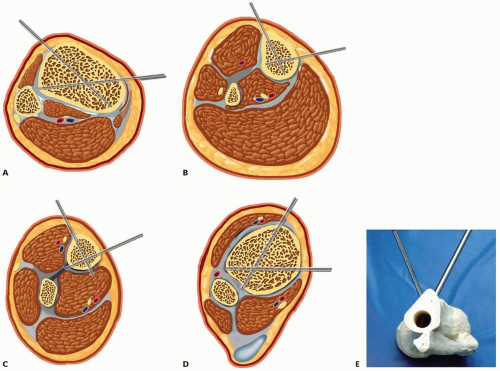
The cross-sectional anatomy of the diaphysis and the lateral location of the muscular compartments allow placement of half-pins in a wide range of subcutaneous locations. This facilitates pin placement “out of plane” or divergent to each other, which helps achieve excellent frame stability (FIG 2).
The proximal and distal periarticular metaphyseal regions of the tibia are also subcutaneous except for their lateral surfaces. The bone in these locations is primarily cancellous, with thin cortical walls.
The mechanical stability achieved with half-pins depends on cortical purchase and therefore may not be adequate for fixation in this cortex-deficient region.
Excellent stability is afforded in these areas by using small-diameter tensioned transfixion wires in conjunction with circular external fixators. Metaphyseal transfixion wires can be combined with diaphyseal half-pins can be combined to produce frames for periarticular fracture fixation for complex pilon and plateau fractures.
PATHOGENESIS
Open tibial diaphyseal fractures are primarily candidates for closed intramedullary nailing, but there are occasions when external fixation is indicated.
External fixation is favored when there is significant contamination and severe soft tissue injury or when the fracture configuration extends into the metaphyseal-diaphyseal junction or the joint itself, making intramedullary nailing problematic.
The choice of external fixator type depends on the location and complexity of the fracture as well as the type of wound present when dealing with open injuries.
The less stable the fracture pattern (ie, the more comminution), the more complex a frame needs to be applied to control motion at the bone ends.
If possible, weight bearing should be a consideration.
If periarticular extension or involvement is present, the ability to bridge the joint with the frame provides satisfactory stability for both hard and soft tissues.
It is important that the frame be constructed and applied to allow for multiple débridements and subsequent soft tissue reconstruction. This demands that the pins are placed away from the zone of injury to avoid potential pin site contamination with the operative field.
Fractures treated with external fixation heal with external bridging callus. External bridging callus is largely under the control of mechanical and other humoral factors and is highly dependent on the integrity of the surrounding soft tissue envelope. This type of fracture healing has the ability to bridge large gaps and is very tolerant of movement.
Micromotion with the external fixator construct has been found to accentuate fracture union. It results in the development of a large callus with formation of cartilage due to the greater inflammatory response caused by increased micromovement of the fragments.
There appears to be a threshold at which the degree of micromotion becomes inhibitory to this overall remodeling process, however, so hypertrophic nonunion can result from an unstable external frame.
Temporary spanning fixation for complex articular injuries is used routinely. The ability to achieve an initial ligamentotaxis reduction substantially decreases the amount of injury-related swelling and edema by reducing large fracture gaps.
It is important to achieve an early ligamentotaxis reduction: A delay of more than a few days will result in an inability to disimpact and adequately reduce displaced metaphyseal fragments with distraction alone.
Once the soft tissues have recovered, definitive open reconstruction can be accomplished with relative ease as the operative tactic can be directed to the area of articular involvement.13
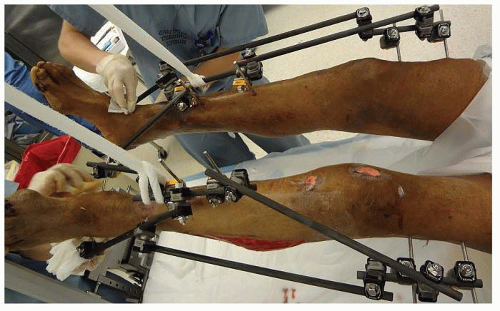
Application of these techniques in a polytrauma patient is valuable when rapid stabilization is necessary for a patient in extremis. Simple monolateral or monotube fixators can be placed rapidly across long bone injuries, providing adequate stabilization to facilitate the management and resuscitation of the polytrauma patient (FIG 3).
NATURAL HISTORY
The stability of all monolateral fixators is based on the concept of a simple “four-pin frame.”
Pin number, pin separation, and pin proximity to the fracture site, as well as bone bar distance and the diameter of the pins and connecting bars, all influence the final mechanical stability of the external fixator frame.1
Large pin monolateral fixators rely on stiff pins for frame stability. On loading, these pins act as cantilevers and produce eccentric loading characteristics. Shear forces are regarded as inhibitory to fracture healing and bone formation, and this may be accentuated with pins placed in all the same orientation.
After stable frame application, the soft tissue injury can be addressed. Once the soft tissues have healed, conversion to definitive internal fixation can be safely accomplished. In some cases, the external device is the definitive treatment. Dynamic weight bearing is initiated at an early stage once the fracture is deemed stable.
In fractures that are highly comminuted, weight bearing is delayed until visible callus is achieved and sufficient stability has been maintained. As healing progresses, active dynamization of the frame may be required to achieve solid union.
Dynamization converts a static fixator, which seeks to neutralize all forces including axial motion, and allows the passage of forces across the fracture site. As the elasticity of the callus decreases, bone stiffness and strength increase and larger loads can be supported.7 Thus, axial dynamization helps to restore cortical contact and to produce a stable fracture pattern with inherent mechanical support.2 This is accomplished by making adjustments in the pin-bar clamps with simple monolateral fixators or in releasing the body on a monotube-type fixator.
Bony healing is not complete until remodeling of the fracture has been achieved. At this stage, the visible fracture lines in the callus decrease and subsequently disappear. The fixator can be removed at this point.
PATIENT HISTORY AND PHYSICAL FINDINGS
History should focus on the mechanism of injury.
Determining whether the injury was high energy versus low energy gives the surgeon an idea of the extent of the soft tissue zone of injury and will help determine the possible location of fixation pins.
Determining the location of the accident is helpful in cases of open fracture (ie, open field with soil contamination vs. slip and fall on ice and snow).
These parameters give the surgeon an idea as to the extent of intraoperative débridement that might be required to cleanse the wound and the necessary antibiotic coverage for the injury.
The neurovascular status should be documented, specifically the presence or absence of the anterior and posterior tibial pulses at the ankle.
A weak or absent pulse may be an indication of vascular injury and may dictate further evaluation with ankle-brachial indices, compartment pressure evaluation, or a formal arteriogram.
Evaluation of compartment pressures is often indicated in open fractures and closed high-energy fractures with severe soft tissue contusion.
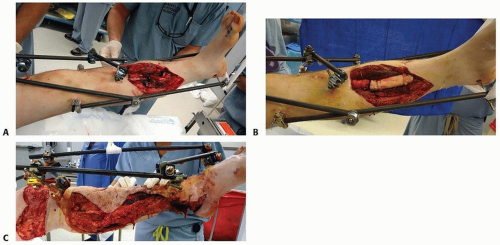
Evaluation of soft tissues and grading of the open fracture with regard to the size, orientation, and location of the open wounds aid in decision making about pin placement and the configuration of the fixator to allow access to open wounds (FIG 4).
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging of the tibia should include at least two orthogonal views, anteroposterior and lateral.
Radiographs of the knee and ankle are necessary to evaluate any articular fracture involvement or associated knee or ankle subluxation or dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree