Abstract
Introduction
It is essential to provide complete information to patients using non-steroidal anti-inflammatory drugs (NSAIDs) because of the risk of side effects. Today, most healthcare professionals recommend and privilege oral information regarding NSAIDs.
Objective
Evaluate the impact of three standardized NSAIDs information-delivery modalities on knowledge, anxiety and satisfaction of patients hospitalized in a Physical Medicine and Rehabilitation unit for debilitating and degenerative locomotor diseases.
Method
Randomized prospective study with an alternate month design. Two control groups were provided with only one type of information modality: written (information sheet) or oral (presentation). The intervention group received both modalities of information. The information included: the definition of NSAIDs, advantages and side effects, and practical advice regarding proper use. The main evaluation criterion was knowledge progression assessed by a specific questionnaire. Secondary criteria were anxiety evolution (STAI-Y questionnaire) and satisfaction related to the information delivered.
Results
One hundred and forty patients were included. Knowledge was improved in the three groups, with a greater score improvement in the group that received both modalities ( P = 0.05). No intergroup difference was noted on anxiety or satisfaction.
Discussion and conclusion
Associating both information-delivery modalities (written + oral) contributes to improving knowledge but does not seem to have an impact on the anxiety of patients treated with NSAIDs for their degenerative locomotor disease. Using standardized information sheets with a validated content could help pharmacists in their role as healthcare education provider and effectively complement the information delivered orally.
Résumé
Introduction
L’information des patients utilisant des anti-inflammatoires non stéroïdiens (AINS) est indispensable, en raison du risque d’effets indésirables. Le mode oral est actuellement recommandé et privilégié par la majorité des professionnels de santé.
Objectif
Évaluer l’impact de trois modalités d’information standardisée concernant les AINS sur les connaissances, l’anxiété et la satisfaction de patients hospitalisés dans un service de médecine physique et de réadaptation pour prise en charge de pathologies locomotrices dégénératives invalidantes.
Méthode
Étude prospective randomisée de type alternate month design . Le groupe témoin recevait l’information sous un seul mode : écrit (fiche) ou orale (exposé). Le groupe intervention recevait l’information selon les deux modalités. L’information contenait la définition des AINS, leurs effets bénéfiques et indésirables, et des conseils pratiques d’utilisation. Le critère principal d’évaluation était l’évolution des connaissances, déterminées par un questionnaire spécifique. Les critères secondaires étaient l’évolution de l’anxiété (questionnaire STAI-Y) et la satisfaction liée à l’information reçue.
Résultats
Cent quanrante patients ont été inclus. Les connaissances étaient améliorées dans les trois groupes, avec une variation du score supérieure dans le groupe ayant reçu les deux modalités associées ( p = 0,05). Il n’y avait pas de différence intergroupe sur l’anxiété, ni sur la satisfaction.
Discussion et conclusion
L’association de deux modes d’information (écrit + oral) contribue à améliorer les connaissances mais ne semble pas influencer l’anxiété des patients traités par AINS pour une pathologie locomotrice dégénérative. L’utilisation de fiches d’information standardisées au contenu validé, pourrait aider les pharmaciens dans leur rôle d’éducateur de santé en complétant efficacement l’information orale.
1
English version
1.1
Introduction
International scientific organizations recommend an integrated approach of pharmacologic and nonpharmacologic therapies for optimal care of patients with osteoarthritis . Overall, pharmacologic options are the same, regardless of the affected area . Paracetamol (acetaminophen) in oral administration remains the first-line treatment for mild to moderate arthritic pain . When pain relief is not adequate or when faced with severe pain/and or an inflammatory component another pharmacologic treatment should be considered. In this case, non-steroidal anti-inflammatory drugs (NSAIDs) are the primary alternative option . In patients with symptomatic arthritis, the lowest effective dose should be used for NSAIDs and for the shortest possible duration. NSAIDs remain one of the most used and prescribe drugs in the world. In France, they amount to 3.6% of prescriptions in general practice . They are among the most used over-the-counter products for self-medication, essentially for their analgesic properties . However, NSAIDs have several side effects. They are linked to at least 2000 to 2500 deaths annually in countries like France or Great Britain . Severe complications, i.e. affecting the digestive tract, skin and mucous membranes as well as renal or cardiovascular functions, (especially with coxibs) can mostly be avoided by respecting the published recommendations for good practices. Because NSAIDs are so commonly used for self-medication, they are one of the leading causes of iatrogenic adverse events . In a study directed in a rheumatology department, Berthelot et al. reported that patients were not well informed on how to safely use NSAIDs, and unveiled the poor educational value of fact sheets provided with the medications. Thus, if patients were better educated on the proper use of NSAIDs, they would be more cautious and thus limit the onset of adverse events related to improper use.
The objective of our study was to educate patients on NSAIDs using different types of information-delivery modalities and evaluate their impact on knowledge and anxiety of patients hospitalized for osteoarthritis as well as patients’ satisfaction regarding the way the information was delivered to them.
1.2
Population and method
1.2.1
Population
Inclusion criteria were: patients hospitalized for debilitating degenerative locomotor disease taking or having taken NSAIDs. Exclusion criteria were: age above 70 years, inflammatory rheumatoid arthritis, major cognitive disorders and poor written and oral comprehension of the French language.
1.2.2
Study site
The study was conducted within the inpatient and outpatient services of the PM&R unit of the Montpellier University Hospital Lapeyronie, specialized in the care management of degenerative diseases of the locomotor system.
1.2.3
Evaluation criteria
The main evaluation criterion was the patients’ level of knowledge regarding NSAIDs one week after having received the information. Secondary criteria were anxiety and satisfaction of patients regarding the information received. This choice was made based on the common use of these criteria in this type of study .
To determine the level of knowledge, in the absence of any questionnaires validated in the French language, we used a multiple choice questionnaire developed in a preliminary validation study on NSAIDs information sheets . This questionnaire was derived from the French translation of the one designed by Pope et al. in the English language . It includes 15 single-choice questions, covering accepted general data on NSAIDs, therapeutic effects, most common drug interactions as well as adverse side effects. A score between 0 and 15 (0 = no knowledge; 15 = maximum knowledge) is obtained by adding-up the points attributed to each answer (right answer = 1, wrong answer = 0, no answer = 0). Anxiety was assessed using the State-Trait Anxiety Inventory Form Y (STAI-Y) developped by Spielberger. This scale is validated in French and has been widely reported in the literature . The STAI-Y form includes two distinct scales including 20 items each, anxiety-state (sensitive indicator of changes in transitory anxiety) and trait-anxiety (evaluates the usual anxiety state). For each item, subjects needed to indicate their answers on a 4-point interval scale. Answers were rated as: almost never = 1, sometimes = 2, often = 3 and almost always = 4. The values obtained with this questionnaire are comprised between 20 (no anxiety) and 80 (maximum anxiety).
Satisfaction was assessed with a questionnaire that included four items selected from a previously validated questionnaire designed to evaluate satisfaction after spinal steroid injections . This questionnaire covered the following areas: patient’s satisfaction regarding the information delivered on the relevance and advantages of NSAIDs, their adverse side effects, how to behave when faced with certain negative side effects and NSAIDs benefit/risk ratio. For each item, the evaluation was conducted with a 4-point interval scale: not satisfied at all, not satisfied, rather satisfied, very satisfied.
1.2.4
Study protocol
1.2.4.1
Randomization
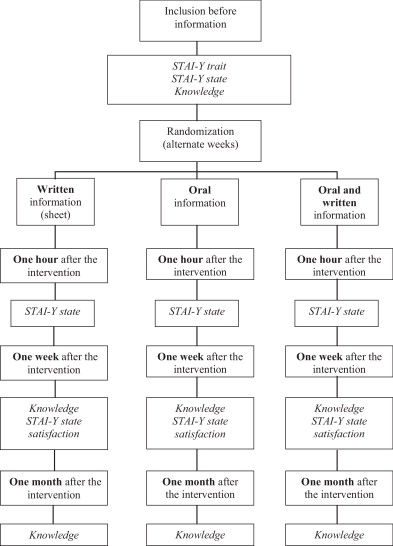
The study was conducted according to the methodology for controlled, randomized prospective studies with an alternate month design [28] corresponding to alternate-week time periods over the course of 9 months, according to the following protocol: written/oral/written + oral/written/oral/written + oral ( Fig. 1 ). An intervention-free interval was respected between each alternate-week period in order to avoid contaminating the information delivered between each group. The study could not be conducted in double-blind mode, since the modality of the information was obviously known by the person delivering this information. However, patients were not aware of which group they were included in.
1.2.4.2
Intervention
The intervention included one information intervention: written fact sheet, oral presentation or an association of both. The written information consisted in a standardized fact sheet on NSAIDs, according to the HAS (French Higher Authority on Health) recommendations on patient information forms and validated during a preliminary study . The physician in charge of the patient would hand out the sheet after the inclusion visit; the reading time took about 15 minutes. Oral information was delivered in education group sessions lasting from 10 to 15 minutes. The various aspects of NSAIDs treatment were presented to patients using a slide show. All the informative aspects delivered during the oral presentation were included in the fact sheet. The patient could, at any time, ask questions. The dual information modality consisted in patients attending the oral presentation and being handed out the fact sheet at the end of the session.
1.2.4.3
Data collection
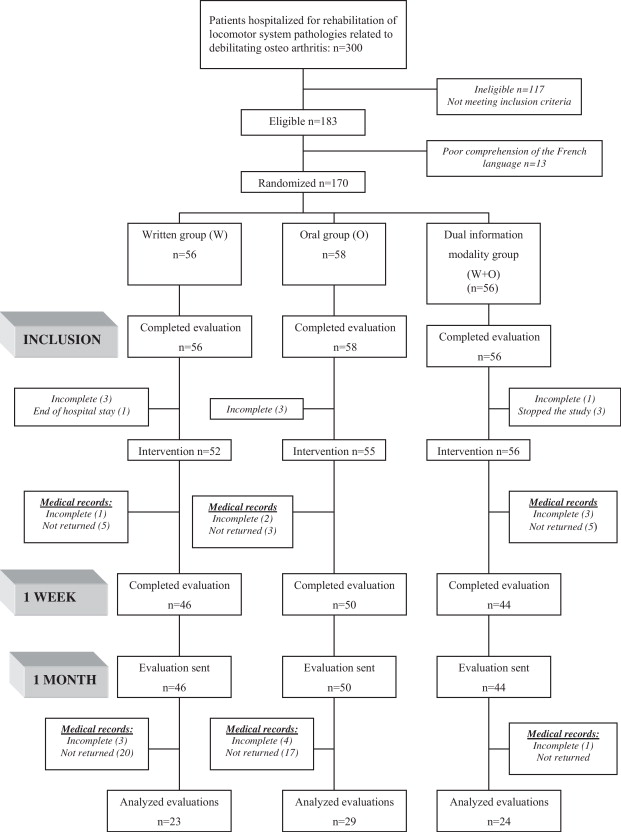
Demographics were collected upon admission in the PM&R unit. Measures of initial knowledge and anxiety were conducted after the inclusion visit. A second anxiety measure was performed one hour after the intervention One month after patients were discharged from the PM&R unit, a final measure of knowledge was conducted by mail, with phone follow-up when no answers had been received to the mailed questionnaire ( Fig. 1 ).
1.2.5
Patient consent
Since the study was not physically or psychologically invasive and in the absence of formal evidence of the superiority of one kind of information modality, an oral consent was collected before study inclusion and after the patient was informed on the study design and protocol. The study was conducted according to good clinical practices and the principles of the declaration of Helsinki.
1.2.6
Number of subjects needed
The sample size was computed with PASS software for Windows ® , taking into account a minimal clinically relevant 5-point difference on the knowledge questionnaire (minimum = 0, maximum = 15) and a 3-point standard deviation . Using a one-way analysis of variance (Anova), a total sample size of 66 subjects (22 in each of the three groups) could reach the statistical power of 91% to detect a 5-point difference, using the Bonferroni correction test for multiple comparisons with a significance level set at P = 0.05. Anticipating a 50% proportion of subjects who could refuse and/or become lost to follow-up, we chose to recruit 132 patients.
1.2.7
Statistical analysis
All analyses were conducted with the NCSS 2000 program for Windows. Quantitative variables were described using mean and standard deviation (SD). Qualitative variables were described using raw data and percentages. For analyses comparing the three different information modalities, we used for quantitative data, the one-way Anova followed by the Bonferroni correction test in case of significant interaction; and a Chi 2 test with Yates’ correction for continuity to compare percentages. To test the impact of a single information modality (oral or written) compared to a dual information modality (oral + written), comparison of means was done with the Student- t test and comparisons of qualitative variable with a Chi 2 test.
1.3
Results
1.3.1
Study description
During the 9 months of the study, 450 patients were hospitalized in the main Physical Medicine and Rehabilitation unit, including 300 for care management of locomotor pathologies ( Fig. 2 ). Among these 300 patients, 117 did not meet the inclusion criteria, 13 were not included due to their poor understanding of the French language and 30 were excluded for technical reasons (problems with data collection during their hospital stay). A total of 140 patients were included in the study: 46 in the W group received written information consisting in a standardized fact sheet, 50 patients in the O group received oral information and 44 patients in the W + O group received both information-delivery modalities, written and oral.
1.3.2
Comparing the impact of the various information-delivery modalities
Upon admission, we did not unveil any significant difference between the three groups regarding demographics and clinical data ( Table 1 ). The level of knowledge upon admission was similar in all groups. Furthermore, scores were high for baseline anxiety and immediate anxiety, without any significant difference between the groups.
| Group W 46 subjects | Group O 50 subjects | Group W + O 44 subjects | Intergroup difference | |
|---|---|---|---|---|
| Age (m ± SD) | 46.24 ± 12.78 | 49.52 ± 9.25 | 49.34 ± 11.63 | NS |
| Sex F/M | 17/29 | 31/19 | 28/16 | NS |
| Is taking/took NSAIDs | 18/28 | 17/33 | 18/26 | NS |
| Education level | ||||
| Primary school | 6 (13.04%) | 5 (10%) | 10 (22.74%) | NS |
| Secondary school | 10 (21.74%) | 19 (38%) | 16 (36.36%) | NS |
| High school diploma | 17 (36.96%) | 14 (28%) | 10 (22.73%) | NS |
| Upper education | 13 (28.26%) | 12 (24%) | 8 (18.18%) | NS |
| Knowledge (m ± SD) | ||||
| [0→ 15] | 6.35 ± 2.56 | 6.48 ± 3.04 | 5.59 ± 3.05 | NS |
| Anxiety (m ± SD) | ||||
| Baseline [20→80] | 47.06 ± 5.04 | 47.52 ± 5.6 | 46.57 ± 4.72 | NS |
| Immediate [20→80] | 49 ± 4.22 | 48.9 ± 4.13 | 48.84 ± 4.94 | NS |
Upon admission to the hospital the patients’ level of knowledge on NSAIDs was low, without any intergroup difference: 6.35 ± 2.56 points for the W group, 6.48 ± 3.04 points for the O group and 5.59 ± 3.05 points for the W + O group. Improvement of knowledge between the score at one week and the score upon admission was statistically significant for the entire population ( P < 10 −6 ), without any intergroup difference. However, the score progression was one point higher in the W + O group that received the association of both information modalities, whereas it was similar in the W and O groups with respectively 3.54 ± 3.51 and 3.56 ± 3.7 ( Table 2 ). Taking this element into account, we assembled these two groups to conduct analyzes with a higher statistical power and evaluate the impact of a single information modality (W or O) compared to dual information delivery (W + O).
| Knowledge score variation | Group W | Group O | Group W + O | Variation significance | Intergroup difference |
|---|---|---|---|---|---|
| Admission/1 week (2-1) (m ± SD) | 3.54 ± 3.51 | 3.56 ± 3.7 | 4.79 ± 3.17 | P < 10 −6 | NS |
| Admission/1 month (3-1) (m ± SD) | 3.6 ± 3.06 | 4.48 ± 3.86 | 5.42 ± 2.87 | P < 10 −5 | NS |
| Discharge/1month (3-2) (m ± SD) | –0.35 ± 1.87 | –0.17 ± 2.39 | 0.75 ± 2.52 | NS | NS |
Immediate anxiety scored high in all groups upon inclusion. Delivering the information did not increase the immediate anxiety score, regardless of the type of modality. Finally, there was no difference between groups regarding satisfaction for the information delivered.
When considering patients who received one single information modality (oral or written, n = 96) compared to those who received two types of information (written + oral, n = 44), these two groups did not exhibit any significant difference for demographics and clinical data. The level of knowledge was low with mean values at 6.42 ± 2.81 for the single information group and 5.59 ± 3.05 for the dual information group. One week after the intervention, the knowledge score increased significantly in both groups ( P < 10 −6 ), with a greater variation in the combined information group (W + O): progression of +4.79 ± 3.17 versus +3.55 ± 3.6 points for the single information group; P = 0.05 ( Table 3 ). Furthermore, the proportion of patients presenting an increase of 5/15 points or more on the knowledge score (i.e. 30% of progression, corresponding to the clinically significant minimal difference) was higher in the dual information group: 59.1% versus 38.5% in the single information group; P = 0.023) ( Table 4 ).
| Knowledge score variation | Single information group (W/O) | Dual information group (W + O) | Student- t test |
|---|---|---|---|
| Admission/1 week (2-1) (m ± SD) | 3.55 ± 3.60 | 4.79 ± 3.17 | P = 0.05 |
| Admission/1 month (3-1) (m ± SD) | 4.1 ± 3.52 | 5.42 ± 2.87 | P = 0.11 |
| Discharge/1 month (3-2) (m ± SD) | 2.42 ± 2.16 | 2.76 ± 2.52 | P = 0.08 |
| Single information group (W/O) | Dual information group (W + O) | Chi 2 | |
|---|---|---|---|
| Admission/1 week | |||
| Increase in the knowledge score by 5 points or more (Δ knowledge ≥ 5) | 37 (38.5%) | 26 (59.1%) | Chi 2 = 5.15; P = 0.023 |
| Stable knowledge score (–5 < Δ knowledge < 5) | 59 (61.5%) | 18 (40.9%) | Chi 2 = 5.21; P = 0.03 |
| Total | 96 | 44 | |
The level of immediate anxiety was high in both groups and did not significantly vary after the intervention ( Table 5 ).
| Single information group (W/O) 96 subjects | Dual information group (W + O) 44 subjects | Student- t test | |
|---|---|---|---|
| Before the intervention (1) (m ± SD) | 48.94 ± 4.15) | 48.84 ± 4.94 | NS |
| After the intervention (2) (m ± SD) | 47.98 ± 4.36 | 47.27 ± 4.15 | NS |
| Anxiety variation (1-2) (m ± SD) | –0.96 ± 4.94 | –1.57 ± 3.53 | NS |
Regarding satisfaction, regardless of the criterion studied, we did not unveil any significant difference between both groups ( Table 6 ).
| Group W (%) | Group O (%) | Group W + O (%) | Intergroup difference | |
|---|---|---|---|---|
| S1: information on the relevance and advantages of NSAIDs | ||||
| Not at all satisfied | 0 (0) | 0 (0) | 0 (0) | NS |
| Not very satisfied | 3 (6.5) | 1 (2) | 2 (4.5) | NS |
| Rather satisfied | 28 (60.9) | 38 (76) | 23 (52.3) | NS |
| Very satisfied | 15 (32.6) | 11 (22) | 19 (43.2) | NS |
| S2: information on adverse side effects | ||||
| Not at all satisfied | 1 (2.2) | 1 (2) | 1 (2.3) | NS |
| Not very satisfied | 5 (10.9) | 3 (6) | 3 (6.8) | NS |
| Rather satisfied | 23 (50) | 36 (72) | 21 (47.7) | NS |
| Very satisfied | 17 (37) | 10 (20) | 19 (43.2) | NS |
| S3: information on how to react faced with certain side effects | ||||
| Not at all satisfied | 0 (0) | 0 (0) | 1 (2.3) | NS |
| Not very satisfied | 4 (8.7) | 7 (14) | 5 (11.4) | NS |
| Rather satisfied | 25 (54.3) | 25 (50) | 19 (43.2) | NS |
| Very satisfied | 17 (37) | 18 (36) | 19 (43.2) | NS |
| S4: information on the benefit/risk ratio of NSAIDs | ||||
| Not at all satisfied | 1 (2.2) | 0 (0) | 1 (2.3) | NS |
| Not very satisfied | 2 (4.3) | 8 (16) | 5 (11.4) | NS |
| Rather satisfied | 26 (56.5) | 29 (58) | 19 (43.2) | NS |
| Very satisfied | 17 (37) | 13 (26) | 19 (43.2) | NS |
1.4
Discussion
The results from this study show that quality information with a previously scientifically validated content has a positive impact on patients’ knowledge regarding NSAIDs and their satisfaction, without any negative effects, especially on anxiety. The impact on knowledge seems higher when combining two types of information modalities (written + oral), compared to using only one of these two modalities.
The objective of our work was to compare three information modalities: written (standardized fact sheet on NSAIDs), oral (information presented during group sessions) and the combination of both written and oral information. Confronting these three information-delivery modalities seemed interesting, since studies regarding the superiority of one information modality versus another are often quite contradictory. Oral delivery of information is often privileged, since it does not require any prerequisite education level. The study by Savas et al. showed however a superiority of the written mode versus the oral mode of information for patients with very little knowledge on NSAIDs. In fact, using written supports enables patients to keep a reference document, which they can go back to at any time, whereas the oral modality relies only on immediate auditory memory . One of the limits of the written modality could be issues with reading and understanding the French language. However, Savas and Evcik showed that in spite of a low level of education, patients are able to understand a written document if the latter is simple and short .
A study very similar to ours was conducted on a population of English-speaking patients by Arthur et al. , comparing three different information-delivery modalities: oral, written, oral + written. The criteria studied were: knowledge, satisfaction and treatment compliance. Only the results on knowledge were highlighted, with no difference found between the modalities tested. However, this study suffered from a possible recruitment bias since it focused on patients with chronic inflammatory joint pain already treated with NSAIDs on the long term and thus aware of this therapeutic, as evidenced by the high level of knowledge at baseline. In another randomized study on 56 patients, Pope et al. did not find any significant effect on patients’ knowledge, simply evaluated on three items, when adding a written fact sheet to the oral information delivered . Given the lack of references on NSAIDs information in the literature and, to our knowledge, the absence of French-language studies, it seemed relevant to conduct this randomized prospective study on a population of subjects with different cultures suffering from debilitating osteoarthritis. We chose to include arthritis patients and to exclude patients with inflammatory joint pain to help prevent a selection bias, i.e. a higher level of knowledge at baseline.
The results of this study seem to validate the ones from Arthur et al. with the absence of significant difference between the three groups regarding the evolution of the patients’ level of knowledge. However, a more in-depth analysis of the results unveils that changes in the level of knowledge in the written (W) and oral (O) groups were similar. Our work does not highlight the superiority of one of these two information modalities, written or oral, contrarily to the results of the Savas study . The W + O group stands out with a variation in the knowledge score greater than 1 point compared to the variation seen in the other two groups. Thus, it seemed relevant to merge the two groups receiving only one single type of information, written or oral and compare them to the W + O group in order to conduct an in-depth analysis of the W + O synergy. In fact, in terms of knowledge improvement we can observe a significant difference between the group that received only one type of information (oral or written) and the group that received a combination of information modalities (oral + written). In our study, the baseline level of knowledge was assessed right upon the patient’s admission in the PM&R unit. The level of knowledge at baseline was quite low and its increase reflects the impact of the information delivered, the subject became aware of this knowledge progression. Thus, these results underline the synergy and potentiating of the two modes of information combined as first observed by Savas and as suggested by the study by Hill conducted on patients with rheumatoid arthritis .
Information has a positive impact on patient’s knowledge on the short term, but it would be interesting to understand the lastingness of that positive effect on the long term. Linne et al. reported positive effects at 3 months. Similarly, our results showed a stability of the level of knowledge one month after receiving the information, which is quite encouraging since NSAIDs are usually used on the short term in the studied population. This element could contribute to a safe use of the medicine.
One of the limiting factors to information delivery is its potential anxiogenic effect . Our results show that regardless of the modality of information delivery, receiving detailed information on NSAIDs was not anxiogenic. Our results are in accordance with the ones of Coudeyre et al. on the use of written fact sheets delivered to patients before spinal steroid injections. Other studies even unveiled a significant decrease in patients’ anxiety after having received the information .
We found a high level of satisfaction since 85% of patients reported being satisfied or very satisfied, regardless of the information-delivery modality and the criterion studied. These results are similar to the ones reported by Gibbs et al. and George et al. with respectively 87% and 86% of satisfaction rates. Patients are also very satisfied regarding information on adverse side effects, since it meets their expectations. In fact, McGaughey mentions in his study that 70% of patients want to be informed on all potential treatment complications. This element can help explain the low level of satisfaction they obtained in their study, since the information on postoperative complications was deemed insufficient.
Our study suggest the superiority of a dual information delivery as already underlined by other studies without being able to validate it . This dual mode has the advantage of offering a support to help memorize the information and arouse a dialog which is nowadays essential between health professionals and patients. Nevertheless, it is difficult to know if this improvement of knowledge is related to the synergic effect of the two modalities of information or if it is linked to longer time spent hearing and reading the information, using two different channels of communication. According to the results of our study, we could see the relevance of a larger diffusion of NSAIDs fact sheets by pharmacists, family physicians and rheumatologists as well as care facilities. Maybe in the future other tools such as CD-ROMs, which have proved their effectiveness , or Internet will positively complete the already available range of information tools . Conducting further medico-economics studies would seem helpful to underline the impact of these strategies in terms of cost-effectiveness for the society.
Finally, our work focused on a targeted population, i.e. patients with debilitating osteoarthritis diseases requiring hospitalization in a PM&R unit. This could explain in part the high level of anxiety. It is possible that these specificities had an impact on the results, and it would seem relevant to study the effects of these strategies in patients with different profiles, especially those with moderate arthritis, for whom targeted information could bring a positive impact on the natural progression of the disease and its related debilitated complications.
1.5
Conclusion
Our results suggest that a dual mode of information delivery in patients with debilitating osteoarthritis has a greater impact than a single mode of information delivery (written or oral) in terms of improving the level of knowledge on NSAIDs. Innovative strategies combining several modes of communication, and future communication tools, could be developed and it would seem important to evaluate them in terms of effectiveness on observance as well as their cost/benefit ratio.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article. Financial support : none.
2
Version française
2.1
Introduction
Les sociétés savantes internationales recommandent l’association de modalités pharmacologiques et non pharmacologiques pour la prise en charge optimale des pathologies arthrosiques . Les options pharmacologiques sont globalement les mêmes, quel que soit le site considéré . Le paracétamol reste l’antalgique oral de première intention pour le traitement des douleurs arthrosiques légères à modérées . En l’absence de réponse adéquate ou en présence de douleurs sévères et/ou d’une composante inflammatoire, un autre traitement pharmacologique doit être envisagé. Dans ce cas, les anti-inflammatoires non stéroïdiens (AINS) restent la première option alternative . Chez les patients atteints d’arthrose symptomatique, les AINS doivent être utilisés à la dose minimale efficace en évitant si possible leur prescription au long cours. Les AINS restent l’une des classes pharmacologiques les plus utilisées et les plus prescrites dans le monde. Ces produits représentent, en France, 3,6 % des prescriptions en médecine générale . Ils font partie des produits les plus utilisés en automédication, essentiellement pour leur propriété antalgique . Or, les AINS peuvent être source de nombreux effets indésirables. Ils apparaissent responsables d’au moins 2000 à 2500 décès par an, dans des pays comme la France ou la Grande-Bretagne . Les complications graves de ces médicaments, notamment digestives, cutanéomuqueuses et rénales ou cardiovasculaire (notamment pour les coxibs) sont cependant pour la plupart évitables sous réserve du respect des recommandations de bonnes pratiques. Leur emploi souvent banalisé en automédication fait en effet de cette classe pharmacologique une des premières causes d’accidents iatrogènes . Dans une enquête menée en milieu rhumatologique, Berthelot et al. ont mis en évidence une franche méconnaissance des règles de prise des AINS par les patients, et la faible valeur pédagogique des notices. Ainsi, une meilleure information des patients pourrait permettre une utilisation plus rationnelle de ces médicaments et limiter la survenue d’effets indésirables liés à leur mauvais usage.
L’objectif de notre travail consistait à étudier l’impact de différents modes d’information concernant les AINS sur les connaissances et l’anxiété de patients arthrosiques hospitalisés, ainsi que leur satisfaction vis-à-vis du mode d’information.
2.2
Population et méthode
2.2.1
Population
Les critères d’inclusion étaient les suivants : patients hospitalisés pour prise en charge d’une pathologie locomotrice d’origine dégénérative invalidante et bénéficiant ou ayant déjà bénéficié d’un traitement par AINS. Les patients de plus de 70 ans, porteurs d’un rhumatisme inflammatoire, présentant des troubles cognitifs majeurs, une mauvaise compréhension du français parlé et écrit n’étaient pas inclus.
2.2.2
Site de l’étude
L’étude a été menée au sein des unités d’hospitalisation complète ou de jour du service central de rééducation fonctionnelle du CHU Lapeyronie à Montpellier, unités spécialisées dans la prise en charge des pathologies dégénératives de l’appareil locomoteur.
2.2.3
Critères d’évaluation
Le critère principal d’évaluation était le niveau de connaissance des patients concernant les AINS une semaine après la séance d’information. Les critères secondaires étaient l’anxiété et la satisfaction des patients vis-à-vis de l’information reçue. Ce choix a été dicté par la large utilisation de ces critères dans ce type d’étude .
Pour déterminer le niveau de connaissance, en l’absence de questionnaire validé en français, nous avons utilisé un questionnaire à choix multiples développé dans un travail préliminaire de validation d’une fiche d’information sur les AINS . Ce questionnaire était basé sur la traduction de celui utilisé en langue anglaise par Pope et al. . Ce questionnaire est composé de 15 questions à choix simple, portant sur des données générales consensuelles concernant les AINS, leurs effets thérapeutiques, leurs interactions médicamenteuses les plus fréquentes, ainsi que leurs effets secondaires. Un score entre 0 et 15 (0 = connaissances nulles; 15 = connaissances maximales) est obtenu en additionnant les points attribués pour chaque réponse (bonne réponse = 1, mauvaise réponse = 0, absence de réponse = 0).
L’anxiété était évaluée à l’aide du questionnaire STAI-Y de Spielberger échelle validée en français et largement utilisé dans la littérature . Le STAI-Y comporte deux échelles distinctes de 20 items chacune, l’anxiété-état (indicateur sensible des modifications transitoires de l’anxiété) et l’anxiété-trait (évalue l’état d’anxiété ressentie habituellement). Pour chaque item, le sujet doit indiquer sa réponse sur une échelle d’intervalle en quatre points. Les réponses sont cotées ainsi : presque jamais = 1, quelques fois = 2, souvent = 3, presque toujours = 4. Les valeurs obtenues à l’aide de ce questionnaire sont comprises entre 20 (absence d’anxiété) et 80 (anxiété maximale).
L’évaluation de la satisfaction était réalisée par un questionnaire comportant quatre items sélectionnés à partir d’un questionnaire précédemment utilisé pour évaluer la satisfaction après infiltration rachidienne de corticoïdes , envisageant les éléments suivants : la satisfaction du patient concernant l’information délivrée sur l’intérêt et le bénéfice des AINS, sur les effets indésirables, sur la conduite à tenir face à certains effets indésirables et sur le rapport bénéfice/risque des AINS. Pour chaque item, l’évaluation était réalisée à l’aide une échelle d’intervalle en quatre points : pas du tout satisfait, peu satisfait, plutôt satisfait, très satisfait.
2.2.4
Déroulement de l’étude
2.2.4.1
Randomisation
L’étude a été menée selon la méthodologie pour les études de type contrôlées, randomisées, prospective de type alternate month design qui correspond à une randomisation par période de temps alternée ( Fig. 1 ). La randomisation s’est faite par périodes de temps alternées « semaines alternées » sur neuf mois, selon le schéma suivant : écrit/oral/écrit + oral/écrit/oral/écrit + oral. Un intervalle libre d’intervention était respectée entre chaque période afin d’éviter une « contamination » du type d’information reçu entre chaque groupe. L’intervention n’a pu être réalisée selon une procédure en double insu, le type d’information délivré étant évidemment connu de la personne délivrant cette information. En revanche, le patient n’était pas au courant du groupe dans lequel il était inclus.








